- Hot Dogs
- Beyond Animal Welfare
- Mast Cell Tumors
- Take a Hike
- Word Up!
- How To Get The Tick Out
Download the Full July 2019 Issue PDF
Keep Your Dog Safe from Accidents
In a 48-hour period last weekend, three dogs who are very close to me ended up in veterinary emergency rooms. It was a very weird aggregation of events – but each event was avoidable, and each dog’s owner has taken responsibility for their dog’s potentially deadly accident.
Beware of Wild Animals Around Your Property
The first accident happened to Daisy, my sister’s little 15-pound Jack Russell Terrier. My sister and her husband live in a rural area, where most of the homes are on lots of a half-acre or more. In addition, they live at the bottom of a steep hill, on a court with just five houses on it, and several empty lots. She sometimes allows her little dogs to potty in the empty half-acre lot next door to her house. The lot is, like her own backyard, studded with oak trees, but unlike her yard, is covered with tall grass, and the little dogs enjoy sniffing and exploring the area as they take their potty break.
On this particular day, though, what my sister failed to notice as she let the dogs wander into the lot, was a female deer apparently lounging at the back of the lot. She didn’t see the moment that two of her dogs discovered the deer – or whether the deer spotted the dogs before they spotted her. But she heard one of her dogs shrieking and as she ran in the direction of the screams, saw a large female deer rearing up and stomping down on one of her little dogs.
Like many of us, she was focused on getting to and protecting her dog, and failed to appreciate the danger to herself as she ran toward the deer. She said she was yelling, “Hey! Hey!” and about 15 feet from the deer, fully expecting the deer to spook and run from her, when it, instead, reared up and charged at HER. She screamed and waved her arms and dodged behind a tree, and fortunately, little Daisy took that opportunity to bolt away from the deer. My sister, too, turned and ran and, again, fortunately, the deer didn’t pursue either of them. I suspect that she had a baby resting nearby or some other reason to go on the offensive. My sister didn’t investigate further, as Daisy was still screaming – now in pain, rather than from fear. The deer’s hooves had made one very deep and long laceration along Daisy’s flank, and her face was bleeding, too.
A night in the ER, x-rays, pre-anesthetic bloodwork, surgery (under anesthesia) to close the laceration and insert a drain, antibiotics, and pain medication: $1,600. Nope, they don’t have pet insurance.
Don’t Leave Out Food Leftovers or Dirty Dishes

The very next morning, I received a call from a friend regarding her dog Nova, who was my favorite puppy from a litter I fostered last fall. (I used her and Nova to model for an article in WDJ not long ago, you can see them here.) She said, “I just need a little support. I am at the ER with Nova and scared!” It seems she had made barbequed ribs the night before, and had left the glass pan, covered with baked-on sauce, on the stove top, to deal with the next day. In the middle of the night, Nova had apparently knocked the pan onto the kitchen floor, where it shattered into hundreds of pieces – and she spent some time licking the sauce off of those pieces of glass! There was broken glass – and blood – all over the kitchen floor. My friend didn’t hesitate; she just put Nova into the car and drove straight to the emergency clinic.

The attending veterinarian used an endoscope (under full anesthesia) to examine Nova’s esophagus and stomach, and removed several pieces of glass – as well as several pieces of chewed-up tennis ball. She was incredibly lucky; the procedure took place quickly enough that Nova hadn’t yet vomited (which could have made the glass cause damage on the way out of the stomach and in Nova’s throat), nor had the glass hadn’t started to move through Nova’s intestines. The blood that her owner saw on the kitchen floor was definitely caused by cuts the glass made on Nova’s tongue, but none of those cuts (nor others in her esophagus) were serious enough to require surgical repair.
Total cost: $2100. Fortunately, Nova’s owner has pet health insurance. Since she had another vet visit earlier this year and has already spent the $250 deductible for 2019, she will receive a reimbursement from the insurance company for 90 percent of the most recent bill.
Nova’s owner reports: “I have learned my lesson; my counters are the cleanest in the county and there won’t ever be a mistake made like this again. Also, no more tennis balls for Nova.”
Another Counter-Surfing Case
The same afternoon that my friend was picking up Nova after her procedure, I received a text from another friend! “Ricky ate Chaco’s pain meds. We are at (a local vet clinic).”
While ALL medications should be kept in kitchen or bathroom cabinets – never on counters that dogs can reach – this is especially true of chewable medications. Most dogs won’t eat more than one nasty-tasting pill they find lying around. But the chewable kind tempts many dogs into eating the whole bottle – and that’s what Ricky did. He ate about eight Deramaxx pills, a nonsteroidal anti-inflammatory (NSAID) that can cause liver damage if an overdose is consumed.

Again, fortunately, my friend discovered the chewed-up, empty bottle right away, and drove immediately to a veterinary hospital, where they administered an injection of apomorphine, which makes dogs almost instantaneously vomit. So Ricky has (apparently) suffered no ill effects, and the bill was a quite reasonable $170 (no insurance).
We’re All Susceptible
Lest anyone think I am judging my friends: I, too, once had a dog eat a whole bottle of chewable medication meant for another dog (I wrote about that in 2013!). The experience made me VERY careful about where I put medications.
Protecting our dogs is an ongoing, complex task, and none of us can prevent every potentially fatal accident. But all of these were preventable – and my sister and friends and I all hope that these stories make you just that much more alert and able to prevent any of these accidents from befalling your dogs!
In case you want to learn about more ways to avoid a trip to the veterinary ER, here is a link to an article that veterinarian Catherine Ashe (who practiced emergency veterinary medicine for nine years) wrote for us last year.
How to Get the Tick Out

It’s creepy enough that there are billions of these tiny insects living in the woods and fields, just waiting to latch onto your dog (or you!) and suck your blood. Bloating themselves with blood, ticks expand in size exponentially before falling off, able now to reproduce – gross! Add in the fact that a certain percentage of ticks may also infect your dog (or you!) with a disease that can cause pain and suffering for the rest of his life – that’s beyond creepy. I lack words to describe the sheer perniciousness of this insect’s survival strategy.
Most of us are aware that ticks can be infected with the spirochetes (microscopic bacterial organisms) that cause Lyme disease (for more information, see Lyme Disease in Dogs, WDJ October 2018). But, depending on what part of the country you live in, the ticks around you may carry any number of other spirochetes that cause other painful diseases, such as Rocky Mountain spotted fever, anaplasmosis, babesiosis, ehrlichiosis, and more.
Parasites in Parasites
These spirochetes are parasites of the ticks themselves! Ingeniously, they use ticks to help them move from one host to another. When a tick sucks blood from an infected mammal, bird, or reptile (common hosts include mice, chipmunks, deer, birds, and lizards) the spirochetes come aboard and set up shop inside the tick; when the infected tick bites its next host, the spirochetes slip into the new victim through the tick’s saliva. The longer the tick feeds, the longer the spirochetes have to infect the tick’s newest host.
Not all ticks carry the spirochetes that cause disease in mammals. The rate of their infection varies by geographic location, species and life-stage of the tick, and species of spirochete. Most prevalent is the species that causes Lyme disease, Borrelia burgdorferi. In southern New England – the epicenter of Lyme infection – about 20 to 30 percent of tick nymphs and 30 to 50 percent of adult ticks are infected with B. burgdorferi. In other parts of the country, B. burgdorferi may be found in fewer than five percent of ticks.
How to Protect Your Dog
To protect your family members from tick-borne disease, then, your job is two-fold: Do everything that you can to keep ticks off of your dog, and quickly find and remove any ticks that do manage to climb aboard.
We’ve discussed oral and topical pesticides that are fed to or applied to dogs to kill ticks in other articles (see Prescription Flea and Tick Medication, WDJ September 2017). But it’s clear to anyone who uses prescription or over-the-counter medications or spot-on products, tick collars, essential oils, or anything else, that no matter what you use, some ticks will manage to climb aboard and bite your dog. So let’s talk about the second tactic for protecting your dog from tick-borne disease: Getting the ticks off your dog ASAP.
