LIVER HEALTH IN DOGS: OVERVIEW
1. Be alert to physical signs of liver problems: allergies, inflamed eyes, seizures, chronic anal sac problems, and digestive difficulties.
2. Consider a liver disorder as a possible contributor to the sudden onset of behavioral problems such as fearful aggression and separation anxiety.
3. Consult with a holistic veterinarian. She can diagnose liver problems, direct treatment, and assist you in planning changes in your dog’s diet.
Maryann, guardian of a young female terrier named Salsa, made an appointment for her veterinarian to spay her dog in the winter of last year. A couple of weeks after Maryann brought Salsa home from the veterinary clinic, Salsa began to vomit up her evening meal occasionally. Because Salsa exhibited her digestive upsets only once every two or three weeks, Maryann chalked the episodes up to an occasionally unsettled stomach. However, over the next few months, Salsa vomited her evening meal consistently, once every couple of weeks.
Later, Salsa began to show a growing sensitivity to loud noises, although the bangs and crashes that punctuate everyday life in a busy household were never an issue for Salsa in the past. Now she jumped and cowered when doors slammed or when Maryann dropped a pot lid on the kitchen floor. When spring arrived, Salsa became frightened of thunderstorms and hid in the clothes closet whenever a storm approached. Although Maryann’s veterinarian prescribed a mild sedative to help Salsa stay calm during a storm, Salsa remained agitated until the storm passed.
Unnerved by Salsa’s digestive problems and newly acquired sound sensitivity, Maryann decided to consult with a holistic veterinarian about these conditions. The doctor talked with Maryann about Salsa’s medical history, observed Salsa’s general demeanor in her office, and checked Salsa’s pulse and tongue. To Maryann’s surprise, the doctor advised her that she would be treating Salsa, using acupuncture and Chinese herbal combinations, for a liver disharmony.
Liver Health and Chinese Medicine
One of the main tenets of Traditional Chinese Medicine is that qi (also known as chi, and understood as life-force energy) courses throughout the body in pathways known as meridians. Each meridian follows and affects aspects of the physical systems of the body. For example, the liver meridian runs across and affects the actual liver, and travels throughout the body affecting related functions.
So, when a physical organ such as the liver is discussed, it’s implied that the organ’s associated “energy meridian” is also involved.
For this reason, a veterinarian who studies and uses Oriental Medicine may describe symptoms of different sorts of liver disease in terms of the organ’s physiological function (or dysfunction) and in terms of problems with the liver meridian’s energy flow. These problems may include an energy excess, deficiency, or imbalance.
Assaults or “insults” to any of the energetic meridians can cause a disharmony or imbalance in the organ and its associated system, which can manifest itself as a particular health problem in the dog.
Maryann’s holistic veterinarian explained that the anesthesia administered during the operation to spay Salsa probably caused an imbalance in the state of health of Salsa’s liver, the organ responsible for processing the anesthesia and eliminating it from her dog’s body. Most dogs can “right” themselves after they have experienced an assault of this kind to one of their organs, like the liver, but not always. If the imbalance is not treated, a dog may begin to display symptoms associated with a liver imbalance, such as digestive problems or certain inappropriate behavioral responses to her environment.
So, according to Maryann’s veterinarian, the disruption of the energy in Salsa’s liver, which governs certain bodily systems like her digestion, resulted in several physical and behavioral manifestations, most commonly referred to as “symptoms.” Although Salsa had received treatment to relieve her symptoms, in the form of a tranquilizer for her fearfulness, the root cause of her health condition remained unidentified and untreated.
Chinese Herbs for Liver Imbalances
Visit Dr. Chris Bessent’s website for information about Chinese herbal remedies. Holistic veterinarians prefer to meet their patients in person, but, if you do not have access to a local veterinary herbalist, you can order Chinese herbs with the guidance of an herbalist. After your dog has taken the recommended herbal combinations for several weeks, the herbalist will check on your dog’s progress and evaluate any changes in your dog’s condition. The herbalist will modify the recommended herbal remedy based upon this feedback.
