Download the Full August 2010 Issue PDF
Keeping Hot Dogs Cool This Summer
It’s hot here in Northern California. And it’s just the start of a two-month annual period of the extremely high-temperature, dry weather we get here in the northeastern Sacramento Valley. I’m not crazy about it, but my dog Otto REALLY seems to hate the heat. Once the mercury hits 90 or so, he finds the coolest, darkest place he can find to hide out from the heat.
In his first summer – we adopted him in mid-June 2008 – Otto almost wore out his welcome with my husband even before his temporary ID tags had faded. The dog spent the first week digging down into any cool, moist place he could find – which happened to be under plants we were watering and inside of raised flower and vegetable beds we had painstakingly planted. Fortunately, I had been trained by the best – WDJ’s Training Editor, Pat Miller – and knew that we had a management problem, not a training issue, on our hands. I could see that Otto was just trying to get cool, so we needed to give him a “legal” place to do so.
(Why not let him in the air-conditioned house, you might ask? Because we don’t have one! We have a house, of course, just not one with air conditioning. In my office, I have what is locally known as a “swamp cooler” — more accurately called an “evaporative cooler.” It’s a powerful fan that pulls air through moist mats of aspen shavings and forces it through your home; you have to crack some windows or a door to let air escape. When it’s running Otto is welcome to join me as I work, but when I’m not in the office, he has to find other options.)
Otto’s best defense against the heat is his sandbox: it’s 4 feet by 6 feet and filled about 10 inches deep with nice clean sand, and situated in the shadiest corner of the yard. I wet the sand when I’m watering the garden in the morning, and Otto knows just how to dig a nice hole for himself and hide out in the damp sand throughout the day.
We have to alter our usual daily schedule out of deference to the heat. Throughout the rest of the year, I often take Otto along when I walk, or take my mountain bike for an afternoon ride on our abundant local trails; now, it’s just too hot for vigorous exercise at any time other than close to dawn and well after sunset. That is, too hot for a hot dog – people are still out running and riding bikes, but it’s just too hot for dogs, who are much closer to that egg-frying pavement, and barefoot to boot! We take our longest walks at night, and take more frequent, short trips to the river, where Otto loves to wade back and forth through the shallow water. (I’m hoping in this, his third summer, he finally gets comfortable with swimming. He loves the water, but only when his feet can touch the ground. When the water gets too deep for that, he looks panicky and heads for shore.)
I usually feed Otto twice a day, but in the heat, he really loses his appetite. We’ve switched to a once a day schedule, and I feed him late at night, when it’s cool. Only then will he dive into his food with gusto. When it’s hot, he just picks. OF COURSE, I make sure he’s got many sources of cool water – bowls in my office and the house, and a big bowl and a deep bucket outside. And I change the water frequently, making sure he’s got lots of incentive to drink as much as he needs.
What are you doing to keep your hot dogs cool?
When Your Dog Refuses To Walk On A Leash
It’s frustrating and embarrassing when your dog puts on the brakes and refuses to move. If he’s small you can pick him up and carry him; although that might not be the best training solution, at least it gets you out of there and you can save face. But what if it’s a Great Dane, a Newfoundland, or any breed – or combination of breeds – that’s too big to be portable? Whether your dog is giant or tiny, here are five things to do when your dog gets stuck in neutral:

288
1) Evaluate possible medical problems: Your dog may be in pain or otherwise not feeling up to par, and the last thing she wants is a jaunt around the block. If your dog refuses to move routinely, or even occasionally – not just once – it’s time for a trip to the dog doctor to look for a physical reason. You don’t want to force her to walk if she’s hurting.
2) Look for environmental aversives: Pavement gets painfully hot on warm sunny days – enough to cause considerable discomfort. Prickly weed seeds, sharp stones, sometimes even tall or wet grass can be aversive. (Dog boots can protect paws from surfaces that cause discomfort.) Maybe your dog is just hot and trying to stay in a shady spot! Be sensitive to aversive environments you can avoid; walk your dog morning and evening on very hot days. Conversely, maybe he needs a down jacket or more indoor exercise on frigidly cold winter days.
3) Consider fear issues: A temporary environmental aversive can create a negative association with the location where it occurs. Maybe your dog stepped on a bee and got stung, or a loud scary noise happened at his sticking spot. If his body language tells you he’s worried or fearful (head down, looking away, ears back, leaning back, perhaps even showing a whale eye and trembling), you’ll need to counter-condition at the place (or places) where he shows fear. (For in-depth information on counter-conditioning, see “Reducing Your Dog’s Anxieties,” WDJ April 2007.) Even better, identify specifically what causes his fear, and counter-condition that stimulus in a safer environment first, before trying it on a walk.
If he puts on the brakes as you approach the car, something about the car may be aversive. Counter-condition! Perhaps there’s a reactive dog behind a fence. If your dog gets sticky as you approach a barking, growling, berserk dog behind a fence, he may not be comfortable being barked and snarled at as you walk past. Cross the street, and then counter-condition to convince him that a snarling dog makes chicken fall from the sky, and/or arrange with your neighbors to have their dog indoors when you’re going to walk your dog.
4) Reinforce movement: If you always click and treat your dog for sitting when you stop, she may decide that stopping gets reinforced. Spend lots more time clicking for movement. If she does get stuck, avoid luring to get her unstuck, so she doesn’t learn to put the brakes on in order to get you to bring out the treats.
5) Do stuff she loves: These four tips are good for prevention and diagnosis. But what do you do in the moment, when your dog won’t move?
Do something that she loves, to get her mind off being stuck and get happy about moving. If she gets happy about targeting, play-target in a direction she is willing to move (usually back the way you came from). When she’s acting playful, target forward in the direction you want to go. Play a simple “Find it!” game, by tossing treats on the ground in the direction she’s willing to go, and then repeat the game in the other direction. Play with a ball, play tug, play any games that get her happy and moving. If it’s safe to do so, put her on a long line and run past her, fast, to the end of the line to see if she’ll chase happily after you. (Don’t use your “come” cue; do use random happy chatter).
If she gets stuck going home on walks because she’d rather stay out and have fun with you, backchain going home (start close to your front door and gradually move farther and farther away). Each time you arrive home, have a fantastic play party with her favorite toys and games so she eagerly looks forward to going home and having fun.
Pat Miller, CPDT-KA, cdbc, of Fairplay, Maryland, is WDJ’s Training Editor.
Beware of Over-Vaccinating Your Dog
VACCINATING YOUR DOG: OVERVIEW
1. Keep accurate records of your dog’s vaccination and titer history.
2. Arm yourself with accurate, credibly sourced information when having a discussion with your veterinarian about vaccine protocols.
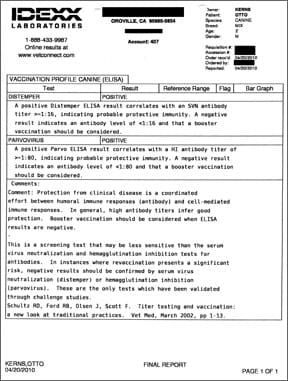
3. Consider using antibody titer tests to accurately detemine whether your dog needs to be re-vaccinated.
4. Commit to taking your dog to your veterinarian for annual checkups; consider twice-annual visits for dogs seven years of age and older.
Should you vaccinate your dog? Should your dog receive all the recommended vaccines at once? How important are common shots, like the DHPP vaccine, or rabies vaccine? Over-vaccinating dogs is a definite problem in the veterinary world, but immunizing your pet is nonetheless a necessary part of having one.
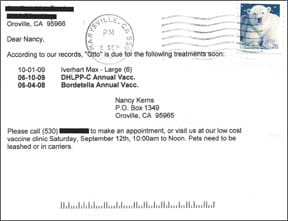
You check your mailbox and there it is: a reminder postcard from your dog’s veterinarian. If you’re like many of us dog owners, you groan and toss the card aside.
If you’ve not yet found an enlightened, up-to-date veterinarian, the postcard is likely to say, “It’s time for your dog’s annual vaccinations! Call us today for an appointment!”
We hope, however, that you’ve done your homework and found a veterinary practice whose postcards say something more like, “It’s time for your dog’s wellness examination! Call us today for an appointment!”