How to Remove Ticks
I have heard countless methods for tick removal: Paint a tick with nail polish and it will detach from the dog to avoid being suffocated. Touch a just-extinguished match to the tick’s body so it pulls itself out. Pull while turning the tick clockwise. No – pull while turning counter-clockwise! All of these tactics are ineffective; don’t do any of them!
It’s actually quite simple: Just try to get a good grip on the tick, as close to the dog’s skin as possible, and pull it straight out.
Note that I said simple, not easy. Ticks are tiny. Your dog may be squirming. If his coat is thick, it might be hard to isolate the tick in your grip. You may end up pulling, or being impeded by, his hair, too. And if your fingers are thick, you run the risk of squishing the tick between them as you pull, which can result in squeezing the contents of the tick’s mouth and guts into your dog! Ack! That actually increases the chance of infecting your dog with any disease-carrying spirochetes that the tick might be hosting!
Tweezers can be used more effectively than your fingers, but they, too, pose the risk of squeezing the tick and squirting that potentially pathogenic-filled tick spit into your dog’s body.
Instead, use a tick pulling tool with a V-shaped slot. Slide the tool between your dog’s skin and the tick’s body, wedging the tick’s body into the tightest part of the tool’s crevice. When you feel that the tick is securely lodged in the slot, pull upward on the tool and – pop! The tick comes right out.
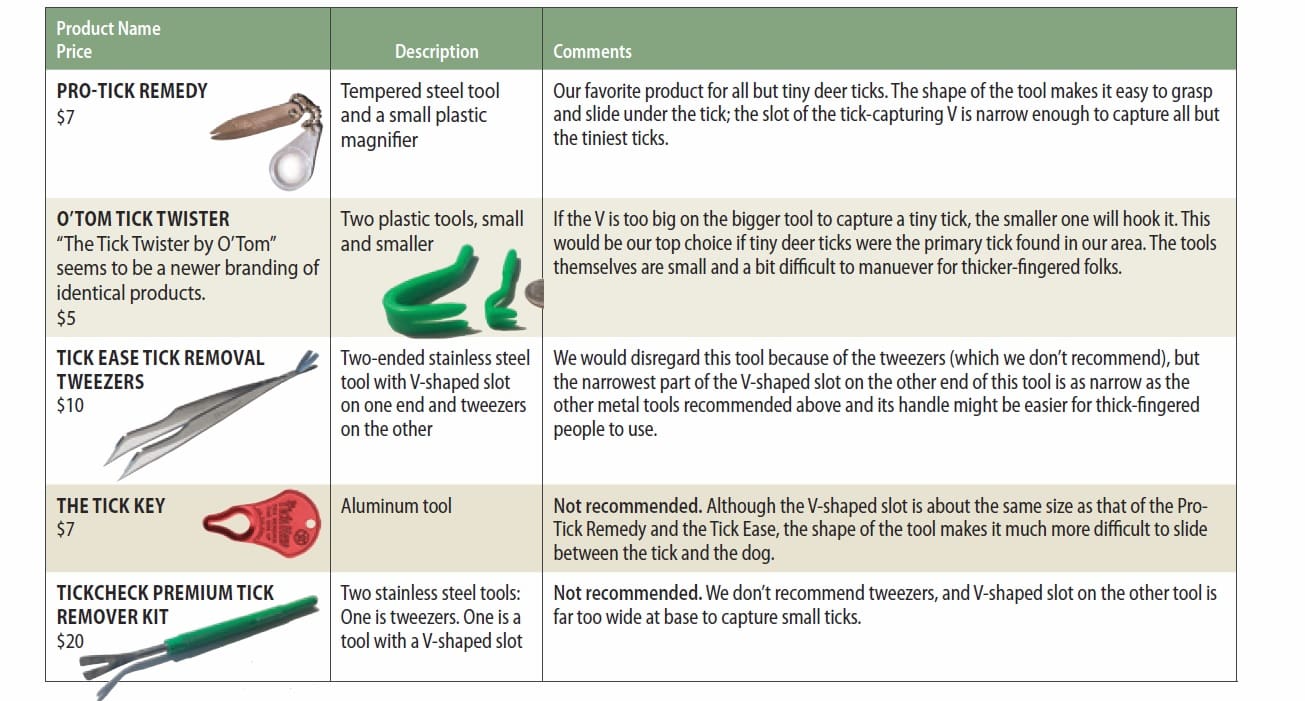
Tick Tool Time
There are any number of tick-pulling tools on the market. Many of them are basically tweezers. They may have longer stems or sharper points than tweezers meant for other purposes, but they all pose the risk of squeezing the tick as you grasp it hard enough to pull it out.
The superior tools for this purpose all have the V-shaped slot that you wedge the tick’s body into, effectively using its … shoulders? … as leverage for when you pull.
The best tick-pulling tools have a few specific attributes that increase their effectiveness:
- They are made of a strong yet thin material. The tool has to be thin enough to slide between the tick’s body and the dog’s skin, along both sides of the tick’s … neck?
- They are possessed of a V-shaped slot that is narrow enough at the bottom of the V to trap and leverage against the narrowest of tick … shoulders? (The tick’s body, basically.) If the V is not vanishingly narrow at the bottom, the tool won’t capture the tiniest ticks.
- They are of a size and shape that is easy for even thick-fingered people to grasp securely and that can be slid under the tick’s body easily.
We tested several tick-removal tools with V-shaped slots, and our favorites are described below. We purchased all of these products on Amazon.com. We like to support local pet supply stores, but these products are rarely found in stores.
How to Teach Verbal Cues

Does your dog understand what behavior you wish her to perform when you use verbal cues alone, with absolutely no hand gestures or suggestive body language? In many cases, the body-language picture we present to our dogs tells them as much – or more – about what we expect them to do as our verbal cues do.
In fact, it’s pretty common for dogs to be unable to perform the behavior that their owners are sure they know upon hearing the verbal cue alone – for example, if the owner’s back is turned to the dog when he gives his dog the verbal cue.
There are many compelling reasons to strengthen our dogs’ knowledge of and response to verbal cues – not least of which is that there are actually times when it would be helpful for our dogs to perform the behaviors we want when our back is literally turned!
The stronger their understanding of and response to our verbal cues, the more likely it is for our dogs to respond to those cues in situations where we look different, such as when our hands are full, we are sitting down, we are keeping our eyes on an approaching dog and/or person, or when our dog can’t see us because he’s darting toward the delivery van pulling in the driveway.
How to Teach a Verbal Cue
By helping your dog make an association between your verbal cue, the desired behavior, and the delivery of a resulting reinforcer (such as a food treat), you teach your dog how to respond with the appropriate behavior when you ask for it. You are giving him a choice: the opportunity to be reinforced for performing a particular behavior, or not. If he chooses “not,” then your job is to figure out how to help him want to choose to do the behavior.
First, you will properly introduce the cue and help him understand what it means. While there are several different ways to do this, we’ll walk you through the process with a couple of basic behaviors using one of our favorite training techniques: the lure-reward method. The steps are:
1. Get the behavior. Encourage the dog to do the behavior by using a treat as a lure to explain to him what you want. When he does the behavior for the lure, “mark” the moment that he does the desired behavior (with the click of a clicker or a verbal marker, such as the word “Yes!”) and give him a treat. (Note: For some dogs and/or for some behaviors, you may need to lure/shape – marking and giving treats for pieces of the behavior until you build the final behavior. See “Shaping Your Dog’s Behavior,” WDJ January 2017.)
2. Add the cue. When your dog will easily offer the behavior for the lure, use your verbal cue just prior to luring the behavior. You are essentially explaining to him, “This word means the same thing as this luring motion I’ve been doing.” Continue to mark and treat as appropriate throughout the process.