Herbs that harmonize the liver generally decrease heat in the body, and are described as cooling herbs. Some herbal combinations contain minerals that calm the spirit, and some concentrate on moving fluids smoothly through the dog’s body. The following are some of the Chinese herbal combinations Dr. Bessent uses to rebalance a disharmonious liver:
| LIVER SYMPTOM | CHINESE HERBAL COMBINATION |
| Aggression | Bupleurum and Dragon Bone decoction |
| Separation anxiety | Zizyphus decoctions |
| Allergies | Coptis Relieve Toxicity decoction |
| Inflamed eyes | Gentian Drain the Fire decoction |
| Anal sac problems | Gentian Drain the Fire decoction |
| Vomiting | Rambling Powder |
| Seizures | Gastrodia and Uncaria decoction |
| Diarrhea | Coptis Relieve Toxicity decoction |
Liver Disease in Dogs Indicates Systemic Illness
Dr. Chris Bessent, a veterinarian and a certified veterinary acupuncturist and Chinese herbalist, states that a majority of the cases she sees in her Oconomowoc, Wisconsin, practice have some liver involvement at some stage in the progression of symptoms. According to Dr. Bessent, our modern world introduces many stress factors into our dogs’ lives, such as the presence of toxins in the environment, treatment with repeated vaccinations or pesticides, emotional distress from lack of attention or training, and poor quality food or water.
Although conventional western medicine is slow to recognize that an excess of stress and extremes in emotions can translate into physical problems, holistic medical professionals have acknowledged this connection for a long time. It’s clear to holistic practitioners that there is a link between toxins or stress factors experienced by a dog to disharmony in the dog’s vital organs, which, in turn, may manifest in a seemingly unrelated symptom. At issue is the fact that conventional veterinarians may treat each individual symptom by suppressing it, such as prescribing a tranquilizer for a fearful dog, but they may not address the real, root cause of the problem.
Allopathic medicine offers few solutions to heal a diseased or malfunctioning canine liver. However, holistic medicine is very effective at treating the canine liver as the root cause of disease.
The Liver’s Role in Canine Health
The liver, located centrally in the dog’s body as the link between the breathing and circulatory activities of the chest and the digestive functions of the abdomen, works hard at its many tasks. The liver manufactures blood proteins and fat, and stores energy, fat-soluble vitamins, and iron. It removes drugs, chemicals, and other unusable substances from a dog’s body, and secretes the bile needed to digest food. The liver filters the blood to keep harmful bacteria from entering other parts of the body and prepares toxic waste materials for elimination by the kidneys. The liver operates as both a storage facility and a functional organ.
When Dr. Bessent sees a dog with health or behavioral problems for the first time, she diagnoses the dog using three resources or techniques:
• The owner’s account of the behavioral or physical abnormalities experienced by the dog, along with a physical examination of the dog in her office.
• Her own observation of the dog’s behavior in her office. A “disharmony of the liver” may cause an excess of heat in a dog’s body. An animal with a liver imbalance is always moving and does not sit in one place for very long. The dog may pant, drink more than usual, and/or exhibit thickened saliva.
• A tongue and pulse diagnosis. Taking the dog’s pulse on the inside of the dog’s rear legs, the doctor may feel that the pulse is taut, like a wire, sometimes called a “liver pulse.” The dog’s tongue may be purple or red, especially at the edges, indicating an imbalance in the liver.
When a dog’s liver is in a state of imbalance, she may present one or several behavioral and/or physical abnormalities. Although, at first glance, these abnormalities appear diverse and unrelated, their root cause can be found in the liver. Once Dr. Bessent has determined that a liver imbalance is the basis of the dog’s problem, she can treat the dog to rebalance the liver and relieve the root cause of the symptoms.
Liver Disease in Dogs
Behavioral manifestations of liver problems include both angry or aggressive responses as well as fearfulness. The emotions associated with the liver are anger, irritability, aggression, and frustration. A dog may display these emotions by excessively protecting her possessions, environment, or “space,” or by snapping or nipping. She may also display fearful aggression, like suddenly attacking a harmless visitor, separation anxiety, or a fear of loud noises and storms.
In essence, the dog is not settled in her world, and her actions are not responsive to normal behavior modification techniques. Dr. Bessent explains that harmonizing the dog’s liver, the source of these behavioral manifestations, can help normalize the dog’s reactions to its environment.
The physical manifestations of a liver imbalance include allergies, inflamed eyes, seizures, chronic anal sac problems, and digestive difficulties.