What’s the difference? In 2003, the American Animal Hospital Association (AAHA) revised its vaccination guidelines, recommending that vets vaccinate adult dogs only every three years – not annually. Many enlightened veterinarians changed their canine healthcare protocols to reflect the guidelines, and now suggest annual wellness examinations with vaccinations only every three years.
In WDJ’s opinion (and that of the experts we consult), annual vaccination for most canine diseases is unnecessary and potentially harmful. Dog owners should avoid employing those old-fashioned veterinarians who recommend annual vaccines. Owners should also avoid those veterinary service providers who provide inexpensive vaccines and other routine care without the benefit of a relationship with you and your dog beyond a brief transaction in a parking lot or pet supply store. While the financial cost of vaccine clinics may be appealing, the fact is, your dog’s health may pay the price of unnecessary or inappropriate vaccines.
Vaccines for Dogs: The Basics
Core vaccines protect animals from severe, life-threatening diseases that have global distribution. According to the AAHA, core vaccines that every dog should receive initially as a puppy (a series of three vaccines given between 8-16 weeks of age) are:
1. canine distemper (CDV)
2. canine parvovirus 2 (CPV-2)
3. canine adenovirus 2 (CAV)
The core vaccines should be administered one year later, and every three years thereafter, unless antibody titer test results indicate that the dog possesses antibody levels that have been determined to be protective. (For more about titer tests, see
“Dog Vaccination Information“.)
The rabies vaccine is also considered a core vaccine, but should be given once at age 12 to 16 weeks (or as late as local law allows), then again one year later, followed by every three years. (Unfortunately, some locales require rabies vaccination more frequently than every three years, so check your local laws.)
Non-core vaccinations should be administered only to dogs whose geographical location, local environment, or lifestyle place them at risk of contracting each of the specific infections. These vaccines are:
– Bordetella bronchiseptica (kennel cough) & parainfluenza
– Borrelia burgdorferi (Lyme)
– Leptospirosis
Vaccines not recommended, per 2006 AAHA Guidelines are:
– coronavirus (CCV)
– giardia
Note: The above recommendations are per the AAHA. Dr. Dodds no longer recommends the CAV vaccine, and advocates administration ofthe initial rabies vaccine after 20 weeks of age (if allowable by local law).
Be Prepared with Your Dog’s Vaccination History
That said, don’t think for a minute that you need to take your dog to the vet only every three years. It’s imperative that you take your canine companions in for yearly checkups. Rather than throw that postcard in the trash, pick up the phone and call for an appointment. Yearly wellness examinations help our veterinarians develop a good baseline on our dog’s health, be better able to take notice of subtle changes in his health over time, and develop a relationship with our dog and us.
While these annual trips to the vet might now be called “wellness checks” rather than “vaccine visits,” the odds are good that the topic of vaccines will come up. And despite our good intentions, many of us head in with our dog for his annual exam and feel blindsided as the vet suggests an array of vaccines for our dogs. Often, we nod in agreement, get that “deer in the headlights” look and agree with her recommendations (she is the expert after all), then go home with regrets.
Remember the Scout motto and “Be prepared” as you get ready for your dog’s next veterinary appointment. Being prepared means more than remembering to take your dog’s leash, collar with ID, treats, and showing up on time, on the right day, with the right dog. How to best prepare for your dog’s annual veterinary visit and be ready for a discussion on the most appropriate vaccine strategy for him?
- Bring veterinary records and/or a list with you of your dog’s vaccination history; do not assume the veterinary clinic will have all the most recent information, especially if you’ve changed clinics. Other test dates and results to bring include most recent heartworm test, antibody titer test results, and blood and/or urinalysis test results. Ideally, you’ll collect all the data ahead of time and enter into a table so that you have a timeline of the pet’s life.
My dogs’ veterinarian, Susan Wynn, DVM, recommends creating a table with vaccines/yearly wellness test along the vertical axis, with dates along the top. If visiting a new clinic, chances are they’ll want proof that your summary is accurate, so request copies of any previous vet records for your dog’s new file.
- Have a clear idea in your mind whether you want/need your dog to receive any vaccinations (and for which diseases), an antibody titer test, or none of the above. If you are unsure, cultivate a good understanding of the vaccines available. And ask your veterinarian if any particular vaccines are warranted due to conditions in the area in which you live.
- Educate yourself using reputable sources so that you can have an intelligent conversation with your veterinarian on the pros and cons of vaccination for your dog; a good place to start are the AAHA Guidelines. Writings and research by Ronald Schultz, PhD, DACVIM, and Jean Dodds, DVM, are also excellent references.
- Know the status of your dog’s health, and whether he has any health or behavioral issues that your veterinarian should be aware of.
- Bring a list of your dog’s current medications and supplements, including dose, strength, and frequency.
- Have an idea of what the visit will cost, including any tests, to avoid sticker shock or making hasty (bad) decisions based solely on price. Call ahead.
- Be prepared to take your dog and go home if you are uncomfortable with your veterinarian’s recommendations. There’s no need to get nasty or defensive. We suggest something along the lines of, “I’m not sure I’m comfortable with those recommendations. I’d like to go home and think about them.”
If you are going to see a veterinarian who is new to you and your dog, consider making an appointment with the veterinarian, without your dog, to discuss her philosophy toward vaccinations and antibody titer tests.
Educate Yourself About Vaccines
Michelle Kitzrow, of Sugar Hill, Georgia, had a change in thinking regarding vaccine protocols after hearing immunology expert Dr. Schultz speak on the topic (see “Vaccinations 101,” WDJ August 2008). Armed with a new understanding of vaccine protocols, Kitzrow took her then-four-year-old Bouvier, Casey, in to see her longtime veterinarian for Casey’s annual exam.
She admits that it “wasn’t very easy” to convince her veterinarian that, in lieu of vaccinations, Casey should receive an antibody titer test to determine whether she had what vaccination experts regard as a “protective level” of circulating antibodies from past vaccinations. But in the end, Kitzrow’s veterinarian relented, and agreed to take and send a blood sample off to a lab for the titer test.
Kitzrow believes that it was the relationship she already had established with Casey’s veterinarian, along with a new and accurate understanding of vaccines, that helped her veterinarian to support her decision. “He knows that I bring in my dogs regularly for veterinary care, and he trusts me to do the right thing. He also appreciated that I had taken the time to educate myself about vaccine protocols and titers.”
An acquaintance of mine, Diane (name changed at her request), had a bit harder time at the annual exam convincing her veterinarian to check her dog’s antibody titers instead of reflexively vaccinating – despite an 18-year relationship with her dogs’ veterinary clinic and the fact that she takes in her dogs twice a year for checkups. Diane’s 16-month-old Bouvier had received a puppy vaccine series, with the final boosters given after she was 16 weeks of age. The series included distemper, hepatitis (adenovirus), parvovirus, parainfluenza (shorthand for this combination of four vaccinations is DHPP), rabies, Leptospirosis, and Bordetella.
“At my dog’s most recent vet checkup, I requested that only the rabies vaccine be given. I asked that titers be checked for distemper and parvovirus, and I requested a SNAP 4Dx test, which checks for heartworm disease, as well as the most prevalent tick-borne diseases: ehrlichiosis, Lyme disease, and anaplasmosis.
“I declined the combo, ‘all-in-one’ vaccine for distemper, hepatitis, parvovirus, and parainfluenza, as well as the Leptospirosis and Bordetella vaccines. I did not want all of those vaccines given at the same time and hoped that the titer results would show adequate immunity. I was adamant that my dog receive only the rabies vaccine at that time. The vet marked ‘refused’ on my dog’s chart next to the other vaccines she wanted my dog to receive that day.”
Diane understands that Lepto and Bordetella need to be given at least yearly to be effective, but has made the decision not to re-vaccinate her dog for those diseases at this time and understands the risk. Dr. Wynn notes that while we as clients might consider a notation of “refused” on our dog’s chart to be judgmental on the veterinarian’s part, the reason that the vet must note in the file that the client declined vaccination is to limit liability in case the animal is infected with that disease and subsequently blames the vet. (Dr. Wynn assures me that this has happened.)
“In this particular situation, it turns out that my decision to decline all of the ‘recommended’ vaccines, except for the rabies booster, was a good choice as the SNAP 4Dx (checked in-house afterward) indicated that my dog has Lyme disease. A follow-up Lyme Quantitative C6 Antibody Test confirmed an active Lyme disease infection, which means that her immune system was already compromised at the time of the exam. The distemper and parvo vaccine titers showed adequate immunologic response, indicating that my dog was still protected against these diseases, most likely from her previous round of vaccinations.”
In fact, vaccinating a dog who has an active Lyme infection might have been harmful. “It is never wise to vaccinate a dog whose immune system is preoccupied with something else,” asserts internal medicine specialist Nancy Kay, DVM, DACVIM, author of Speaking for Spot: Be the Advocate Your Dog Needs to Live a Happy, Healthy, Longer Life. “The vaccine might ‘distract’ the immune system from the more important task at hand. Also, in theory and for the same reason, the vaccine might not be as likely to create protective immunity.”
Similar to Kitzrow, Diane finds that “Although my dogs’ veterinarian gets exasperated by the decisions I make that are counter to her recommendations, she knows that I appreciate and respect her knowledge and experience. I always ask for her advice regarding my pets’ well-being and do not hesitate to bring my pets to the hospital whenever I have concerns about their health, above and beyond checkups twice a year. She is also aware that I obtain information from a variety of other sources and that I become concerned and wary when there is a real discrepancy or controversy.
“Although she stresses the importance of following her recommendations, she has come to understand that I feel a strong sense of personal responsibility in the decisions made and their effect on the long-term well-being of my pets. If I have serious doubts about a stand that she takes, I will seek a second opinion, elsewhere. On this day, I guess you could say that we agreed to disagree.”
Diane is a little saddened that she and the veterinarian were unable to reach common ground, or at least have a more comfortable dialogue, noting, “It’s important for me to have a good rapport with the vets who care for my beloved pets. It’s important to me that they consider themselves an essential part of a team working for the well-being of the animals. Open communication and teamwork between pet owners and their veterinarians is essential.”
How Antibody Titer Tests May Affect Your Decisions
Antigens are any substance that the immune system identifies as an invader and responds to by producing a chemical defense: antibodies. When everything is working as it should, your dog’s immune system will recognize disease antigens that were introduced to his system via a vaccine (weakened or killed) or by natural exposure to the antigen that causes the disease (viral or bacterial).
A “titer” is a measurement of how much antibody to a certain antigen is circulating in the blood at that moment. The result is usually expressed in a ratio. A positive titer test result is strongly correlated with a good antibody response to either a recent infection or vaccination. A dog who has received “core” vaccines and who displays a positive antibody titer test result should be considered protected from the diseases for which he was vaccinated (meaning, he doesn’t need vaccines at that time). See WDJ blog entry, “Vaccine Titer Tests,” for more insight.
Your dog must undergo a blood draw in order to have an antibody titer test. Labs such as Antech, IDEXX, and most veterinary college laboratories offer these tests. Antibody titer testing is typically run for parvovirus and distemper, since the dog’s antibody response to these two antigens is highly predictive as to the dog’s immunologic competence in dealing with any other antigen to which he has been exposed.
Rarely, there are exceptions. When an antibody titer test is negative, the owner and veterinarian should consider revaccinating and then testing the titers again. It may turn out that the animal simply needed another exposure to the antigen in order to stimulate a stronger immune response. Or, it may develop that the dog lacks the ability to respond normally to vaccines, that is, by mounting a proper immune response. In this case, the owner and veterinarian have gained very valuable information about the dog’s compromised immune status – information they never would have gained by simply vaccinating and assuming the dog was “protected,” as is usually the case with healthy dogs.
Dr. Kay comments, “There are several reasons I can think of why a vet might be loathe to run titers, but of these, I consider only a couple of them to be ‘honorable.'” Two examples she gives are:
- Some veterinarians question the accuracy of titers in terms of accurately assessing immunity.
- If a dog is truly at a high risk of infectious disease, revaccination might be a safer bet than relying on the results of an antibody titer test. She adds, “Very few dogs are truly in this situation, such as those who live in the midst of lots of completely unvaccinated dogs and in a lower socioeconomic setting.”
When I pressed Dr. Kay on the first point, asking what information “Dr. Doe” would have that trumps information provided by someone such as Dr. Schultz, she replied, “You will get no argument from me on this. I suppose that if Dr. Doe professes that titer tests are not accurate, one could ask to see the data that leads him (or her) to this conclusion.”
Although Dr. Wynn adds, “If a distemper or parvo titer is positive, we know that the dog is protected. If it is negative, the dog might be protected, but we have no practical further test to know whether or not it is. Hence, some veterinarians have said the titer isn’t accurate to point out that we don’t know what a negative titer means.” In the case of negative titers, Dr. Schultz recommends revaccination, even though the dog could already be protected.
If You Choose to Vaccinate Your Dog
If you determine that your dog is in need of vaccination, consider the following:
- Ask the veterinarian to perform the health exam and other tests first; you might even wait to vaccinate until those results are in, and schedule a follow-up vaccine visit once you know your dog is in the clear, health-wise.
- Avoid a combination vaccine (five-in-one-type vaccinations) that offers multiple vaccines in only one shot. Note: some veterinary clinics only carry this type of vaccine. We recommend that you look elsewhere for care.
- Do not vaccinate your adult dog more frequently than every three years (unless local conditions suggest a heightened need for Lepto, Bordetella, or Lyme vaccines; these each last a year or less).
- At a minimum, try to schedule the rabies vaccine for a different visit than the other vaccines, if your dog needs them. The rabies vaccine should be administered by itself at a later date, apart from the other three “core” vaccines (distemper, parvo-virus, and adenovirus), and in another part of the dog’s body.
If you’re considering vaccinating simply for financial reasons (because vaccines cost less than running a titer test) a well-planned vaccine/titer strategy might have you coming out ahead in the long run if you scale back on vaccines and run titers on a strategically planned schedule.
Veterinary medicine today has advanced to the point of acknowledging that there is no single “perfect” vaccine program; vaccine programs must be tailored to the specific needs of each animal. Although there is a tendency to want to treat all dogs the same, the program should be designed for the individual, not the masses. The dog’s health, age, environment, activities, lifestyle, and whether he has previously had any adverse vaccine reactions all need to figure in to the equation.
If you encounter a veterinarian who continues to advocate yearly vaccination, schedule a sit-down talk with her, or take your business elsewhere. In Dr. Kay’s book, she notes that a “deal breaker” when choosing a veterinarian is when the clinician “vaccinates dogs for everything, every year.”
It’s Up to You to Make Vaccination Decisions
Don’t expect your veterinarian to ask you broadly what you want to do when you take your dog in for an annual exam. Most veterinarians, unless prompted by the client, will assume that you’re there for “the usual” and will go ahead and recommend annual vaccinations. It is up to you to educate yourself and advocate for your dog and know what vaccines and tests might benefit him, and to know the laws concerning how frequently the rabies vaccine must be administered.
If you and your veterinarian are not on the same page, try having a rational, objective discussion. Put yourself in her position and try to understand her concerns. Take a step back to be sure that what you propose is reasonable. Keep in mind that taking your dog in regularly for annual checkups will help your veterinarian to develop further trust in you and your intentions. If you’ve got a good relationship and you’re armed with the facts, you just might be able to reach common ground.
Lisa Rodier is a frequent contributor to WDJ. She lives in Alpharetta, Georgia, with her husband and two Bouviers, and volunteers with the American Bouvier Rescue League.
Comfortable Dog Cone Alternatives
ALTERNATIVES TO THE DOG “CONE”: OVERVIEW
1. Shop for a dog cone alternative before your dog’s surgery, when he’s still feeling well.
2. Have your dog “try on” several different products. Have him wear them around the store for as much time as you can afford, to see how he deals with each product’s challenges.
3. When choosing a product, take your dog’s anatomy and size into account.
4. If your dog may have to wear one of these products for an extended period of time, consider buying a couple or three, so you can find the one that works best for him.
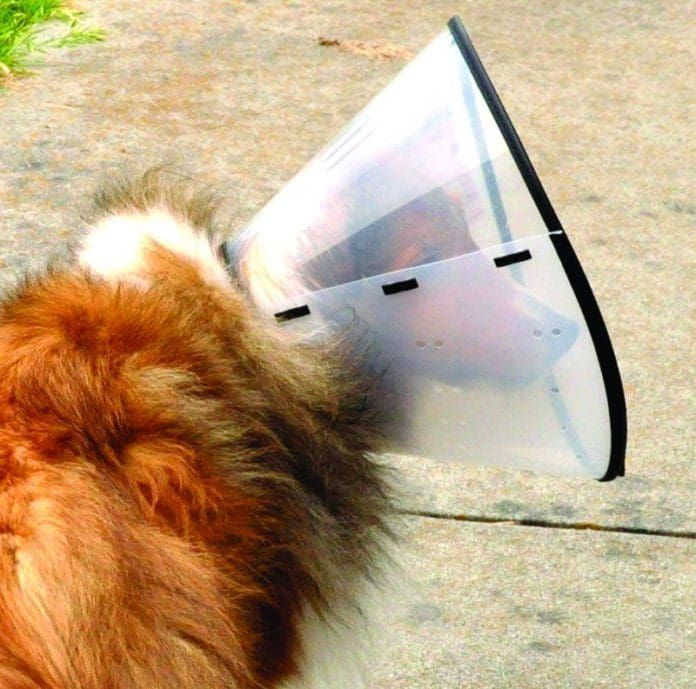
My mother once phoned me to tell me that one of our family dogs, an oversized German Shepherd, had required surgery for an embedded foxtail in one of his back paws. She told me that the vet sent her home with a gigantic plastic disc that she understood was to be put on the dog, to prevent him from licking or chewing his bandage or paw. Giggling, my mother told me, “Your father put it together…but how do I put it on the dog? I mean, is he supposed to look like a tulip or a prince?”