Your dog training reward marker doesn’t need to “click”
A clicker is a small device that makes a consistent, distinct clicking sound. Some make a very sharp sound; some make a softer (though still consistent) clicking sound, like the sound of a ballpoint pen being retracted or extended with the press of a button. But markers don’t have to be a click; any distinctive, consistent sound, gesture, or event can work.
I sometimes use the verbal marker “Yes!” with dogs, in a distinct, consistent, bright tone of voice. I have also perfected a loud “mouth click” by suctioning my tongue to the roof of my mouth and pulling it off with a resounding “pop” – very useful when working with horses and I want both of my hands free to handle a 1,000-pound animal and related equipment. Dogs who are sound-sensitive may do better with a verbal marker than a plastic clicker.
But the marker doesn’t have to be a sound! People who train deaf dogs often use a thumbs-up gesture or a momentary flash of a small flashlight to mark the desired behavior displayed by their canine students. Any signal that is consistent and easily noticed can work as a reward marker.
3. Add a pause. After several repetitions, pause for a few seconds after you say the cue, to give his brain a chance to process the word; then lure the behavior. (“Several” will vary from dog to dog. Some dogs will get it quickly; some dogs need more repetitions to understand the process. You will come to know how many repetitions is appropriate for your dog.)
4. Vary the pause. As you proceed with cue-pause-lure, begin to vary how long you wait before you lure. Sometimes, use the lure after just a second or two; sometimes wait several seconds. Luring quickly keeps him from getting frustrated. Waiting longer before you lure gives him more time to think.
5. Reinforce offered behaviors. At this point, some dogs will begin to offer the behavior before you lure. If yours does, the first time he does it, mark, treat, and party! Tell your dog how brilliant he is, give him several treats (or a special high-value treat you’ve saved for this occasion), and give him a break before you try again. Know that just because he did it once doesn’t mean he will do it every time – you may still have to do some cue-pause-lure repetitions, but it means you are well on the way to getting the behavior “on cue.” Congratulations!
6. Fade the lure. Some dogs won’t begin to offer the behavior so easily, which means you will need to “fade” the lure. This means you will continue to cue-pause-lure, but gradually decrease the amount of luring help you give him.
For example, if you were moving the lure six inches, try moving it just four inches; if he commits to finishing the behavior, whisk the lure away, mark the completion of the behavior without the treat in front of his nose, then give him the treat.
Also, be conscious at this stage that you do not inadvertently use other body-language hints or “prompts” to help your dog do the behavior, such as moving a hand toward the floor for the “down.” If you do use these prompts, you will have to fade them later to have the behavior truly on verbal cue alone.
Continue with your repetitions, fading the treat more and more, until your dog will reliably offer the behavior without the lure. Congratulations!
Note: Notice that I do not use “air cookies” – pretending to lure but not actually having a treat in your hand. To me, this is lying to your dog, and you still have to fade the “air cookie.” You might as well just skip this extra step and move right to fading the lure.
Verbal Cue for “Sit”
Sitting is one the most basic of canine behaviors. It’s an easy behavior for most dogs to do, and a great “incompatible behavior” to ask for when you don’t want your dog doing something else, such as jumping up on people. It also can become a useful “default” behavior – the behavior you teach your dog to offer when he’s not sure what else to do, or when he’s asking for something – like, your attention or his dinner.

Here’s how to teach your dog a verbal “Sit” cue using this process.
1. Get the behavior. Do not use your verbal “Sit” cue for this step. Simply use a food lure to encourage your dog to sit, by placing it at the tip of his nose and slowly lifting up a little. (If you go too fast you will “outrun” him and he will lose his connection to the lure.)
With some dogs you can move the treat back over the head a little; other dogs will find this aversive and back away from you. Experiment a little by moving the lure in different places – back a little, forward a little, up a little more, up toward your chest – until you find the place that invites him to sit.
If he doesn’t lure into a sit fairly easily, lure/shape it by marking and giving him a treat him for any upward head movement that follows the treat, and for any lowering of the hindquarters, until he is all the way in a sitting position.
2. Add the cue. When your dog will sit easily for the lure, it’s time to add the cue. Say “Sit!” in a cheerful tone of voice (remember, it’s an invitation, not a command!), and lure him into a sit position. Repeat this at least a half-dozen times. Continue to mark (with the click of a clicker or a verbal marker, such as the word “Yes!”) and give him a treat for sits throughout the process.
3. Add a pause. Now say “Sit” in a happy voice and pause a few seconds. If he sits, mark and treat and party – you have a canine genius! More likely he won’t sit for just the cue yet, so after two to three seconds, lure him to sit, then mark and treat. Repeat several times.
Cue the cues
Today’s force-free dog training professionals increasingly use the word “cue” rather than “command” to describe the communications we give to our dogs when we want them to perform a behavior. Here’s why:
The word “cue” typically refers to a signal that encourages someone to take an action. A cue informs your dog that there is an opportunity for him to receive a reinforcer (such as a yummy treat) for performing a particular behavior. Compare that to the word “command,” which means to give an authoritative or peremptory order. The implication when you give a command is, “You better do it, or else!”
The words we use are important. They inform our mental associations and physical responses. As philosophically positive as a person might be when she is training her dog, if her brain thinks “command,” she is likely to use a more forceful tone of voice and more dominating body language. She might even be tempted to physically coerce her dog into position, albeit gently, if she perceives that her dog has “disobeyed” her command.
In contrast, a trainer whose brain thinks “cue” is more likely to use a lighter tone of voice, softer body language, and to examine why her dog declined the opportunity to earn a reinforcer. Perhaps he was distracted, didn’t understand, hasn’t yet generalized the behavior to a new environment, has a prior aversive association with the cue, or has a medical issue of some kind that makes it painful when he tries to perform the behavior.
Keep in mind that it is our job, as the supposedly more intelligent species, to be able to get the dog to want to do what we want him to do, rather than just force him to do it!
4. Vary the pause. Continue to “Sit”-pause-lure, but now, start to vary how long you pause before luring to give your dog’s brain time to process the information and respond. Sometimes lure after just a one-second pause, sometimes two to three seconds, and sometimes wait as long as five or six seconds.
5. Reinforce offered behaviors. Some dogs will begin to offer sits at this stage with the longer pauses. Mark and treat and party!
Continue to repeat this step, and remember that he may still need some luring. Just because he sits in response to the cue sometimes without luring doesn’t mean he fully understands.
Repeat this step until he responds to your verbal “Sit” cue without the lure 80 to 90 percent of the time. At that point you can say he knows the cue – and you may still need to assist with your lure from time to time when he doesn’t respond due to the cue. (None of us are perfect!) It’s better to lure when needed than to repeat the cue and risk “learned irrelevance,” where the cue loses its meaning. Sometimes even very well-trained dogs need a little help to get it right!
6. Fade the lure. If you have one of those dogs who just doesn’t get it with the cue-pause-lure step, you will need to fade the lure. Give him your cheerful “Sit” cue, pause, and begin to lure. As soon as he appears to be committed to sitting, whisk the lure out of sight behind your back and let him finish the sit without the lure in front of his nose. (If you keep the treat in view, he may try to follow it!) Mark and treat. Gradually lure less and less, whisking the treat out of sight sooner in the sit sequence, until, lo and behold, you don’t have to lure at all. Mark, treat, and party!
We’re Down
We start to teach “Down” as soon as we can easily lure our dog into the sit position, even if “Sit” isn’t yet reliably on verbal cue. It can be a more challenging behavior for many dogs than the sit, but the same procedure works.
1. Get the behavior. Do not use your verbal “Down” cue for this step. Simply use your lure to encourage your dog to lie down, by placing it at the tip of his nose and slowly moving it straight down toward the floor.