A dog with liver-related allergies experiences itching, especially in her paws, abdomen, head, and face. She may be hot to the touch, have red skin, and have weeping pustules. The dog’s coat may have a heavy, or phlegmy smell. Some dogs develop “stinky” ears not caused by a bacterial infection. These allergic reactions are the result of the dog’s hypersensitive response to toxins in her environment, which disrupts the energy flow in the dog’s liver and entire body, and increases the incidence and severity of future hypersensitive reactions.
Most allergic conditions are complicated because, if the root cause of the allergic reaction is not relieved, the dog’s body develops a general tendency to overreact to environmental allergens, and the effect becomes cumulative over time. As the allergic reactions continue to cascade and escalate, they become more difficult to treat.
Frequently, conventional veterinarians prescribe antihistamines and corticosteroids (prednisone, for example) to relieve the symptoms of allergies in dogs. However, steroids have a profoundly negative effect on the liver, and may eventually cause more harm than good, as higher doses are needed as time passes to control the increasingly severe allergic reactions from the dog.
Dr. Bessent recommends addressing allergies early, as soon as they begin to emerge in a dog, especially in young dogs. She finds that it takes only a few acupuncture treatments to rebalance a dog’s liver and reverse the allergic cascade, if managed right away.
A disharmony in the liver will likely cause inflamed eyes in the dog, either alone or in combination with other symptoms, and includes the development of a chronic discharge.
Seizures often result from a liver disharmony. Epilepsy, a diagnosis often arrived at by the process of elimination, may have its root cause in a liver imbalance. Traditionally, after examining the dog’s blood tests, doctors label a seizure condition for which the cause is unknown as epilepsy.
Dogs experiencing seizures from a liver disharmony are usually older, docile, slow-moving dogs. Their coats may be dull and they may have arthritis. Often, when these dogs are vaccinated, the insult from the vaccine imbalances their liver and they demonstrate a dramatic reaction, or seizure, to the change in their health equilibrium.
Although phenobarbital may stop the seizures, it does not balance any underlying disharmony of the liver. In many cases, this condition progresses to activate other problems, such as allergies and inflammatory bowel disease. Phenobarbital will not affect the evaluation of a pulse and tongue diagnosis, so a liver imbalance can be recognized even if the dog receives the drug. And, if the dog requires phenobarbital to control her seizures after receiving acupuncture treatments and herbal remedies, the holistic treatment may enable the dog to avoid seizures with a reduced dosage of the drug, or stop the advance of the condition into other symptoms.
The liver controls the perineum, or pelvic and anal regions of the dog’s body. Chronic anal sac problems, chronic diarrhea, and bowel problems all indicate an overreaction of the liver due to an imbalanced state.
Holistic practitioners attribute many digestive problems to liver disharmony. Chronic vomiting, especially in the late evening, when the liver is most active, indicates the involvement of the liver. Dogs suffering from a liver imbalance often vomit bile, and develop a pattern of vomiting that persists for a long time. Though vomiting may not occur very often, a dog may vomit once a week or once a month, but does so consistently.
Treating Liver Disorders in Dogs
Be aware that seemingly unrelated patterns of behavior and health problems can come from the same root source, such as a liver imbalance, and the root source can be effectively treated holistically.
Provide good general health maintenance for your dog, including feeding the highest quality food possible and offering the purest water.
Provide moderate exercise for your dog on a regular basis. The liver maintains the smooth flow of blood and qi in a dog’s body, and exercise keeps the liver efficient.
Minimize the sources of frustration and emotional upset in your dog’s life.
Address health problems with a holistic veterinarian when they first occur. That’s when they are easiest to fix.
Learn acupressure techniques for use at home in preparation for a visit to a healthcare professional. Holistic support can help tip the scales in your dog’s favor at the very start of a problem.
Recognize and Minimize the Toxic Insults Sustained By Your Dog’s Liver:
Avoid elective surgical procedures that require anesthesia, or group them together. For instance, have a radiograph of your dog’s hips taken at the same time your dog receives anesthesia for a dental procedure.
Don’t overvaccinate your dog. Consider testing your dog’s titer levels to check her existing antibody levels before vaccinating her.
Minimize the use of environmental toxins, such as lawn chemicals, carpet cleaners, carpet and fabric deodorizers, and insect sprays in or near your home. Use nontoxic alternatives whenever possible.