I could understand her confusion. The dog was so leggy that he actually could wear the Elizabethan collar either way; wearing a conventional “cone” like a “prince” would render dogs with shorter legs immobile. In contrast, most dogs have to wear these protective cones the way in which they were designed to be worn – like a dejected, bumbling tulip. Most dogs are miserable while wearing a classic, veterinary-supplied cone. Lacking peripheral visibility, they crash into furniture and doorways. With the wide, flaring cone, they get stuck in tight spots in the house.
Every dog owner should be aware that, today, there are a number of dog cone alternatives to the classic Elizabethan collars to prevent a dog from licking a wound, aggravating a hot spot, tearing out his surgical stitches, or removing a bandage. The alternatives offer a dog greater comfort, better mobility, and improved visibility.
Cons of Classic Cones
Are the classic plastic cones really all that bad? It depends on which dog you ask. Some dogs seem to accept the weight of the heavy plastic, the restricted visibility imposed by the opaque material, the need for increased clearances around the house, and even being gouged by the thick plastic tabs that are supposed to be belted by the dog’s collar at the base of the cone.
But many dogs seem to suffer more from the cones than from whatever necessitated their use! I’ve known many dogs who wouldn’t eat or drink with a cone on. I’ve seen some dogs who, after bashing into doorways and furniture, became extremely reluctant to move – or even lift their bodies or heads from the floor – as long as the cone was on.
Very recently, this very thing happened to a friend’s Shetland Sheepdog, Rickey, who had to undergo a long and complicated surgery. His surgeon removed a large (but fortunately benign) tumor that had surrounded the poor little dog’s esophagus, stomach, and other areas in his abdominal cavity, leaving a surgical scar almost the entire length of Rickey’s tummy. After a day or two of recovery in the hospital, the veterinarian sent Rickey home with a classic, heavy, opaque cone to keep him from fussing at his stitches.

Rickey’s family was delighted to have him home. But the usually spunky Sheltie seemed depressed, deflated by difficulties with his Elizabethan collar.
And so his owner called me; we had communicated about Rickey all through his long illness, diagnosis, and even the surgery. “He may be in pain from the operation,” she told me. “But honestly, I think he’s far more upset about the cone!” She asked me if I knew of anything she could do to keep Rickey from bothering his stitches . . . but without making him as miserable as he was with the cone.
If you and your dog were ever in a similar position, and you called your vet for advice, you were probably told that being quiet was good for the dog, and that it was just as well that the cone reduced his activity. There is a certain value to the advice; you certainly don’t want a post-surgical dog to race around the house. But what if he won’t even eat or drink, or fails to walk around enough to eliminate urine and feces as frequently as he should?
I knew there were dog cone alternatives to the classic cones – and that all of them are more comfortable for dogs. I also knew that WDJ hadn’t reviewed those alternatives for quite some time. So I made a list of other products designed for the same purpose as classic cones, and told my friend to buy every one that fit Rickey and give them all a try. WDJ would repay her – and take them off her hands when she was done. You know, in exchange for a little product feedback?
Glad to have something to do to help Rickey, my friend’s husband raced all over the Bay Area, picking up products in a variety of pet supply stores. The good news: While Rickey was unable to lick or chew at his sutures while wearing any of the products, he was happier (and hungrier) in every single alternative product than he was when wearing the classic veterinary-supplied cone. His legendary appetite quickly returned, as did his spunk and spark (and bark!).
Not long after Rickey had his stitches removed, he modeled all the products for my camera. I can attest that the dreaded white classic cone literally depressed the underweight (but gaining!) Sheltie. In contrast, he appeared considerably brighter with the alternatives.
Dog Cone Alternatives
ProCollar

Rickey seemed to be most comfortable wearing a product that his owners guessed he’d hate; so much for being able to tell what might work best while in the store. You really should take your dog to the store and try various models on him.
The doughnut-shaped ProCollar, distributed by G&B Marketing, of Vista, California, features an inflatable core with a durable cover. (The cover feels like vinyl – not our favorite material – but doesn’t have the distinctive “stink” of vinyl. The package doesn’t say what the material is.) A Velcro strap secures the outer perimeter of the collar; the dog’s collar is run through loops on the inside ring of the product. (One must have a collar that can be unsnapped or unbuckled; collars that slip over the dog’s head won’t work with this design.)
The ProCollar is available in five sizes (X Small to X Large). That sounds like plenty, maybe, except that 25-pound Rickey required the “large” size. Truly large dogs would not be able to use this product.
Rickey was easily able to navigate his home while wearing the ProCollar. He seemed to understand his limitations and cope with them without getting upset. Unlike his peeved response to crashing into the furniture with the stiff vet-supplied cone, Rickey barely seemed to notice when the cushioned ProCollar knocked into something. He also seemed to appreciate that when he lay down, the cushion provided him with a little pillow. Seriously! His owner thought he missed sleeping with his chin on something after his need for the ProCollar was past.
We were able to find the ProCollar in a number of chain pet supply stores (Petco and Petsmart) and catalogs, from $15 to $25, depending on size.
Soft-E-Collar