Some dogs will follow the treat straight to the floor and lie down the first time you lure, but most need a little lure/shaping here: move the treat down a little, mark and treat. Move it down a little more, mark and treat. Continue to lure him a little farther each time until he is all the way down.
If he stands up, you may have moved the lure too far, too fast, or moved it away from him rather than straight toward the floor and he got up to follow it. Try again, with smaller increments, and make sure the treat is moving straight toward the floor.
2. Add the cue. When your dog will lie down easily for the lure, it’s time to add the cue. Say “Down!” in a cheerful tone of voice (invitation, not command!), and lure him into a down position. Repeat this at least a half-dozen times. Continue to mark and give treats for downs throughout the process.
3. Add a pause. Now say “Down” in a happy voice and pause a few seconds. Make sure you have the treat in a neutral position at your side or behind your back. If you hold it up at your chest, you are giving your dog a body language signal to sit. Because dogs are primarily body language communicators, he will likely pay more attention to your “Sit” signal than your verbal “Down” cue.
If he lies down when you say the cue, mark and treat and party – you have a canine genius! More likely he won’t lie down for just the cue yet, so after two to three seconds, lure him to lie down, then mark and treat. Repeat several times.
4. Vary the pause. Continue to “Down”-pause-lure, but now start to vary how long you pause before luring. Sometimes lure after just a one-second pause, sometimes two to three seconds, and sometimes wait as long as five or six seconds.
5. Reinforce offered behaviors. Some dogs will begin to offer downs at this stage with the longer pauses. Mark and treat and party!
Continue to repeat this step, and remember that he may still need some luring. Just because he lies down in response to the cue without luring sometimes, doesn’t mean he fully understands. Repeat until he responds to your “Down” cue without the lure 80 to 90 percent of the time. Remember, it’s better to lure as needed than to repeat the cue and risk “learned irrelevance,” where the cue loses its meaning.

6. Fade the lure. If you have one of the many dogs who just doesn’t get it with the cue-pause-lure step, you will need to fade the lure.
Give him your cheerful “Down” cue, pause, and begin to lure. As soon as he appears to be committed to lying down, whisk the lure out of sight behind your back and let him finish the down without the lure in front of his nose. Mark and treat. Gradually lure less and less, whisking the treat out of sight sooner in the down sequence, until, lo and behold, you don’t have to lure at all. Mark, treat, and party!
Another Language
You can use this same process to put many different behaviors solidly on verbal cue. First get your dog to do the behavior, then add the cue, then fade the lure. It is very important to begin fading the lure as soon as he will reliably perform the behavior so that your dog and you don’t become dependent on the presence of the lure to make the behavior happen.
We are a verbal species, and while it is critically important for us to understand our dogs’ body language communications, there is something quite compelling about helping our non-verbal canines learn our language. It is very gratifying – and incredibly valuable for strengthening the dog-human bond – when your dog understands and responds to your verbal cues. Just decide what behavior you want on verbal cue, and get started!
Take a Hike! (With Your Dog)

I love hiking with my dogs, and one of my favorite things about living in the Pacific Northwest is the abundance of dog friendly hiking trails available to us. Over the years, I have learned a great many things about how to take a safe and enjoyable hike with dogs – some things that you really should do, and some things that you really should not do. Here are 10 tips for ensuring a great time for all involved.
Safety
Being out in nature is a great way to relax and connect with your dog, but it’s important to think about safety. With three dogs of various ages, sizes, and abilities (from 2 to 17 years old, 10 pounds to 103 pounds, and one dog with two surgically reconstructed knees), I take a lot of precautions to ensure everyone’s safety when we hit the trails.
1. All of the normal safety precautions for hiking in general apply to hiking with dogs – and then some. Tell other people where you are going and when you will be back. Monitor weather conditions. Be realistic about your own skill and fitness level. Carry trail maps; don’t just rely on your phone, as GPS signals might not work in the backcountry. Turn back early so you are back before dark. Don’t approach wild animals. Carry a cell phone (though, again, be aware you may be out of signal range). Carry water.
When you’re going with a dog, do all of the above, and carry extra water for your dog, and allow yourself give extra time for the hike.
Also, monitor weather conditions to ensure temperatures aren’t too hot for your dog to safely hike. Because (unfortunately) the general public can’t always be trusted to make good decisions for their dogs, the city of Phoenix, Arizona, piloted a program that banned dogs from hiking on trails when the weather is 100 degrees or more. People caught with dogs on the trails in those temperatures can be fined or jailed. The program took effect after multiple dogs died while hiking in the Phoenix heat.
2. Be realistic about your dog’s abilities, and aware that they can change. “The dog’s general health and athleticism should be considered before planning a hike,” says Stacey Rebello, DVM, medical director of emergency services at NorthStar Vets Veterinary Emergency Trauma & Speciality Center in New Jersey. “And the duration and length of the hike should be adjusted to ensure the pet can tolerate it.”
On your hike, watch for symptoms of tiring. Turn back before injury or exhaustion occurs. Signs that your hiking plans need adjustment include an adolescent dog who has more energy than stamina or a senior dog who has a hard time keeping up. Any dog who seems to be over-tired the next day or has difficulty recovering from the hike needs more conditioning before attempting that hike again.
I’ve found that trails rated as a good match for hiking with children work well for most dogs.
Leash Laws
Although many people like hiking in naural settings with their dogs off-leash, this is not allowed in many areas, including most state and national parks.
3. Be sure you know the regulations that govern trail use by dogs for any area you plan to hike with your dogs – and follow them! Some dog owners believe that their dogs are so well trained that they should be allowed to hike off-leash; however, leash laws exist to keep everyone safe, including the leashed dogs, other trail users (canine and human), and wildlife.
Following leash laws also helps ensure that you and your dog will be able to hike again another day. If people can’t be trusted to follow rules and keep their dogs leashed to protect wildlife and fragile vegetation, more wilderness areas will ban dogs all together.
Also, be sure to doublecheck that dogs are allowed on the trails at your planned hiking location before leaving your house. Dogs are allowed in many national parks – but are often restricted to campgrounds (not allowed on trails), and must be in the company of one of their owners at all times. When researching dog-friendly trails, I find local websites are better than hiking guide books; they are more frequently updated with information about current trail conditions or regulations.
4. In areas where dogs are permitted to be off-leash, take your dog off-leash only if he isn’t a danger to himself or others. Just because you hike in an area where dogs are allowed to be off leash doesn’t mean you should remove the leash, says Cincinatti dog trainer Nick Hof, a Board member of the Association of Professional Dog Trainers. “If your dog is off-leash in a permitted area, your dog should have excellent recall skills and be good with any other people or dogs you come across,” Hof says.
BARK Ranger Program
In 2015 the National Park Service began a new program to work with responsible dog lovers to find ways to make national parks more friendly to dogs while protecting their fragile ecosystems. The BARK Ranger program was piloted in Washington’s Olympic National Park. The program was expanded to Montezuma Castle National Monument in 2016 and is now at many national parks nationwide. The program offers structured activities like guided hikes with dogs and the opportunity to get official park gear for your dog.
BARK stands for:
Bag your dog’s waste
Always use a leash
Respect wildlife
Know where you can go
Participants in the BARK Ranger program take a pledge to follow park guidelines to be good examples and good ambassadors in the parks.
Some parks allow dogs and their owners to volunteer as BARK Ranger Ambassadors, making contact with national park visitors and their dogs to ensure everyone has a safe and enjoyable visit. The goal of the Ambassador program is to reduce the number of non-compliant dog incidents in the parks and increase awareness about park rules and training. The teams receive training on how to approach visitors, thank them for following park rules, and request that they comply if they aren’t. BARK Ambassadors also receive special vests for the dogs and t-shirts for the handlers and have scheduled volunteer shifts in the park.
To learn more about what parks near you offer BARK Ranger programs, visit nationalparkpaws.com/the-bark-ranger-program/. If your local park isn’t listed, call the park’s ranger station and let them know you would participate in a BARK Ranger Program if one were started. The National Park Service looks for interest from dog owners to decide where to expand the program next.
