We had a little practice fire drill here last week. I mean,
there was an actual fire, and the mandatory evacuations that were ordered were
close enough to have me putting my “go bag” by the back door and putting the
dogs’ collars on and their go bags in the car. But we didn’t have to evacuate,
and the fire crews got the fire subdued within 48 hours of its eruption, so
that was all good.
However, I had the opportunity to help another friend who did have to evacuate, and we learned a
few lessons together.
Lesson #1: Always Have Backup Phone Numbers
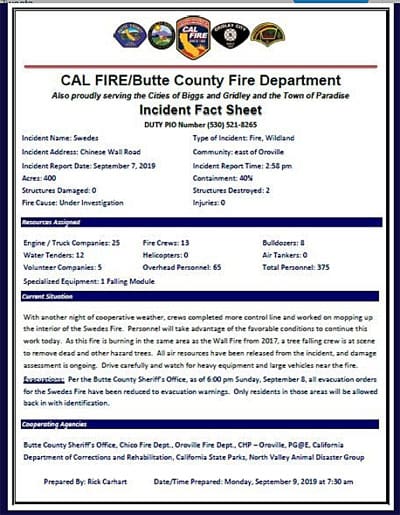
When I saw the location of the fire on the maps published by
Cal Fire (the fire-fighting agency that responds to all fires in California
that happen in the spaces between other fire-fighting jurisdictions) on
Twitter, I texted my friend Dorothy right away; she was right in the path of
the thing. No response. Then I called her. The call went straight to voicemail.
Lesson number one: Have backup phone numbers! I have only her cell phone
number, not her home phone number, and she only carries her cell when she’s not
home. So, knowing that ahead of time as I did, I should really have made more
of an effort to get her home number programmed into my phone.
I decided to head to her house. Already, there were
California Highway Patrol cars parked in the area, blocking access to a number
of roads near her – but fortunately her road was still accessible.
As I pulled my car into the front of her house, she was just
getting out of her own car. It turns out that she had just gotten home from a
long day out of town and was scrambling to catch up to the whole situation (and
she never turns her phone on when she’s driving). She heard about the fire on
the radio as she was driving home, and heard that there were mandatory
evacuations on roads very close to her home. I gave her a hug and said, “Tell
me what I can do.”
I should probably mention that my friend is 80 years old.
She’s a very active 80-year-old; in
fact, she is my horseback-riding buddy. She has three horses and still competes
in endurance races. But she also has a 92-year-old husband who is not quite as
active and able as she is, three cats, and one not-very-well-trained dog. We
had some work to do.
The good news: Her horse trailer is always hooked up to her
truck and ready to roll. It contains a dressing room that has a place for
humans to sleep and a miniature kitchen and bathroom, so the cats and dog and
humans can camp out in the there, too. The bad news: It’s a two-horse trailer
and she has three horses.
She told me that she would send her husband to a friend’s
house to stay. She could use some help to clean out a dog crate for the cats,
and to get some feed for the horses and halter them. She would look for the
cats and get her own things together. She said, “I can take the two horses to
Camelot (a stable, the evacuation site for large animals in our area), drop
them off, and come back.” OK, we had a plan.
Lesson #2: Always Have Important Addresses On Hand
I grabbed her dog, Maddie, who was already running around
barking at everything, and put her in my car. I figured Dorothy would be able
to catch the cats much more easily without Maddie underfoot. I filled up a
bunch of buckets with hay cubes, and put halters on the horses. I tried to
check Twitter, to see how the fire fighters were progressing, but I can’t get a
signal at Dorothy’s house.
I said, “Let me take Maddie to my house. I have a big crate
I can put her in. I will also get news about the fire and see if I can find
another spot in someone else’s trailer for the third horse. Then I will call
you on your cell, or text you anything important, so put your cell in your
pocket.” She agreed.
I can’t get a signal until I am about two miles from
Dorothy’s house. That’s why I got a little discombobulated when I reached
another friend who has horses and who might have been able to pick up Dorothy’s
third horse – and I realized I didn’t know Dorothy’s address, only how to get
there. Lesson two: Make sure you have the physical address of the people you
are trying to help!! I could neither ask Dorothy nor look at her street sign
nor the number on her fence. I explained Dorothy’s location to my friend on the
phone as well as I could, and said I would call her back and let her know the
address for sure. I hoped we wouldn’t need the ride for that horse, that
Dorothy had enough time to take two trips.