Jorgensen Laboratories, Inc., of Loveland, Colorado, offers the Soft-E-collar. It’s another cushioned collar, but this product is shaped more like a life-saving ring than a doughnut: wider and flatter. The outer material appears to be a nylon blend. A flap of material on the inner perimeter of the product is tightened by tying a cord (which runs through some grommets on the material flap) to secure the collar on the dog’s neck (see photo below).
The width (and perhaps weight) of this product made navigation a bit more difficult for Rickey; lying down was also more difficult in this collar. A larger dog may not find it as difficult as Rickey did.
The Soft-E-Collar comes in nine sizes (yay!), from XX Small (0 to 5 pounds) to XX Large (95 pounds and up). (Rickey wore a Medium, for dogs 30 to 55 pounds.) We found this product in an independent pet supply store; we also found it offered in many pet supply catalogs. As but one example: we found it for $19 to $49 (depending on its size) from BellasPainRelief.com. (By the way; this site is a great source for products for disabled dogs of all types.)
BiteNot

Here’s a dog cone alternative product with a very different design. The BiteNot collar, distributed by Bite Not Products, Inc., of San Francisco, California, resembles a neck brace for humans – the kind people have to wear after they get whiplash. The interior surface is a thinly padded foam rubber material; the outer surface is a stiff plastic shell. Velcro fasteners – and a nylon strap that wraps around the dog’s shoulders and under his armpits – hold the product very securely in place.
The BiteNot collar is available in seven sizes. In this case, the required size is determined by the length of the dog’s neck, from the back of his ears to the top of his shoulder. (It’s meant to prevent him from bending his neck enough to lick himself.) The smallest size is 3.5 inches wide; the largest is 8 inches wide.
This would be my top choice for a dog who had succeeded in removing all other products; as long as the dog has a discernible neck, it fits really securely. What if the dog is one of the (nearly) neckless breeds, like a Pug? Probably not the best pick. This worked fine on Rickey (although fastening the Velcro with all his ruff hair was a challenge), but dogs with extraordinarily long necks or wounds on their front feet might not benefit at all from the collar.
This product ranges in price from about $20 (smallest size) to $45 (largest) and is sold at several online retailers.
The Comfy Cone

The final two dog cone alternatives that Rickey tried most resemble the classic cone; each offers improvements to the concept, however.
As suggested by its name, The Comfy Cone is a cone, but instead of being stiff and unyielding, it’s cushioned and bendable. The inner material seems to be foam rubber; the outer material is a tough nylon. Numerous strips of Velcro fasteners and a ring of elastic “belt loops” (meant to be laced through by the dog’s collar) hold the cone in place.
As also suggested by its name, the product was perfectly comfortable for Rickey. He seemed unperturbed when the cushioned collar crashed into things – and it did crash, since it affords its wearer with just as little visibility as a classic cone.
The Comfy Cone is available in five sizes, from Extra Small to Extra Large. Rickey wore a Large, which was probably larger than necessary; there is a lot of overlap built in (as you can see in the photo, left), so the sizing need not be precise in order for the product to be secure.
All that is good news. The bad news? While Rickey, like most post-surgical patients, was easily deterred from licking his sutures be this product, a very determined dog (such as one who suffers from chronic hot spots), could probably turn his head with enough force to bend the walls of the cone and reach parts of his body.
We found The Comfy Cone in many online and brick-and-mortar stores, from about $10 for the Extra Small to $30 for the Extra Large.
Distributed by All Four Paws, Los Angeles, California. See allfourpaws.com for a list of retailers, or call (866) 454-7768.
Kong EZ Collar
This product is another plastic cone. So what makes it an alternative? First, the plastic it’s made of is transparent; the dog can see through it! Brilliant! This one tiny thing makes a huge difference to the dog. It’s also much lighter in weight than the vet-supplied conventional cones, though not so light that its protective rigidity is compromised. And finally, both its inner and outer edges are lined with a material that feels like vinyl. This means no stiff edges cut into the dog’s neck, and when the dog does bump into something solid, the impact is a bit blunted.
The Kong EZ Collar is distributed by the Kong Company, of Golden, Colorado, and is available in five sizes, from Small to XXL. Rickey’s owner bought the Extra Large, which was also larger than required and has a lot of size overlap built in.)
We found the Kong E-Collar in numerous online and independent pet supply stores. For example, Pet Street Mall carries them for $8 to 16; petstreetmall.com or (800) 957-5753.
Note: Cardinal Pet Care makes a very similar, transparent, light-weight cone for a very similar price. These can be found in chain stores like Petco.
How to Train Proper Leash Walking – Pull Over!
One of the more frustrating experiences for positive dog trainers is watching their clients being dragged by their dogs across the parking lot toward their cars, just moments after training class is dismissed. “Dang,” we sometimes think, “Will they ever teach their dogs to walk politely on-leash? What part of ‘Don’t reinforce your dog for pulling!’ didn’t they hear?”
Of course, it’s equally frustrating for dog owners when their dogs drag them. And the training solution – stopping every time the dog pulls – gets tiresome. Owners often wonder if they will ever be able to go anywhere without handfuls of dog treats in their pockets. In some cases, owners are actually injured when their dogs yank on their arms, or even pull them off their feet. Many dogs have their social outings severely restricted, simply because their owners have difficulty controlling them on-leash.

288
If none of us want dogs to pull, then why is it that so many dogs do pull? There are several reasons:
- Their humans haven’t managed to reinforce polite leash walking strongly enough to overcome the high-value competing reinforcers in their dogs’ environments.
- Pulling is sometimes reinforced (by allowing the dog to go where he wants when he pulls) and behaviors that are intermittently reinforced become very durable/resistant to extinction (it’s hard to make then go away).
- Dogs are confused by owners who sometimes want their dogs to walk in perfect heel position, and sometimes let their dogs wander, sniff, and yes, pull.
- It’s just not a natural behavior. Unlike sit, down, touch, jump, and many of the other behaviors we put on cue, dogs rarely plod sedately along in a straight line of their own accord. Since it’s not a behavior that comes naturally to them, we have to work hard to make it reinforcing and convince them it’s a behavior worth offering.
Avoidance behavior
Training your dog to walk politely on-leash used to be so simple, some folks say. When he stepped out of position you simply yanked, hard, on his choke or prong collar. He learned to march lock-step next to you to avoid being garroted, and all was well.
Only it wasn’t that simple. I used to train the “old” way, and we still had plenty of owners dragged across the parking lot by their dogs after class. Besides, dogs get hurt that way.
Some of the same owners who are inconsistent about reinforcement now were just as inconsistent about punishment then. Others were (rightfully) horrified at the prospect of yanking on their dogs’ necks hard enough to suppress natural sniffing and pulling behaviors, and they just ignored our instructions to “jerk harder!”
At any rate, many dogs who were “trained” to walk politely on-leash were really only trained to avoid the punishment of the collar, which is why dogs still wore their choke chains in the obedience competition ring (many still do) as a not-so-subtle reminder of what could happen if they stepped out of line. This, despite the American Kennel Club’s odd pretense that you’re not allowed to use “training equipment” in the ring. What is a choke chain if not training equipment? And we all know dog owners who still walk their dogs in prong collars months – even years – after completing old-fashioned training classes. The dog didn’t really learn how to walk politely on-leash; it’s just avoidance behavior; he doesn’t want those prongs to dig into his neck!

288
A partnership
Trainers and owners who subscribe to a positive approach to training are committed to making the process a partnership, with the dog willingly and happily participating in the behaviors asked of him. The exact opposite of the avoidance model, positive training asks the dog to voluntarily choose to offer the behavior so we can reinforce him for his choice.
The less natural and more complicated the behavior, the more practice – and reinforcement – the dog needs, to make the behavior a well-conditioned habit. Failures of leash training are most often a function of insufficient amount and value of reinforcement, lack of commitment to the necessary amount of practice, and impatience (increasing distraction and decreasing reinforcement too quickly).
Attention!
Realize that attention and focus behaviors are a hugely important piece of polite leash walking, and ones that you can practice with your dog separately from the actual leash-walking part. (See “Look at Me,” February 2004.) If your dog is paying attention to you, he’s not trying to sniff the bush you’re passing. You can practice attention exercises with your dog any place, any time, simply by reinforcing him with treats, attention, or a favorite toy any time he voluntarily glances your way. Shape for longer duration of attention by very gradually (a second or two increase at a time) waiting a little longer before you reinforce him for looking at you.
To get your dog’s attention when he hasn’t offered it voluntarily, teach him that a “Look at me!” cue is followed by a high value reinforcer. Say “Watch!” or whatever you want your cue to be, and feed a piece of something very tasty. When he has made a strong classical association with the cue (“Watch!” makes chicken happen!) you will be able to use your “Watch” cue to get his attention, even if he’s on-leash and distracted by a scent, a scampering squirrel, or the sight of another dog.
Age differences
Of course, polite walking lessons are best taught in puppyhood, before your baby dog has the opportunity to be repeatedly reinforced for pulling. Most young puppies naturally cling to the heels of their humans because they’re not confident enough to explore the world on their own. Start reinforcing this wonderful behavior early and often, and you build a foundation of a polite walking behavior that will make future leash training much easier for you. Your pup doesn’t even have to be on-leash for you to reinforce him for walking with you; just convince him from day one that being close to you while you walk makes very good things happen.
Once again, this proves the value of enrolling your puppy in a good, positive puppy training class as soon as possible. Sometime between the age of eight weeks and 16 weeks your pup will likely get bolder, and more willing to leave you to investigate his surroundings. A well-run positive puppy class is the ideal controlled environment in which to be able to reinforce him for walking with you even when there’s really interesting stuff nearby – like other puppies and humans.
When choke chains were de rigueur, training classes didn’t take puppies until the age of early adolescence, at six months, in part due to the potential for damage to tender puppy tracheas from enthusiastic jerks on the leash. With the advent of gentler training methods it has become perfectly safe – and appropriate – to start puppies in class at the age of eight weeks, as long as they are kept current on vaccinations throughout the class.
If it’s too late to start early, it’s still not too late to teach your dog polite leash-walking. It just means you’ll need more diligence and commitment to the training process to convince your adult dog that pulling on the leash no longer pays off. You will likely experience more and stronger pulling; you may need higher-value reinforcers and a higher rate of reinforcement; and you will probably find your dog reverting to pulling behavior more easily around novel or highly rewarding stimuli.
When you replace an existing unwanted behavior (pulling) with an incompatible one (walking politely) the original behavior never completely goes away (extinguishes). It lurks silently in the background, waiting for an opportunity to be triggered again (what’s called a “spontaneous recovery”). If that happens, you have to do the work, again, to prevent reinforcement for the pulling, and to reinforce the incompatible behavior that you prefer in its place.