“Remember, when you take your dog off-leash in an unsecured area, you are betting his life that you can predict how he will handle any situation and feel confident that you all will succeed,” says Hof.
Hof advises for leashed and unleashed dogs to practice the occasional recall, reinforcing prompt responses generously. This reinforces not only the dogs’ recall but also that hiking near you is rewarding.
Trail Etiquette
If you have found an enjoyable place to hike with your dog, the odds are that other trail users appreciate the area, too. Be sure you are the trail user that others enjoy seeing – or at least, don’t notice!
5. Always be courteous to others and to nature when you and your dogs are out on the trail. Be sure to bring plenty of poop bags with you and pick up after your dog.
It can be tempting to let your dog go crashing through the underbrush, but this is disruptive to the plants and animals. Teach your dog that part of hiking is staying on the trail.
Keep in mind that not everyone likes dogs or wants to greet them on the trail. It’s not acceptable to let your dog approach another dog or person without the person’s permission or invitation.
6. Share the trail! Keep your dog close to you when hiking. Whenever possible, I put myself between my dog and other hikers to protect everyone (I’ve actually had a hiker reach out and grab my dog’s tail while doing an unsolicited “drive by pet”).
If you are on a trail that also allows horses, be sure to bring your dog close to you, giving extra space to the horses. Be aware that a dog who jumps up or barks at a horse might spook the horse – and that some some dogs may be spooked by horses! A dog who bolts away from the horses in fear may cause the horses to spook in turn, so unless you know that your dog will be calm and unafraid, put even more space between him and any equestrians.
Similarly, mountain bikes are common on many hiking trails. Ideally mountain bikers will slow or even possibly dismount before biking past you and your dog, especially if a trail is narrow. But if not, be aware that bikes may startle some dogs, so keep your dog close and put yourself between your dog and the bike.
7. Don’t impose your dog’s “issues” on others. If your dog displays aggression or reactivity toward other dogs or people, “you should either be working on those issues or have a plan in mind for how to mitigate any issues that may come from those,” Hof recommends.
One of my dogs is a former street dog and she’s very reactive to other dogs, so we seek out trails in areas where all dogs are required to be on on-leash, and that have reviews indicating they are only lightly used. If we arrive somewhere and find that the trails are crowded, or that people are breaking the leash laws, we simply leave and find somewhere else to go. It’s just not reasonable to expect other people to anticipate that your dog poses a greater than average potential for aggression to them!
Gear
Good quality, comfortable gear can make or break a hike for us, and it’s no different for our dogs.
8. When getting ready to go hiking, it’s important to make sure that your dog’s gear fits and is in good condition. No half-chewed leashes or harnesses with frayed stitching! And the trailhead is not the place to fit gear for the first time! Check the gear and adjust it for his comfort at home.
“I almost always prefer harnesses to collars for leash attachment,” Hof says. Note that harnesses have more contact with the dog and so pose a greater risk of rubbing and causing a raw, sore spot. Check your dog frequently when he’s wearing new gear, especially in sensitive places that are hard to see as you walk along – under his elbows, for example.
If you want your dog to carry a pack on your hikes, be sure to start slowly. It’s a good idea to visit to your veterinarian to ensure your dog is structurally sound enough to carry a pack. Also talk to your vet about what amount of weight would be appropriate.
Conditioning
In addition to choosing the right trails to hike with your dog, you need to condition him slowly to keep him from getting sore or injured.
Dog Scouts of America
Dog Scouts of America is a national scouting troop for dogs and their people, where dogs can earn badges for learning tricks and skills, including hiking. Kelly Ford, Leader of Dog Scout Troop 219 and a Dog Scouts of America Scoutmaster, says that there is an abundance of hiking badges and titles that can be earned by dogs and their owners. “The ‘Trails’ titles include backpacking, hiking, letterboxing, and geocaching with many achievement levels. Dog Scout badges include Backpacking and Hiking,” Ford says.
For dogs to earn the backpacking badges and titles, they must carry a pack with their own survival gear. To ensure safety, Ford says, “We stress the importance of keeping the packs lightweight, especially for our smaller Scouts.”
To earn hiking badges with Dog Scouts of America, dogs and their handlers need to complete a required number of miles and submit a log sheet. The first level of the dog hiking titles is 50 miles.
Being courteous and respectful is an important part of being a Dog Scout. “Polite trail behavior is always important in our Scouts. We also teach a ‘leave it,’ which applies to wildlife, roadkill, fish hooks, or anything on the trail that could pose a danger,” Ford explains.
“My dogs are always excited to go hiking with their Dog Scout Troop,” Ford says. “Their fellow Scouts ase are their best friends. Our Troop has learned a lot of new things and explored new places together.”
To learn how to get involved with dog scouting, see dogscouts.org.
9. Don’t force your dog to be a weekend warrior. Dr. Mandi Blackwelder, DVM, CCRP, owner of Healing Arts Animal Care in Beaverton, Oregon, cautions against taking our dogs along on infrequent and/or overambitious types of hikes. “They (and we!) are much more likely to be injured either during the hike or when we are sore afterward,” says Dr. Blackwelder. Instead, she advises that dog owners who want to start hiking begin a regular, structured exercise routine locally, long before making long drives to desinations for long hikes. “The first thing to do to prepare your dog for hiking is daily walks of increasing length, changing up terrain, and adding hills,” she says.
If you plan for your dog to wear a pack on the trails, you need to start conditioning her for that on your local walks, too. Start with an empty pack and slowly increase the weight (going no higher than what your vet advises) and length of time your dog wears the pack.
And when you do get to the trails, monitor your dog carefully. “Know your dog,” warns Dr. Blackwelder. “If she is a kamikaze hiker, be prepared to corral her before she is exhausted. If your dog is cautious, then work on some uneven terrain (rocks, gravel, bark) beforehand so you’re not forcing a march she is not ready for.”
Dr. Blackwelder offered the additional caution that it’s important to think about your dog’s specific structural or health needs. If your dog has preexisting health conditions, is overweight, or is a short-nosed breed, take additional precautions to prevent her from becoming overheated.
First Aid
Trying to prevent injuries should be foremost, but being prepared with a few essentials can be invaluable in case of an emergency on the trail.
10. Stuff happens, so prevent what you can and be prepared to deal with what you can’t. “Traumatic injuries, including abrasions, lacerations, and stick impalment are not uncommon when dogs are allowed to run through wooded areas. The risk of these types of injuries can be mitigated by keeping your dog on a leash and following an existing/established trail,” Dr. Rebello advises.
She advises that the most important thing to carry when hiking is water – to make sure dogs remain well-hydrated and to prevent overheating.
She also suggests carrying gauze and bandages. “If your pet is injured, the goal should be to get medical attention as quickly as possible. Spending exorbitant amounts of time on field first aid is less important than getting them to a veterinarian as quickly as possible,” Dr. Rebello says. “Rinse any wounds with clean water, apply firm pressure to stop bleeding, and place a temporary bandage until they can be assessed by a veterinarian.”
Dr. Rebello says “the biggest concern for owners who take their pets hiking is the risk of exposure to infectious diseases and parasites.” She advises dog guardians to ensure that their dogs’ tick preventatives are up to date before hiking, and to check their dog for ticks when they take breaks during a hike and when they get off the trail.
In addition, she warns dog owners to prevent their dogs from drinking from ponds, puddles, or streams on the trail that could be contaminated with leptospirosis; instead, bring enough clean water for you and your dog. And finally, “Owners should consider ancillary vaccinations for Lyme and leptospirosis for dogs who regularly go hiking, hunting, or live in highly wooded areas,” she says.