Minimize the use of pharmaceuticals known to have a significant, negative impact on the liver, including Rimadyl and prednisone. Consider using alternative treatments, especially on young dogs, like acupuncture, Chinese herbs, and nutritional supplements like MSM (methylsulfonylmethane) or glucosamine. Use the pharmaceuticals, if needed, in your dog’s later years.
Feed Your Dog’s Liver:
Use good nutrition to help keep your dog’s liver healthy, or to help mend an imbalanced liver. Avoid feeding fatty dry foods that are difficult to digest. Generally, veterinarians suggest that a dog with liver involvement in his health problems should receive a low-fat, low-protein diet.
Feed more than once a day, preferably two (or three times for sick dogs) to manage and balance the load placed on the liver.
Choose easily digestible foods that nourish the liver and blood, such as non-oily fish, rabbit, chicken, beets, spinach, chard, kale, squash, broccoli, and cabbage.
Consult with your veterinarian about adding B-vitamins and lecithin to your dog’s diet. These nutritional substances support the liver by helping to digest fat and assisting in circulation.
The Holistic Approach to Healthy Livers in Dogs
A conventional western veterinarian will likely prescribe a pharmaceutical to suppress a dog’s symptoms, like a drug to coat and soothe an upset stomach. A holistic veterinarian like Dr. Bessent will treat a dog with acupuncture, and send the dog home with a recommended Chinese herbal remedy to rebalance the dog’s liver.
Holistic practitioners look for the root cause of a dog’s symptoms, although imbalances in one organ or system can throw off a related organ or system and create additional health problems. An imbalance of the liver manifests itself in certain ways that are distinct from the conditions manifested by imbalances of other organs and systems. For instance, swelling would most likely develop from an imbalance of the spleen, which is responsible for moving fluids through the body.
Dog owners can add adjunct measures, like nutritional support and acupressure, to the acupuncture and Chinese herbal combinations provided by holistic veterinarians to help heal or rebalance their dog’s liver.
Dr. Bessent cautions that liver imbalances are particularly difficult to harmonize in certain dogs. If a dog has what she describes as a “liver constitution,” then the dog may have a lifelong tendency to develop a liver condition as the result of any “insult” or problem elsewhere in her body. Throughout her life, her owner must work to strengthen the dog’s liver and quickly respond to an imbalanced state with proper treatment.
Older dogs, especially those with long-standing cases of liver-related problems, and who have been medicated for years with strong drugs that assault the liver, may not rebalance easily. The ultimate target for treatment success may be stabilization and the satisfactory management of liver-related conditions.
With the help of your holistic veterinarian, consider the role an imbalance of the liver may play in your dog’s health problems, and review the holistic care options available to help your dog rebalance her liver. Treatment is highly successful, and your dog’s liver will receive the support it needs to do its job for your dog.
Acupressure for Liver Problems in Dogs
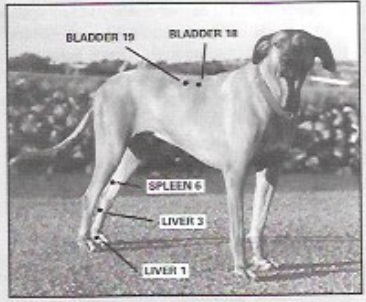
The acupressure points for the liver are located on the dog’s back and inside the dog’s hind legs, with five points on the right side of the dog’s body, and five points on the left side.
Place the dog on her side in a quiet, comfortable place in your house. Get away from high traffic areas, the television, telephone, and other potential disturbances.
Using the photo below as a guide, feel for the deepest depression under your dog’s skin and press lightly on the depression, or massage the point in a circular, counter-clockwise motion.
Continue the treatment at each point for 30 seconds to two minutes. Treat each side of your dog’s body one time.
Acupressure is easy to learn and very effective. If done correctly, your dog will fall sound asleep, signaling the arrival of qi (or life force) in her body. Even if you miss the exact acupressure point, your dog will get a wonderful massage that will relieve stress, settle her mind, and make you both feel great!
Visit your holistic veterinarian for a thorough evaluation of your dog’s health condition and potential treatments.
Lorie Long is a freelance writer living in Oriental, North Carolina with two Border Terriers, Dash and Chase. All three are addicted to agility.