375
If you’re prompt and consistent about it, pulling should extinguish again with relative ease. If you’re inconsistent – if you sometimes reinforce pulling by allowing the dog to move forward with a tight leash – it’s even harder to extinguish pulling behavior. Trainers actually put some behaviors on an “intermittent schedule of reinforcement” in order to make them very “durable” (resistant to extinction). On an intermittent schedule, your dog learns if he just does the behavior often enough, like playing a slot machine, eventually the reinforcement will come.
Separate but equal
Does this mean your dog always has to walk in step by your side, never looking to the right or left? Not at all. You can teach your dog two different leash-walking behaviors; you just have to use two different cues, being clear about which behavior you reinforce at any given time, and making sure neither one involves reinforcing your dog for pulling.
For my dogs, “Heel!” means, “Do that pretty obedience walking where you prance by my left side, gaze adoringly into my eyes and sit with your shoulder by my left knee when I stop.” “Let’s walk!” means “We’re heading in the same direction and you can wander and sniff a little as long as you don’t pull.” That way, we can go on some walks in tune with my agenda: get from Point A to Point B in the most efficient manner; and some that are in tune with my dog’s agenda: taking time to stop and smell the pee-mail.
How do you teach your dog to walk politely? First, have a clear mental image of the behavior you want. Second, prevent your dog from being reinforced for behavior you don’t want. Next, generously reinforce approximations of the behavior you do want; it’s a shaping process. I teach my dogs two leash-walking behaviors:
How to heel
My mental image of “Heel” is my dog walking at my left side with her shoulder in line with my knee. She watches me closely so she can read my body language and anticipate my movements. She turns when I turn, changes speed when I go faster or slower, and stops and sits when I stop.

288
- I prevent her from being reinforced for pulling by stopping or even backing up when she tightens the leash. I try to prevent her from reaching the end of the leash by using a high rate of reinforcement when she’s within the bounds of the leash-length. As training progresses, I reinforce (with a click! or another marker such as the word “Yes!” and a treat) ony for closer and closer approximations to actual heel position.
- Initially, I may reinforce (click and treat) her any time she’s close to the position I’d like her to be in, on my left side, as we walk. I also click and treat for any attention (direct eye contact) she gives me. I’ll add the “Heel” cue when she’s staying reasonably close to my left leg.
- I talk to her in a cheerful tone to keep her happy and attentive. I also change speed and direction frequently to keep the exercise interesting for her. I want her to think that “Heel!” is a fun game, not a boring trudge in a circle.
- As she tends to stay closer and closer to my left side (because that’s where I deliver the treats) I gradually raise the criteria for her to earn a reward (click and treat), by looking for (and clicking and treating) increasingly closer approximations of a perfect heel, until she eventually is walking in perfect heel position, her shoulder at my left knee. I also reinforce (click and treat) her for sitting when we halt, and gradually shape the sit so she learns that to sit in a perfect heel position as well.
Let’s walk
This is the behavior most dog owners (at least those who aren’t into rally and obedience competitions) want from their dogs: a nice, leisurely stroll around the block with canine as compatible companion – not glued to the leg, but also not dragging the owner down the sidewalk.
- Here’s my mental image: my dog ranges within 5.5 feet of me on her 6-foot leash, on my left side. She stops and sniffs if she wants, but also responds if I ask for her attention. If I give her the “Let’s walk” cue, she moves forward with me again.
- I prevent her from being reinforced for pulling by stopping or even backing up when she tightens the leash. I try to prevent her from reaching the end of the leash by using a high rate of reinforcement when she’s within the leash-length.
- As training progresses I reduce the rate of reinforcement so that, eventually, my dog needs only very occasional clicks and treats on our walks. Of course, I always increase rate of reinforcement if I think circumstances demand it – such as the appearance of very exciting distractions.
- Since this is a less precise behavior than “Heel,” I don’t have to spend time shaping to a very specific position. I do like my dogs to stay on one side rather than criss-crossing back-and-forth or worse, wrapping around me, so I shape for a left-side “Let’s walk” by gradually raising criteria until I’m reinforcing only loose-leash walking on my left side.

385
Technique
I’ll leave you with a final word or three on technique:
- Remember to click for behavior (Click! That behavior just earned you a treat!) and feed for position. If, for example, you’re shaping “Heel” in the early stages, you may click for a behavior that’s still far from perfect heel position, but if you feed the treat at the side of your left knee, you’ll encourage your dog to stay closer to that perfect spot.
- Many trainers carry their treat in the left hand to encourage left-side walking. This is actually a bit of luring, and makes it harder to eventually fade out the presence of the treat. I prefer to hold treats in my right hand (leash in my left) with my hand out of sight behind my right hip, and deliver across my front to the side of my left knee after I click. This way your dog has to think about where he needs to be to earn the click, not just follow the tempting scent of the treat in your left hand.
- I don’t generally wear a treat bag; I prefer to wear loose clothing where I can stash bags of treats in pockets. A treat bag is a flashing neon sign to your dog that now he has the opportunity to earn treats. I’d rather my dogs know they may be reinforced at any time, not just when I’m wearing the bag.
- Vary your reinforcers. As the late positive trainer Patty Ruzzo frequently said, be variable and unpredictable. Don’t always make it about food treats. If your dog never knows when, where, or how you might reinforce him, he has to stay attentive to you; he won’t want to miss anything! My personal choice is this: If I click my dog gets a food treat; if I use some other reinforcer I use my verbal “Yes!” marker. Now, go walk your dog!
Thanks to Sarah Richardson, CPDT-KA, CDBC, of The Canine Connection, in Chico, California, for modeling the techniques discussed in this article.
Pat Miller, CPDT-KA, CDBC, is WDJ’s Training Editor. Miller lives in Fairplay, Maryland, site of her Peaceable Paws training center. Pat is also author of The Power of Positive Dog Training; Positive Perspectives: Love Your Dog, Train Your Dog; Positive Perspectives II: Know Your Dog, Train Your Dog; and Play with Your Dog.
The Tellington TTouch For Dogs
For many years, I was curious about Tellington TTouch (pronounced TEE-touch) Method, a training system that uses bodywork and non-habitual movement to influence behavior and health. But I was skeptical that the hallmark circular touches with fanciful names like “Clouded Leopard” and “Tarantulas Pulling the Plow” would have much impact beyond helping an animal relax; wasn’t this just another form of petting and massage? It wasn’t until I witnessed a TTouch practitioner work with my young dog, Chance, that I realized there was more to TTouch than I had imagined.

photo by Donna Zetterquist
At that time, trust did not come to Chance easily. Her background as a feral dog meant that she was often overwhelmed during social interactions with humans. Her lack of trust manifested in hyper-social behavior. And, even though she had learned to sit when greeting people and she behaved well when asked, she was often on the verge of an eruption of nervous hyperactivity when interacting with people.
As I watched Jodi Frediani, a TTouch practitioner who holds workshops in the Santa Cruz Mountains (near the central coast of California), I saw a subtle change in Chance’s demeanor. It wasn’t that Chance immediately calmed down, though we did see a mild shift in her hyper behavior. It was the way that Chance and Frediani were communicating through the touches that was so impressive. When using TTouch, Frediani entered into a mutually respectful relationship with Chance, a noninvasive and nonconfrontational give and take. TTouch helped to create a dialogue between the dog and practitioner. Chance’s body language shifted from stiff and tense, to softer and more relaxed. The growing trust was evident.
What is TTouch?
The TTouch method was developed by Linda Tellington-Jones. The Canadian horsewoman had a long background in horse training and massage, but in 1970s, she began studying with Dr. Moshe Feldenkrais, an Israeli physicist. Feldenkrais had developed a method of gentle manipulation of the human body, designed to improve pain and movement. He believed that by engaging non-habitual movement, you might be able to activate unused neural pathways to the brain and expand the potential to learn. Tellington-Jones’ study of the Feldenkrais method of “Awareness Through Movement” sparked a shift in her thinking about touch and movement in animals.
Tellington-Jones began to experiment with non-threatening manipulations with horses. Her experimentation lead to her development of the Tellington Touch Equine Awareness Method (TTEAM), a training system for horses that included a circular touching technique, ground work, and riding exercises. The approach seemed to help horses relax and move beyond instinctive responses into a more grounded and thinking state. Tellington-Jones found the method to be very effective and in the 1980s began adapting it for working with other animals, including dogs, and TTouch was born.
Tellington-Jones writes that the goal of TTouch is to “stimulate the function and vitality of the cells in an animal’s body, and to activate unused neural pathways to the brain.”
TTouch likely engages the parasympathetic nervous system, relaxing muscle tension and allowing heart rate, blood pressure and circulation to slow, in effect bringing stress levels down. Bringing the stress level down may allow a dog (or person or horse) to have more body awareness, which can help if the body is compensating because of a past fear or pain, says Frediani. “The touches, in some fashion, help to release that memory and bring about healthy function in the cells.”
One study, done at the Biofeedback Institute in Boulder, Colorado, showed that TTouch can create changes in certain brain waves. During the study, the brain wave patterns that emerged during TTouch were different from those that emerged from simple petting, stroking, or massage. The results suggest that TTouch may relax the body and brain while simultaneously encouraging an alert, thinking state.
Tellington-Jones describes the effect of TTouches as “turning on the electric lights of the body,” but she acknowledges that no one really knows how or why TTouch works and that the secret may simply be the mindfulness of the method.