About Mast Cell Tumors in Dogs

Mast cell tumors (MCTs) are the most common form of malignant skin cancer that occurs in dogs, accounting for about 14 to 21 percent of all skin tumors. There is significant variability in the presentation of MCTs from dog to dog and even from tumor to tumor, which explains why this form of canine neoplasia is often referred to as complicated and challenging. But the fact remains that MCTs are treatable, and many dogs are considered cured after treatment and go on with happy, healthy lives.
How Mast Cell Tumors in Dogs Develop
Mast cells are a subtype of white blood cells that derive from the bone marrow and then become residents of specific tissues, especially those that are closest to the external surfaces of the body, such as the tissues of the nose, mouth, lungs, skin, and around blood vessels. Their primary functions include defense against parasitic infection, tissue repair, and formation of new blood vessels; they also play an important role in the allergic response system. They can be activated by the immune system – a process called degranulation – to release a wide variety of inflammatory mediators, including histamine and heparin, which in turn modify immune reactions and inflammation.
When mast cells replicate in higher than normal numbers, an MCT (also known as a mastocytoma) can form. They are usually first noticed on or just under the skin, but they can form anywhere on the body. The most common location is on the trunk, followed by the limbs and in between the toes; they can occasionally be found on the head and neck. The skin mass might appear as a raised lump or bump or growth; it can soft or firm; hairless or covered by hair; it may or may not be red, ulcerated, or swollen.
MCTs can also occur internally, developing on the spleen, liver, intestine, and in bone marrow, as well as on the salivary gland, nasopharynx, larynx, oral cavity, gastrointestinal tract, ureter, and spine. This type is more aggressive, and it is usually preceded by dermal and subdermal tumors.
MCTs can not only vary in location, appearance, shape, and size, but also have a tendency to present with varying clinical behavior, which is suspected to be influenced by breed. MCTs can even change in size (increasing and decreasing from day to day!) because of reactions occuring in the mass. This is due to secondary inflammation caused by the release of histamine, which then results in intermittent swelling.
This type of tumor tends to present in dogs of middle age or older, but can occur in dogs of any age. No gender predilection has been reported. MCTs typically present as a solitary tumor but about 11 to 22 percent present with more than one tumor and 10 to 20 percent of those that have had an MCT will develop a new MCT in another location at some point.
The Cause of Mast Cell Tumors
The cause of MCTs is unknown. Certain breeds of dogs are predisposed to them, so there may be some genetic component. A genetic mutation in the protein c-kit tyrosine kinase receptor – called a c-kit oncogene – is found in 25 to 30 percent of tumors. Chronic inflammation may also predispose dogs to developing the disease, such as dogs that have a history of allergic skin disease. There has been no association found between sun exposure and MCT in dogs.
Breeds With a Predisposition for Mast Cell Tumors
MCTs are over-represented in Pugs (at risk for multiple but low-grade tumors), Boxers, Labrador Retrievers (at increased risk for the more aggressive form), Golden Retrievers, Beagles, and Boston Terriers. Other breeds showing an increased likelihood of developing the disease include Schnauzers, Bullmastiffs/Bulldogs/ Bull Terriers, Cocker Spaniels, Fox Terriers, Weimaraners, Rhodesian Ridgebacks, Shar pei, and Dachshunds.
Diagnosis of Mast Cell Tumors
The initial evaluation of a suspected MCT begins with a fine needle aspirate and cytology, from which a diagnosis is usually made. Grading of the tumor cannot be done at this point as only cells are obtained from the aspirate; visual examination combined with the cytology report will determine if the MCT is a candidate for surgical excision.
It is reasonable to stage (evaluate how far the disease has spread) the tumor prior to surgery; in cases of a recurring tumor, multiple tumors, or evidence of metastasis, staging in advance is considered necessary.
When an MCT spreads, the cancer usually moves into the regional lymph nodes near the tumor, then to the liver and spleen; it can also spread to other places in the abdomen as well as to the bone marrow. At a minimum, the staging tests should include an aspirate of the lymph nodes near the tumor and an abdominal ultrasound.
The ultrasound can show if there is any evidence of metastasis or anything suspicious that requires further testing. Aspirates of the liver and spleen may be recommended, even if all the organs appear normal, because they may harbor cancer cells.
Treatment for Mast Cell Tumors in Dogs
The preferred treatment for MCTs is surgical removal – and for many cases, this is the only treatment needed. Prior to surgery and to alleviate some of the unpleasant symptoms of MCTs, a dog may be placed on antihistamines and antacids to mediate the effects of the histamine generated by the mast cells. Because MCTs are prone to growing into surrounding tissues, the visible tumor is removed with the addition of wide surgical margins – 2 to 3 centimeters on all sides, as well as layer of tissue below – in an attempt to remove all cancerous cells; as a result, the surgical sites can be quite large. If there is more than one tumor, a biopsy is recommended for each one because individual tumors can be of different grades and require different courses of treatment.

The excised tumor(s) will be sent to the lab for pathology; the resulting biopsy report will provide the tumor’s grade, confirm whether or not the tumor was completely removed (“clean” or “dirty margins”), and provide a foundation for prognosis. If the biopsy report shows that detectable cancer cells remain, the tumor can regrow. In these cases, a second surgery (if the site is amenable) or radiation therapy can be recommended. Mast cell tumors can be slower to heal post-operatively with suture sites that have the potential to break down.
If the location of the lesion disqualifies it as a candidate for surgery, further diagnostics can be performed to obtain its disease stage. If the tumor is deemed too large for removal, chemotherapy and/or radiation treatments may be recommended in an attempt to reduce the mass to an operable size. Inoperable tumors should be evaluated by incisional biopsy for histologic grade.
The decision to pursue additional treatment should consider the grade of the cancer as well as the results of other prognostic tests. Post-surgical radiation and chemotherapy are warranted on a case-by-case basis. The most important considerations when determining if a patient needs additional treatment following surgery are tumor grade, how complete the excisions of the tumor were, and whether the MCT has spread or not.
Mast Cell Tumor Grading
Traditionally MCTs have been classified using the Patnaik grading system, which assigns a histological grade of I, II, or III to each tumor. Studies have shown that the grade assigned to a particular tumor can vary as it is based on the subjective opinion of the pathologist; accordingly, sometimes a second evaluation of the biopsied tissue is warranted.
- Grade I. About 33 to 50 percent of MCTs are classified as Grade I; these tumors act in a benign manner and are usually considered cured with complete surgical excision and simple monitoring over time. They tend to be contained and not prone to metastasis or recurrence. One exception is low-grade tumors on the dog’s muzzle or lips; these have a high rate of spread and need to be treated more aggressively, as 50 to 65 percent of them will develop metastasis.
- Grade II. About 25 to 45 percent of MCTs are classified as Grade II – and this is where the decisions about their treatment get really challenging. Some Grade II tumors act like Grade I tumors, but others are similar to Grade III and more difficult to treat.In general, Grade II tumors are less defined than Grade I tumors and about half of them are more likely to spread into surrounding tissues and other parts of the body, with about 25 percent having already spread at the time of diagnosis. A Grade II tumor with a mitotic index (more on this below) of greater than 5 should be treated as a Grade III tumor.
- Grade III. About 20 to 40 percent of MCTs are classified as Grade III. These very aggressive tumors invade quickly and into deep tissue layers. About 50 to 90 percent grow and metastasize, with most cases showing spread by the time of diagnosis. If removed, 55 to 95 percent are likely to recur. Surgery along with chemotherapy and/or radiation is usually recommended.The Kiupel system of MCT grading is more recent and achieves better consensus among veterinary pathologists. This simpler approach categorizes the tumors as either high-grade or low-grade; the assessments this system uses provide for a more accurate prediction of the behavior of the disease and therefore hopefully to determine a more significant prognosis. High-grade tumors tend to be associated with increased likelihood to metastasis and poor prognosis with an average survival time of approximately four months. Low-grade tumors have a median survival time of more than two years.