As I drove toward my home, I realized that I had recently
loaned the crate that I intended to put Maddie in to another friend, who was
out of town. Yikes! So I had to drive to that friend’s house, load the pieces
of crate onto the top of my car and tie it down (it’s a Great Dane-sized crate
made of flat panels that get fastened together in the corners with long rods),
and then drive home. Once there, I checked the fire maps online. They hadn’t
changed – but whether that was because the fire fighters were holding the line
or because the news hadn’t updated yet, I did not know. I texted Dorothy a few
times, with no response. I left Maddie in the big crate and headed back to
Dorothy’s house.
Lesson #3: Always Have Backup Keys
By now, it was pitch dark outside. But as I pulled into her
driveway, I could see that her husband’s car was gone; he had already left to
stay with their friends. And two of the horses were in the trailer, and the
cats were in the big dog crate, in the back seat of her crew-cab truck. Good,
good, good! But Dorothy looked distraught and was near tears. “I lost the key
to the truck!” she told me. “I had it with me, but now I can’t find it!”
Lesson number three: Always have a backup key to your
getaway vehicles!
With smoke hanging thickly in the air, we searched for
almost an hour. In her house. In the barn. Down the driveway. In the car. In
the cab of the truck, the back of the truck, the dressing room of the trailer.
I even opened the horse trailer door, where the horses waited impatiently and looked
around their feet, in case she had dropped the key while tying their halter
ropes. We were nearly in despair when I found the key in a place that Dorothy
had already looked: under the hay that she had thrown to the horse that we were
leaving behind. The horse had been eating this whole time, and the key and its
ring was nearly buried in the dirt and picked-over hay, but I have never been
so happy to see a glint of metal in a horse’s food in my life.
As I write this, days later, Dorothy and I have had a
discussion about our little fire drill. I have put her address and home phone
number into my phone. She is having a spare key made for her truck, and is
going to hide it in a location in the barn that she will disclose to her sister
(who lives nearby and also has horses) and me. We both are going to post a “to
do” list of things that we don’t want to forget in the event of another
evacuation or emergency. (She forgot a cell phone charger and her
prescriptions, which fortunately weren’t absolutely needed to survive for the
two days she stayed evacuated. When I went to her house in the dark, I forgot
the flashlight that sits next to my back door, and nearly ran my cell phone
down to zero battery by using its flashlight function instead. Dumb!)
Important Emergency-Preparedness Link
Here in rural Northern California, wildfire is always going
to be a possibility, so all of us in this situation have to keep an evacuation
plan in mind – for ourselves and for all of our animals. In other parts of the
country, you may have to be ready for other natural disasters: hurricanes,
tornadoes, earthquakes, floods, avalanches. Even those who live in cities
should have a go-bag packed and ready with certain items, and a checklist of
things to take along in case of a disaster. I can tell you that there is a huge
difference between how much you will forget when you are thinking about it
right now, while you read this in comfort and security on your computer or
tablet, and how much you will forget if you are in the dark with the smell of
smoke swirling all around and your beloved pets and family counting on you to
get it together. So let this be my annual reminder to you! Make a checklist!
Put together a go-bag! Update your phone and address book!
Here are some emergency-preparedness links I hope you find
helpful:
https://www.ready.gov/build-a-kit
https://www.aspca.org/pet-care/general-pet-care/disaster-preparedness
https://www.cdc.gov/healthypets/emergencies/index.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Ffeatures%2Fpetsanddisasters%2Findex.html
https://www.fema.gov/media-library-data/1553273223562-797451b5cb0bee8d35d3e4e85e3830d6/Checklist.pdf
https://www.fema.gov/media-library-data/1555704332614-dd584fec0c9724656c0292313bcd5da6/Important_Documents_for_FEMA_Assistance.pdf




















![scout2[1]](https://cdn.whole-dog-journal.com/wp-content/uploads/2019/08/scout21-696x520.jpg.optimal.jpg)










 starting with a favorite toy. Rub the toy on the paper towel, and start back at Step 1, placing the toy in plain view and move quickly through to Step 5.
starting with a favorite toy. Rub the toy on the paper towel, and start back at Step 1, placing the toy in plain view and move quickly through to Step 5.