“TTouch is based on a mindful approach to working with the animals,” says Frediani. “Everything we do is mindful and thoughtful. I constantly read the dog’s body language, staying attuned to his emotional state as best I can. I pay attention to both the dog’s response to my touch, body language, and movement, and also the messages that my fingers are giving me. Is what I am feeling hard to the touch? Cold? Trembling? All of this is information that helps adapt what I do and how I do it.”
TTouch is Cooperation-Based
Perhaps the biggest influence of TTouch is that it promotes a philosophy of cooperation and respect in all of our interactions. “TTouch is about partnership,” says Frediani. “It’s about working in a collaborative fashion.”
Frediani trained with Tellington-Jones, and says, “It was an experience that transformed how I live my life.” Frediani continues to practice and teach TTouch, including working with a variety of animals throughout the world, teaching others to lead classes, and offering workshops for dog owners at her home in California.
“In the TTouch philosophy,” says Frediani, “most behavior problems arise because of fear or pain, or because the animal doesn’t understand what we want.” The TTouch method strives to alleviate these issues with three primary techniques: circular touches, body wraps, and movement exercises. These elements work together to bring about a relaxed, calm state that enables the animal to learn. TTouch can function as its own behavior modification program, but it is also often used to complement other reward-based training and behavior programs.
TTouch can be particularly helpful with anxiety-based behavior issues such as social fears or sound sensitivity. With these types of problems, the results of TTouch are often dramatic.
“The intention is to bring awareness, to get the dog to use his thinking mind and not his reactive, primitive brain,” says Frediani. “The touches get the dog to slow down and respond.”
I witnessed a stressed Border Collie fall into a deeply relaxed state in a matter of minutes during a TTouch demonstration. During my research for this article, numerous people related accounts of tail work, ear slides, and body wraps providing miracle-like results for sound sensitivity. For example, Dr. Evelyn Sharp of My Personal Vet in Santa Cruz, California, says she remembers using the TTouch “tail work” with her first dog, Cray, for his fear of thunderstorms.
“Cray would flip out, digging to try and escape, pacing, panting, ears back,” says Dr. Sharp, who had learned about the tail pulls during a TTouch course for horses in the 1980s. “For the first two or three pulls he was worried. But after five tail pulls, he just lay down and went to sleep.”
TTouch is also useful in highly arousing situations. Because it both calms a dog and seems to open him to learning, TTouch may be particularly helpful with performance dogs, for example, as a way to encourage focus before going into the competition ring. It may also be helpful with activities such as vet visits or training classes.
“I use TTouch to get my classes settled down,” says Sandi Pensinger of Living with Dogs in Capitola, California. “If something disrupts the class or dogs get aroused by motion or eye contact, we sit down and do relaxation with TTouch and breathing. The dogs settle down and often fall asleep. It’s amazing!”
But the results of TTouch are often more subtle, as with Chance and her hyper-social behavior. Chance is still often on the verge of a mini-over-excitement-explosion when interacting with people, but TTouch has helped shift her energy from nervous panic to simply excited.
TTouch can also be helpful as an adjunct therapy for hip dysplasia, lameness, and recovery from surgery or other illnesses. “It is not going to cure a dog of cancer or other ailments,” says Frediani, giving an example of the limitations of TTouch. “But it could help make the dog more comfortable and help with the bond between animal and person while the dog is going through the illness.”
TTouches in Action
There are over a dozen different touches used in TTouch. Probably the best way to learn about the touches is to find a practitioner in your area. But you may be able to learn about them from the books or videos available as well.
Many of TTouches employ the hallmark circular motion, but several are more akin to a stroke or lift. Some of the touches are done using only the fingertips, others the flat of the fingers and palm, still others use the whole hand against the dog’s skin. The circle movement is generally done clockwise, starting at the 6 o’clock position and moving around for a one and a quarter circle. The touch is generally light rather than deep like a massage and the goal is to gently move the skin under the fingertips.

Pressure is another aspect of the touches. The pressure scale ranges from one to six, with one being the lightest, and six being the heaviest. The pressure of the touches is much lighter than you might imagine. To get an idea of the pressure of the touches, try moving the skin around on your eyelid using the lightest possible pressure. This would be a number one. A number three is the pressure it takes to move the skin around on your eyelid as firmly as is comfortable. A number six is twice the pressure of a number three (too much pressure to use on your eyelid and with most dogs, and is generally used with larger animals). Each dog prefers a different pressure, and it helps to experiment to find the right pressure for the individual.
The circles are complete within themselves, but they are done in succession moving around on the body. As soon as you are finished with one circle, connect it to the next one by sliding along the fur to your next position, moving parallel to the spine or down the legs. The circular touches can be done anywhere on the body.
Here are examples of a few of the different touches and how they are used:
“The Clouded Leopard” – This is the basic touch and all of the other circular touches are variations of the Clouded Leopard. With the Clouded Leopard, your fingers are slightly curved and you use the pads of your fingers to create the circles. The Clouded Leopard is particularly useful for anxious dogs and regular work with Clouded Leopard may help develop trust. One variation of the Clouded Leopard is the Abalone touch, which uses a completely flat hand against the skin.
Ear slides – Using TTouch on the ears is an important technique and can help calm a stressed or hyperactive dog. The ear slide is done by stroking the ears horizontally from base to tip, or by making small circles starting at the base and working toward the tip.
“Ear work can also be a very helpful tool if you have a hurt or injured animal or an animal in shock. You can use an ear slide while going to the vet.” says Frediani. “There are acupressure points in the ear that are connected to the whole body, and without having to know specific points, one can activate them and stabilize pulse and respiration.”
Tail work – One of the most interesting TTouch techniques is a simple tail pull. With your dog standing or lying down, you hold her tail near its base with one hand, while supporting her body with the other, then gently pull, holding the tension for a few seconds and then slowly, gently releasing. You can also move the tail in a circular motion, or do “Raccoon touches” on the tail, a method that uses just the very tips of your fingers and a circular motion.
“Tarantulas Pulling the Plow” – This is my favorite slide type of touch. You walk your fingers gently up the back (like a spider) while letting the thumbs drag behind (like a plow). It can help stimulate circulation and may be helpful for dogs with touch sensitivity.
Beyond the Touches
There are several other techniques that are part of the Tellington TTouch Method. These techniques are all designed to help a dog gain a calm confidence. “It is hard to be emotionally confident when you are not physically confident. With physical confidence, the tail comes up, the posture changes, the dog feels good about himself,” says Frediani. “It is easier to feel good about the rest of the environment, other animals, and even people when you feel good about yourself.”
Leading exercises – TTouch employs a range of exercises designed to help a dog work in cooperation with the handler. The goal is to teach a dog to understand what is expected, and for the dog to move without pulling or straining on the leash. Some of the leading exercises use a double clip leash with the ends clipped to two different points on the dog; for example, one end might be clipped to the collar and the other to a front clip harness.
Confidence course – The confidence course, as the name suggests, is designed to build a dog’s overall confidence. It may include obstacles similar to those used when introducing a dog to agility equipment – a ladder, a low dog walk or A-frame, a tippy board or low teeter-totter, tires and cones. A simple labyrinth made from six poles on the ground is a common feature of the TTouch confidence course. “The confidence course can help a dog solve problems and learn physical balance, which is connected to mental and emotional balance,” says Frediani.
Body wraps – Traditionally in TTouch, the body wrap is done with an ace bandage wrapped in a pattern around the dog’s body, but I’ve also heard of people using scarves, tight t-shirts, and more recently a commercially designed product called a Thundershirt. Body wraps can be so effective in helping a nervous dog settle that when I was looking for examples of how TTouch had benefited dogs, the response was overwhelmingly related to great effects of body wraps for things like thunderstorm and firework fears. The idea of the body wrap is that a gentle pressure on a dog’s body can help calm the nervous system. One person I talked with said the body wrap was like giving your dog a nice reassuring hug.
Therapy for Dog Handlers, Too!
One of the aspects of TTouch that I like is that it is easy to do, and it feels good doing it. Perhaps it is the mindfulness approach, or the simplicity of the touches and movements, or the fact that it doesn’t have to be done perfectly to have a positive effect. It’s very forgiving and can be adapted to fit an individual dog’s needs.