Supplemental Testing
As there is no single factor or test that accurately predicts the behavior of the disease, supplemental testing can be invaluable in developing an accurate assessment and improving the prognosis of affected dogs.
- Mitotic Index. This test measures the rate at which the malignant mast cells are dividing and populating at the time of biopsy (this is one of the tests in the Kiupel system of grading) and is now usually included in biopsy reports. A tumor with a mitotic index of 5 or less can be treated as a Grade I MCT with a good prognosis and a median survival time of more than five years (regardless of histological grade). MCTs with a mitotic index over 5 should be treated as Grade III tumors. Median survival time for those with higher mitotic indexes is two to four months, again, regardless of the grade.In general, the higher the mitotic index, the poorer the prognosis. For those tricky Grade II tumors especially, this test provides insight into how the tumor is likely to behave, so an appropriate treatment plan can be developed.
- MCT Panel. The MCT prognostic (or proliferation panel of tests can derive additional information from the biopsy sample may help develop a prognosis and treatment plan, especially for high-grade/Grade II/Grade III tumors. This panel evaluates the specific markers AgNOR, PCNA, Ki-67, c-Kit, and tests for c-Kit mutation status, which are related to the proliferation of the MCT.
Approximately one-third of all dogs with MCTs have c-Kit mutation of the mast cells. This is an abnormality in the c-Kit gene, which affects a protein found on the cell’s surface and is involved with proliferation and other biological activities; the mutation causes the tyrosine kinase receptor enzyme in the gene to be stuck in the “on” position, causing uncontrolled growth. In particular, the c-Kit mutation test can indicate whether chemotherapy is warranted, as well as provide a guideline for which chemotherapy protocol to use.
While the presence of this mutation is usually found in higher-grade tumors and indicates a more aggressive form, it also may be more susceptible to treatment with a class of drugs known as KIT inhibitors. Palladia and Kinavet are two chemotherapy drugs that target this mutation specifically; they act by cutting of the blood supply to the tumor and inhibiting tyrosine kinase (a protein that plays a role in growth and development).
Other Treatments
MCTs are very susceptible to radiation therapy, a localized treatment. Radiation is especially helpful in preventing regrowth for incompletely excised tumors. The majority of dogs with low-grade MCT remain tumor-free two to five years after surgery and radiation therapy.
Even dogs with Grade III MCT can benefit from this dual mode treatment; one study documented 70 percent still alive one year following treatment; another study reported a median survival time of 20 months. It may also be used to treat tumors that are not candidates for surgical removal due to size and/or location, either to reduce the size prior to surgery or as palliative care by reducing the size of the tumor and improving clinical signs. It does not prevent metastasis.
Radiation as a primary treatment is considered a palliative approach; the addition of chemotherapy and steroids can improve this approach and may be offered for cases with no other treatment options.
Chemotherapy may be recommended as part of the treatment protocol in cases where the MCT has metastasized or has been rated as high-grade or Grade III, as well as those with a positive c-Kit mutation result, dirty margins, high scores on either the prognostic panel or mitotic index, or presenting with multiple tumors. Chemo may also be considered to prevent tumor recurrence, especially when radiation is not an option.
Combining chemo with surgery typically improves the prognosis of dogs with high grade tumors; median survival for dogs with Grade III tumors undergoing surgery alone is six months while those who undergo surgery and chemo have a median survival time of 12 months. Combination chemotherapy protocols, often in conjunction with steroids, also offer improved efficacy. Commonly used drugs include Lomustine (CCNU), Vinblastine, Palladia, and Kinavet. Vincristine, L-asparaginase, and cyclophosphamide have also been used with some effectiveness.
Supportive Treatment
In addition to antihistamines, supportive medications to consider include: prednisone to reduce inflammation; cimetidine, an antacid that helps to counter the increased acid production in the stomach caused by the MCTs; and intralesional triamcinolone, a corticosteroid, which can be injected directly into the tumor to reduce size. Cryotherapy is sometimes used to freeze and destroy small MCTs; this approach can be an option for older dogs for whom anesthesia and surgery are not an option.
Prognosis
Prognostic considerations for MCTs include grade, clinical stage, location, systemic symptoms, status of surgical margins, and mitotic index. Mast cell tumors that are completely removed and are Low-Grade, Grade I, or Grade II with a low mitotic index and free of metastasis have an excellent prognosis, with most cases being considered cured. Dogs with tumors that were incompletely removed but subsequently treated with radiation therapy have an excellent prognosis as well, with 90 to 95 percent having no recurrence of the tumor within three years.
Poor prognosis is associated with MCTs that occur on the muscle, around the mouth, in internal organs, in the bloodstream, or in bone marrow; those that are ulcerated, large, fast-growing, or recurring are also in this category. Dogs with c-Kit mutation are also associated with poor prognosis, as are dogs with Grade III tumors as local recurrence and/or spread is likely (only about 10 percent of these dogs live a year past surgery). Survival rates for dogs with a mitotic index of over 5 is only two to four months. As daunting as some of these figures are, remember that these are only guidelines; every dog is different.
On the Horizon
A number of exciting therapies for MCTs are in development:
- New treatments using receptor tyrosine kinases inhibitors for tumors with c-Kit mutations are an active part of cancer treatment research for both humans and dogs.
- QBiotics has completed clinical trials on Tigilanol Tiglate EBC-46, a novel anticancer pharmaceutical protein kinase C activator isolated from the seeds of the Blushwood tree (Fontainea picrosperma). The drug, administered by injection into the tumor, stimulates the immune system, resulting in destruction of the mass as well as the blood supply to the tumor. Complete tumor destruction was achieved in 75 percent of the cases after a single injection; the trial demonstrated that the treatment was well-tolerated (minor side effects) with rapid healing and minimal scarring. Application for approval is in process.
- A recent study at the Animal Health Trust Center for Small Animal Studies looked at the genetic changes in mast cells that promote metastasis. Researchers hope this will help develop a highly accurate test that can predict whether an MCT will metastasize; if successful, targets can be identified for new drugs to prevent metastasis. Future research will attempt to identify the causes of those genetic changes, resulting in the development of new cause-targeted anti-metastasis drugs.
- The Cummings School of Veterinary Medicine at Tufts University is conducting a clinical trial to evaluate an experimental drug in dogs with solid tumors (such as MCTs). The hope here is that the drug will not only stimulate the immune system to destroy the cancer cells but also kill the cancer cells directly.
- Oncolytic virotherapy is an emerging therapeutic option for cancer treatment. Studies have found that a modified Sendai virus (of the Paramyxoviridae family) can spread in tumors and kill malignant cells while sparing normal cells.A recent pilot study of six dogs with MCT received the oncolytic Sendai virus treatment. It was well-tolerated with minor transitory side effects. All tumors responded, either partially or completely, indicating a promising approach. Because this treatment does not overlap with any known mechanism of current conventional MCT treatments, researchers hope it will prove effective in combination with other protocols, and warrants additional research.
- Companion Animal Health recently initiated a partnership with Nanospectra Biosciences, Inc. to conduct clinical trials in the treatment of MCT using a combination of laser and nanoshell therapy. The approach of this treatment is to destroy the tumor without damaging adjacent healthy tissue. The initial results are encouraging, and trial outcomes should be published soon. It is hoped that it will deliver an improved treatment option and extend life without harmful side effects.
Watch Those Lumps
My Border Collie Duncan had 29 lipomas. Every time he developed a new lump, I had it aspirated and checked to make sure it was just a lipoma, not an MCT. I also tracked every one of his lumps on a diagram (see below) so I knew whether any given bump was new and potentially dangerous or just an existing lipoma.
Early detection for MCT is key and important for obtaining optimal treatment and long survival rates. If you find a growth on your dog that doesn’t go away after a month, please see your veterinarian to have it aspirated. Even dogs with high-grade metastasized MCTs can have a good quality of life.