“With TTouch, we allow the dog to lead the way,” says Frediani, “and mistakes are part of the process. If what you do doesn’t work, try something different. Set goals, but remain unattached and know that you can change what you are doing.”
Practicing the TTouch techniques is also a great way to connect with your dog. To help strengthen her connection with her dog, Chloe, Lori Rubin took a workshop with Frediani. Rubin says, “I rely on the circle touches when I think something might be stressful for my dog, like when I take her to the vet. It gives me something to do that I know is nurturing to the dog.”
Putting TTouch to Work
TTouch can have a dramatic effect on dogs. Sometimes the help offered through TTouch is subtle. And sometimes, like with all behavior methods, it might not help with a particular behavior or problem. But even that fits in with the TTouch philosophy.
“As with all systems there are times that the methods won’t be as effective and there are some animals that won’t respond,” says Frediani. “If I’m working on an animal, and the animal expresses concern, I might do the touches on a different part of the body, I may change the pressure, the speed, or which touch I use to make it easier for the animal to participate in the process.”
Frediani stresses that in TTouch, you always work for success, which, in this case, means moving forward together and allowing the animal to participate in the process. “I want the animal to be able to express how she feels. I don’t want to inhibit that,” says Frediani. “I don’t want a dog to go ballistic, but I also don’t want her to suppress her communication.”
In TTouch, communication and cooperation remain key to the process. TTouch improved how my dog Chance communicates with me, as well as how she relates to other people. She will often back herself into a person as if to say, “Would you like to communicate with me through those funny circle touches?”
Mardi Richmond, MA, CPDT-KA is a training enthusiast and writer who lives in Santa Cruz, CA with her partner and her heeler-mix, Chance.
Special thanks to Jodi Frediani of Transformational Training, for her assistance with this article.
Competitive Canine Weight Pull
[Updated July 19, 2017]
CANINE WEIGHT PULL OVERVIEW
What is this sport? In weight pulling, a dog‘s strength and stamina are tested by his ability to pull weights.
Prior training required? Moderate.
Physical demands? On the dog: Moderate to high. On the handler: Minimal.
Best-suited structure? Dogs of all sizes and shapes can compete, although the bully breeds do best.
Best-suited temperament? Dogs who enjoy working with their owners.
Cost? Minimal.
Training complexity? Minimal.
Mental stimulation? Moderate.
Physical stimulation? High.
Recreational opportunities? Low.
Competition opportunities and venues? Moderate.
Work it! Work it! Work it! Leaning into the padded harness, muscles bulging with effort, eyes dark with determination, inch-by-inch, the American Staffordshire Terrier pulls the cart loaded with 60-pound pieces of railroad track toward her owner. This is Duvall’s Sureshot Kamakazi, “Banzai,” a striking 43-pound, 17-inch brindle girl. Her owner, Karyn Dawes, smiles wide as she realizes that Banzai is going to record a new “personal best.” It’s official: 3,900 pounds and 90.7 times her body weight. What a gal! Banzai wiggles in delight at Karyn’s hug and effusive praise for a job well done.
In 2003 when Dawes discovered the sport of weight pulling, she had no idea she and her dogs would enjoy it so much. She was an experienced dog sport aficionado, having competed in obedience, Schutzhund, flyball, agility, and carting. It was only at the insistence of a good friend that she capitulated and gave pulling a try. Like many neophytes to a sport, she made a lot of mistakes at the beginning, and then went on to put titles on 11 dogs.
“My first time was cold turkey,” Dawes recalls. “No training, no practice. I borrowed a harness just for fun to see what the dog would do. You’d think by now I would know better! My dog pulled a qualifying pull the first day. The second day she ‘told’ me that if I want to do this sport, she would like me to invest some time in training and conditioning. In other words, I got the ‘paw.'”
Weight Pull History
Dogs have pulled sleds and carts for humans throughout history. In small towns around the world, owners proudly boasted of how strong their dogs were, how much they could pull and how far. “Yeah? You wanna bet? My dog can pull more than your dog!” That’s probably how the sport of weight pulling started. Now there are several organizations that have established rules and regulations for formal competition.
Although any breed can enjoy this sport, it is one that commonly attracts more “bully” breeds (such as American Staffordshire Terriers, Bulldogs, Mastiffs, Boxers, etc.) than any other breed. Some of the sanctioning organizations limit their competitions to purebred dogs while others are open to all dogs.
The United Kennel Club (UKC) rules of competition reflect the goals of most weight pulling competitions, which is to demonstrate a dog’s stamina and strength. In brief, each dog is given 60 seconds to pull the most weight that he can in a 16-foot “chute.” Dogs are separated into “classes” based on their body weight. Dogs who pull a larger percentage of their body weight earn the most points.
The dog wears a padded harness, which is attached to a “trace,” which connects to a “weighted vehicle” that is loaded with sand bags or other easily weighed objects. There are three different types of vehicles.
- Sleds are pulled on natural or artificial snow and must be able to carry a minimum of 3,000 pounds.
- Double-axel wheeled carts are pulled on carpet and must be able to carry at least 5,000 pounds.
- Rail carts are pulled along a rail system and must be able to carry at least 6,000 pounds (the dogs’ path is carpeted so they can achieve traction when pulling).
The chute that contains the pulling system is 35 feet long and between 10 and 20 feet wide.
Canine Weight Pull Titles
There are several titles available in the UKC system. These are just some of them:
- United Weight Puller (UWP): Three qualifying pulls are required. These can be all using the same type of weight vehicle or a combination of the three different vehicles. Each of the different vehicles has a different weight requirement. For example, a dog pulling a sled must pull 3 times his body weight; a dog on rails must pull 10 times his body weight; and a dog pulling a cart must pull 8 times his body weight. You must have the UWP title before pursuing the various championship titles.
- United Weight Pull Champion (UWPCH): Once this level of competition is reached, the competitor starts earning points toward the UWPCH title. 100 points are required for the UWPCH.
- United Weight Pull Champion Excellent (UWPCHX): 250 points are required for this title.
- United Grand Weight Pull Champion (UGWPCH): The dog must have completed the UWPCHX title before earning the additional 200 points for this title.
- United Grand Weight Pull Champion 1 (UGWPC1): The dog must have completed the UGWPCH before earning the additional 200 points for this title.
The somewhat complicated point system is described in detail on the UKC website. Generally, points are earned for the higher levels of competition based on placements (first through fourth place) and the type of vehicle pulled. For example, dogs pulling on wheels earn 20 points for pulling 35 times their body weight, 15 points for 25 times their body weight, 10 points for 15 times their body weight, and 5 points for 10 times their body weight. There are also bonus points awarded for dogs who pull the most weight and the most weight per body weight at each competition. Additional titles require a dog to pull a combination of different vehicles.

There are annual “All Star” rankings based on points earned throughout the year. The rankings are broken into three classes: 1) American Pit Bull Terrier; 2) American Bulldog; and 3) Multi-breed (all other breeds). For dogs who show in conformation as well as weight pulling, there is also a Total Dog Award that can be earned at individual shows by qualifying in a performance sport and taking one of the “winners” awards in conformation on the same day.
Training
Basic pet manners training provides a good foundation for the sport of weight pulling. Your dog needs to be under control and to have been adequately socialized with people and other dogs in order to be comfortable in a competitive environment. That said, weight pulling does not require extensive training. What it does require is the human on the other end of the leash to very gradually physically condition her dog before asking him to pull larger and larger percentages of his body weight.
Dawes, who has trained and titled 11 dogs in the sport, starts by introducing the harness first. “I put the harness on and do short walks with plenty of treats and encouragement. I make sure to hold the spreader bar at the back of the harness so it does not bang the back of the dog’s legs. ‘Drag training’ starts with a plastic bottle filled with small rocks. This is not heavy. Its main purpose is to get the dog used to something noisy following behind. Next I introduce an empty sled. This weighs about 15 pounds. We do lots of praise and rewarding – not luring – but rewards for short distances.”
Experienced handlers know that luring or “baiting” a dog to pull might cause the dog to pull more than he is physically or mentally prepared for. Under the rules of most sanctioning organizations (there are exceptions), handlers are not allowed to use lures or bait during a competition. Although treats are used, they are used to reward the dog for short-distance pulls and gradually increasing weight loads.
“As the dog becomes familiar with the job, I increase the amount of weight and vary the training,” says Dawes. “For example, I might use a heavier weight for short distances and a lighter weight for longer distances. Most of the actual training is done with a sled as few people own their own wheel or rail systems. Occasionally, club members will get together to work their dogs on the actual competition pulling equipment.”
Many people join clubs and train and practice together. Dawes joined her friend’s club, Rip Curl Weight Pullers, and got a lot of help from other members over the years. She now helps newcomers and provides private instruction, as do some of the other club members. The club occasionally offers seminars, but members feel that the real benefits of the club are the camaraderie and support they get from one another.
“We are all enthusiastic about the sport and are always willing to answer questions and give people tips to help them start. When we hold pulls, we encourage people to come without their dog and observe. Once you understand the basics, it’s pretty much a matter of training and conditioning on your own. Just remember: be patient and never forget that the dog did not sign on for the job. You chose the sport; the dog did not. Dogs have good and bad days. Keep your training positive and respect your dog.”
To find a club in your area, go to the UKC website.
Canine Weight Pull Team Attributes
Many who are attracted to dog sports cite the strong relationship that results from the time training and playing together. Weight pulling is no different. “Like any of the dog sports when I ask ‘what’s in it for the dog,’ I have to first point to the quality and quantity of time we spend together,” says Dawes. “Training for anything builds a strong relationship. Some dogs really love the sport. Most work to please their owner. Unfortunately, there are a few people who still use aversive training methods (something that our group does not endorse). You can tell which dogs are trained this way as they walk onto the track.
“Weight pull is work! So, unlike agility or flyball, where the dog barks, jumps, and runs (all things most dogs inherently enjoy), the dog must want to work for the owner or rewards at the end of the pull. There are some dogs who really love pulling, but I would say that most pull to please their handlers.”

The sport attracts many of the “bully” breeds, but Dawes has seen, among others, Great Danes, Rat Terriers, Cattle Dogs, Black and Tan Coonhounds, Basenjis, Patterdale Terriers, Boston Terriers, Shelties, and even an Italian Greyhound. “This sport is mental as much as it is physical. If you capture the dog’s mind, their doggy body will follow. It’s a bit like ‘The Little Engine That Could’ – if they think they can, dogs can do some amazing things.”
People who love this sport come from all walks of life. In the Rip Curl Weight Pullers Club there is a veterinary technician, a groomer, a paramedic, retirees, a heavy equipment operator, and Dawes, who is currently a booking agent for a pet transport company. Prior to finding satisfaction making sure pets arrive safely, she was an advertising sales and layout designer for an aviation newspaper.
Club members may participate in a variety of dog sports although some concentrate all their efforts on this one. “There is the element I refer to as the ‘heavy hitters’ whose only sport is weight pull. These folks parallel the obedience folks who are after the 200 score or the agility people who are aiming for the World Team.”
Equipment and Expenses
Equipment costs are minimal for basic training and conditioning, but you’ll need to join a club unless you want to assume the cost of and find the space for a pulling system. As a member of a weight pulling club, this sport is pretty inexpensive. When you can find someone to instruct you on a private basis, expect to pay around $40 per session. A custom harness for your dog will cost around $75. Entry fees for competition cost about $25.
Get Started!
You might be surprised when you learn that your dog enjoys a sport that results in so much hard work for him. But, with the right animal magnetism, you just might convince him that you’re worth it.
Terry Long, CPDT-KA, is a writer, agility instructor, and behavior counselor in Long Beach, CA. She lives with four dogs and a cat and is addicted to agility and animal behavior.
Something Is Not Right
Why are vaccinations so over-promoted by veterinarians? I’m begging for someone to explain this. Because, from my perspective, there are so many more serious threats to dogs’ health and well-being than whether they receive the fourth or fifth or tenth DHLPP vaccine in their adult lives.

288
Let me be clear: I sincerely wish for all dogs to be vaccinated when it’s necessary. Spend enough time in an animal shelter in a poor district and you will see precisely how deadly it is to be an unvaccinated dog. Puppies and adolescent dogs should be vaccinated, and then – in my opinion and that of a slowly growing number of enlightened veterinarians – dogs should be given an antibody titer test. This will determine whether they are adequately protected from the diseases for which they were vaccinated. For more detail on this topic, see Lisa Rodier’s article, “Annual Vet (Not Vaccine) Visits.”
Practically every time I go to a vet clinic, though, I witness the most disturbing exchanges between the office staff and the clients about vaccinations. I’ve been astonished at the aggressiveness with which the vaccines have been promoted – particularly when the clients’ dogs had more serious health issues that were screaming out for attention!
For example: A man comes in with an old dog; she looked at least 12 or older. She’s obese, arthritic, and covered with what appear to be fatty tumors. She has no collar. Why are they there? A wellness exam and blood chemistry? To find out how to reduce the dog’s weight and improve her mobility? No. “I got one of them postcards?” he says to the receptionist, and he gives his name. “Right,” she replies. “Your dog needs her annual vaccinations. Take a seat, we’ll be right with you.”
I thought, “Okay, don’t jump to conclusions. If it wasn’t for the postcard, this guy may not have ever brought the dog to the vet. Maybe once the tech and the vet see the dog, they’ll realize she has more serious health issues that need to be addressed.”
Only that didn’t happen. A few minutes later, a technician calls the man’s name, and he takes the dog into an exam room, and comes back out about two minutes later. Pays his bill and leaves. Zero conversation about the myriad things that are far more likely to kill his senior dog than parvo or distemper.
Another time I visited a vet hospital during a “low-cost vaccine clinic.” (I was there to buy heartworm preventative.) In front of me was a couple with two mixed-breed dogs. Both dogs had skin problems. Both had collars; neither had an ID tag. The male was intact; the female clearly had a litter of puppies in recent weeks – judging from the appearance of her teats, probably not her first litter. They were there to get the dogs vaccinated. What for? They didn’t know, and the dogs had not been to that office before. They asked the receptionist, “What do they need?”
If they asked me, I would have answered, “Sterilization surgery, identification, heartworm tests, and a flea control product.”
But the receptionist didn’t blink. “Well, we have a lot of vaccines. There’s the ‘annual,’ plus rabies, and a lot more . . .” The matter was settled by how much money the man had in his pocket; they got the “annual,” plus rabies. Not one word about the puppies.
The profit on vaccines (especially at a low-cost clinic) can’t be that great; a vet could make way more money by providing the services dogs really need. So why don’t they do that? Or, at least, spend a few minutes educating their clients about their dogs’ more urgent needs? I’ll bet more adult dogs die in American shelters from a lack of ID than from a lack of vaccinations. And why wouldn’t a vet promote spay and neuter surgery to people whose dogs clearly need it?
I honestly don’t understand.
Shortage of Immiticide for Canine Heartworm Treatment
On December 1, 2009, Merial published an open letter to veterinarians, announcing a shortage of Immiticide (melarsomine dihydrochloride), the only drug licensed for use in treating heartworm infestations in dogs. The shortage is due to a manufacturing site transfer. The company expressed hope that the shortage will not persist beyond the first quarter of this year.
An apparently unrelated problem is responsible for Merial’s announced shortage of Heartgard (ivermectin) tablets, which may be unavailable until 2011. Heartgard prevents canine heartworm disease by eliminating the “tissue stage” of heartworm larvae for a month after infection.
Fortunately, Heartgard chewables and other ivermectin products (including products made by other manufacturers) remain available, so a shortage of the tablets is not cause for concern. The Immiticide shortage, however, has alarmed veterinarians and shelters (who see a lot of heartworm-positive dogs) across the country.
To repeat: Immiticide is the only drug licensed or used to treat adult heartworms in dogs, and Merial is the only company who makes this product. Because of the shortage, veterinarians can no longer order Immiticide from distributors, in order to prevent stockpiling.
Instead, veterinarians who have a heartworm-positive patient must contact Merial directly and provide details of their patient’s case. For now, Merial is selling the drug on a case-by-case basis, providing the drug only to the more severe cases, those dogs with clinical signs of heartworm disease. Dogs who test positive but have no clinical sign of disease will have to wait.
Safe, effective alternative
Fortunately, there is an alternative treatment for heartworm. As we discussed in “Update on Doxycycline and Heartworm Disease” (Whole Dog Journal August 2009), a combination of ivermectin (the active ingredient in Heartgard) and doxycycline (an antibiotic), weakens and sterilizes adult heartworms, eventually killing them. The time this takes depends on the age of the worms; the older the worms, the longer they take to die.
In addition, giving doxycycline and ivermectin prior to treatment with Immiticide lowers the risk of adverse reaction to worm death, making the treatment much safer. It also lessens the negative effects of the worms themselves, primarily due to doxycycline’s effect on Wolbachia, a parasite of heartworms (see “Parasites within Parasites,” Whole Dog Journal August 2006).
The American Heartworm Society (AHS) recently updated its guidelines for treatment of heartworm infection in dogs. It says, “Studies have shown that heartworm-positive dogs pretreated with ivermectin and doxycycline prior to receiving melarsomine (Immiticide) injections had less pulmonary pathology associated with the death of the heartworms. If doxycycline is incorporated into a heartworm treatment protocol it should be given before administration of melarsomine so the Wolbachia organisms and their metabolites are reduced or absent when the worms die and fragment. Doxycycline administered at 10mg/kg BID for four weeks has been shown to eliminate more than 90 percent of the Wolbachia organisms and the levels remain low for three to four months.”
For dogs who are not treated with Immiticide, the guidelines say, “the use of a monthly ivermectin-based heartworm preventive along with doxycycline could be considered. It has been reported that ivermectin and doxycycline administered periodically over 36 weeks resulted in a 78 percent reduction in adult worm numbers. Moreover, microfilariae from dogs treated with doxycycline that were ingested by mosquitoes developed into third-stage larvae that appeared to be normal in appearance and motility, but these larvae were not able to develop into adult worms, thus negating the risk of selecting for resistant strains. The administration of doxycycline at 10 mg/kg BID for a four-week period every three to four months should eliminate most Wolbachia organisms and not allow them to repopulate.”
While the AHS still recommends monthly use of heartworm preventatives in combination with doxycycline during treatment for heartworms, the studies reported above used standard heartworm preventative doses of ivermectin given weekly during the 36-week treatment period. They also pulsed doxycycline throughout the treatment period rather than just giving it every three to four months.
Based on the above, it may be best to give Heartgard (not Heartgard Plus) weekly until treatment with Immiticide is begun, or until the dog no longer tests positive for heartworms, if Immiticide treatment is not used. Giving Heartgard weekly (rather than monthly or every two weeks) is less important for dogs who will be treated with Immiticide than those relying on ivermectin and doxycycline alone to get rid of heartworms. (Note that weekly Heartgard is not recommended for dogs with the MDR1 gene mutation that causes sensitivity to ivermectin.)
Doxycycline should be given at the dosage level listed above for four weeks prior to starting Immiticide treatment. If treatment has not been completed within three to four months, doxycycline should be given again for four weeks. If Immiticide treatment is not done, treatment with doxycycline should be repeated every three to four months until the dog no longer tests positive for heartworms.
Ivermectin and doxycycline may seem a safer (though slower) alternative to Immiticide, even when the shortage is over. But heartworms cause damage as long as they are in the dog’s body, and the danger from the dying worms, while reduced by the use of doxycycline, exists as long as the worms are present. Immiticide following one month of treatment with doxycycline and ivermectin is still the treatment of choice for most dogs with heartworm disease. If Immiticide treatment is not available, or if you have a dog with early-stage heartworm disease, then long-term use of ivermectin with doxycycline is a reasonable alternative. – Mary Straus
For more information:
Merial Customer Service, merial.com, (888) 637-4251 (option 1)
heartwormsociety.org/veterinary-resources/guidelines-Can-HW-Disease.pdf
More States Change Rabies Vaccine Requirement
Arkansas canines and their humans have very good reason to celebrate the start of the new decade. That state’s new rule allowing for a three-year rabies vaccine became effective January 1, 2010. This means dogs in Arkansas will need to be vaccinated only every three years (after their initial first-year booster) instead of annually, as was previously required.

288
The majority of states in the U.S. now allow for the three-year vaccination schedule. Despite a slightly premature announcement from the Rabies Challenge Fund (rabieschallengefund.org) last August that all 50 states had accepted a three-year protocol, a few still do not. Rhode Island’s Rabies Control Board approved a change in April of 2009 accepting the three-year vaccination, but as of yet no effective date has been set. Until that happens, Rhode Island dog owners are still required to vaccinate their canine companions every two years. West Virginia also requires vaccination bi-annually. There may be a few others. Still, every state that approves a three-year schedule is one step closer to that 50-state goal.
Meanwhile, the Rabies Challenge Fund is now raising funds for a fourth year of the Rabies Challenge Study at the University of Wisconsin School of Veterinary Medicine. It will cost about $150,000 per year to cover the remaining four years of the seven-year study that hopes to confirm that rabies vaccinations are effective for at least seven years. This would reduce the necessity to vaccinate as often, and minimize exposure to the potentially carcinogenic adjuvant that is part of the vaccine, as well as to the sometimes deadly adverse reactions some dogs experience to the vaccine.
The second phase of the project will finance a study of the adjuvants used in veterinary vaccines and establish a federal adverse reaction reporting system for rabies and other vaccines.
This project depends primarily upon grassroots gifts for funding the costs of conducting the requisite vaccine trials. To date, contributions have come mostly from kennel clubs and private individuals. The Rabies Challenge Fund Charitable Trust is a federally registered 501(c)(3) charitable organization. – Pat Miller
For more information:
Rabies Challenge Fund
rabieschallengefund.org
AAHA to Create New Nutritional Guidelines
In January, the American Animal Hospital Association (AAHA) announced its plan to create a new set of nutritional guidelines for use by veterinarians and to publish these recommendations in June 2010.
The newly formed committee includes academic leaders, animal hospital directors, and veterinary technicians: Tony Buffington, DVM, MS, PhD, Dipl. ACVN, Ohio State University; Joe Bartges, DVM, PhD, Dipl. ACVIM, University of Tennessee; Lisa Freeman, DVM, PhD, Dipl. ACVN, Tufts University; Don Ostwald, DVM, Dipl. ABVP, Wheat Ridge Animal Hospital, Wheat Ridge, Colorado; Mary Grabow, DVM, Noah’s Westside Animal Medical Center, Indianapolis; and veterinary technicians Julie Legred, CVT, and Kimberly Baldwin, LVT. The AAHA’s goal is to incorporate the latest advancements in medical knowledge, but remain practical enough that veterinarians can use the guidelines to make recommendations to their clients. “It’s time we put nutrition in the minds of veterinarians,” says AAHA President John Tait, DVM. While no details about the scope of the guidelines are available, Tate indicated that poor client compliance (with feeding prescription diets) and the impact of nutrition on pet health are the driving forces behind the decision to create these guidelines.
Another likely factor is the increased interest in homemade diets, especially following the massive pet food recalls in 2007. “Pet owners are inundated with advice from a variety of sources on what constitutes proper quality of care and treatment of their pets. Unfortunately, many of these sources are not credible,” says Dr. Tait.
There are far too many inappropriate or inadequate recipes available to owners, for both healthy dogs and those with health conditions requiring a modified diet. The question is, will the AAHA’s new nutritional guidelines focus on what has been learned about nutrition in the past 10 to 15 years, or will they simply rely on the same high-carb, low-protein formulas that the pet food companies have promoted for so long? Hill’s Pet Nutrition has provided funding for the task force and has promised to help implement the guidelines when they are published, so we’re not overly confident that the new guidelines will be all they could be. We’ll analyze them when they are published, and share our analysis at that time. – Mary Straus