Beyond the 5 Freedoms of Animal Welfare
The “Five Freedoms,” a set of standards for humane animal care, have long been internationally respected and embraced by animal protection organizations, including the American Society for the Prevention of Cruelty to Animals, Royal Society for the Prevention of Cruelty to Animals, Humane Society of the United States, and many more. The American Humane Association calls the Five Freedoms the gold standard of animal welfare.
The original guidelines were developed in response to a 1965 United Kingdom Government report on livestock husbandry. Each of the Freedoms was followed by a “Provision” that explained how the goal could be met. Initially focused on livestock, the application of these five principles of care has been generalized to include the keeping of companion animals, too.
The Five Freedoms and Correlating Five Provisions
These are the Five Freedoms and Five Provisions as currently accepted worldwide:
- Freedom from hunger or thirst, provided by ready access to fresh water and a diet to maintain full health and vigor.
- Freedom from discomfort, provided by an appropriate environment, including shelter and a comfortable resting area.
- Freedom from pain, injury, or disease, provided by prevention or rapid diagnosis and treatment.
- Freedom to express (most) normal behavior, provided by sufficient space, proper facilities, and company of the animal’s own kind.
- Freedom from fear and distress, provided by ensuring conditions and treatment that avoid mental suffering.
Many of our agricultural practices still fall short of these standards. Sadly, even many companion-animal-keeping practices fall short in puppy mills, and even in some homes, shelters, and rescues.
An Even More Progressive Model: The Five Domains
More recently, a more progressive approach to animal welfare has been proposed – one that parallels the move toward more dog-friendly dog training. David J. Mellor,Ph.D., Director of the Animal Welfare Science and Bioethics Centre and professor of Animal Welfare Science at Massey University in New Zealand, developed and promotes a set of guidelines he calls the Five Domains. His model emphasizes maximizing our animals’ positive experiences, not just minimizing negative ones. This approach moves beyond animal welfare (taking care of an animal’s basic needs) to the modern, far more progressive and humane concept of animal well-being (ensuring the animal’s quality of life).
In a 2016 paper published in Animals (an international, peer-reviewed, open-access journal devoted entirely to animals, including zoology and veterinary sciences), Dr. Mellor stated, “A marked increase in scientific understanding over the last two decades now shows that the Five Freedoms do not capture, either in the specifics or the generality of their expression, the breadth and depth of current knowledge of the biological processes that are germane to understanding animal welfare and to guiding its management.”
Dr. Mellor more fully described his model in a 2017 paper also published in Animals. “The Five Domains Model is a focusing device to facilitate systematic, structured, comprehensive and coherent assessment of animal welfare,” he wrote. “The purpose of each of the five domains is to draw attention to areas that are relevant to both animal welfare assessment and management.”
Dr. Mellor proposed that there are five domains of critical importance for modern, humane animal keeping.
In order to provide clear guidance on beneficial objectives for animal welfare management, Dr. Mellor described correlating provisions in each of these domains. Here we list his Five Domains, followed by questions we developed to help you assess how well you might be meeting – or falling short of meeting – these provisions when caring for your own dogs.
1: Good Nutrition
Provide ready access to fresh water and a diet to maintain full health and vigor. Minimize thirst and hunger, and enable eating to be a pleasurable experience.
Self-assessment: Do you feed a good quality food that is also pleasant to taste for your dog? Do you add extra tasty tidbits, vary his diet and control the presence of any aversives while he eats, perhaps even incorporate scent work with his meals to make sure he has a pleasurable dining experience? Have water accessible at all times (except perhaps when he is sleeping)? Avoid the use of water or food deprivation as a training tool?
2: Good Environment
Provide shade/shelter or suitable housing, good air quality, and comfortable resting areas. Minimize discomfort and exposure, and promote thermal, physical, and other comforts.
Self-assessment: Do you make sure your dog always has access to areas with appropriate/comfortable temperature levels – heat in the winter and air conditioning in the summer? Does he have options to choose for himself how warm or cool he wants to be? If walking with your dog in heat or cold, do you provide various means for him to stay cool or warm as needed, depending on the dog: warm jackets, boots to protect paws from hot pavement, dampening his coat to allow for cooling evaporation?
3: Good Health
Prevent or rapidly diagnose and treat disease and injury, and foster good muscle tone, posture, and cardiorespiratory function. Minimize breathlessness, nausea, pain, and other aversive experiences and promote the pleasures of robustness, vigor, strength, and well-coordinated physical activity.
Self-assessment: Is your dog up-to-date on all necessary prophylactic treatments? Do you seek veterinary care promptly at the first sign of illness or injury? Do you consistently mitigate temporary or long-term pain or discomfort with appropriate analgesics? Is your dog fit, well-exercised, and in good weight, not over-crated or overweight?
4: Appropriate behavior
Provide sufficient space, proper facilities, congenial company, and appropriately varied conditions. Minimize threats and unpleasant restrictions on behavior and promote engagement in rewarding activities.
Self-assessment: Do you allow and encourage your dog to behave like a dog? Does he have regular opportunities to bark, dig, run around, jump on things, play, get wet, get dirty, and otherwise act like a dog – with you, and/or other dogs or individuals of other species, if he enjoys their company?
5: Positive Mental Experiences
Provide safe, congenial, and species-specific opportunities to have pleasurable experiences. Promote various forms of comfort, pleasure, interest, confidence, and a sense of control.
Self-assessment: Do you take him places he likes to go and encourage activities that engage his mind, challenge his creativity, give him choices, spark his curiosity, encourage him to think and problem-solve, build his confidence, and otherwise enhance his enjoyment of life?
Score Your Own Dog-Keeping
We would expect that Whole Dog Journal readers in general are doing a good job of providing for their animal companions’ welfare. Even so, we can all do some self-examination to ensure that we are doing as much as we possibly can to also ensure our animal companions’ well-being.
Take another look at the Five Domains and Provisions, and then do a critical self-examination of all the things you provide to enhance your own dog’s well-being. If you can honestly check off all five of the boxes, our hats are off to you: You are a dog-companion superstar and the champion of your dog’s well-being.
If, on the other hand, you identify some areas that need work, then get started on any needed changes – and kudos to you for your willingness to commit to providing your dog with the best life possible.
An Ill-Advised Weight-Loss Program: Bowser’s Story

Bowser was a sweet, lovable, and very fat Beagle. Instead of weighing a healthy 30 pounds, he was a whopping 50. Bowser’s veterinarian examined him in June and prescribed weight loss. It was recommended to his owner that Bowser’s food be changed to a metabolic diet, he stop receiving hourly treats, and he start exercising.
His well-meaning owner felt terrible. He hadn’t realized that Bowser was so overweight. Determined to help his canine friend get in shape, he took Bowser on a run. Unfortunately, Bowser, unlike his owner, was not a runner. He was terribly out of shape. He kept up gamely for the first mile, but somewhere in the second, he collapsed. It was, after all, June in the southern U.S.
Bowser came to our ER on a stretcher. He was panting uncontrollably, stretched out on his side. He had been vomiting, and he had severely bloody diarrhea. His belly was covered with bright red spots. The thermometer read 111 degrees.
Our emergency team jumped into action immediately. An IV catheter was placed and cooled fluids were started. A fan was pointed at Bowser, and towel-wrapped ice packs were placed along his belly and in his armpits. An oxygen mask filled with ice chips was placed over his nose.
Bloodwork showed that Bowser was already severely affected. His white blood cell count and blood sugar were low, and his blood wasn’t clotting properly. His liver and kidney values had already shot up as a result of the shock and organ damage, making his prognosis guarded. His owner was devastated. He had never intended to cause his dog any harm, and he told us to do whatever we needed to do to save his friend.
Bowser spent four days in the hospital with intensive care. He was given two plasma transfusions, many liters of fluids, and kept on antibiotics. Despite how severely he was affected, Bowser recovered. After four days, he went home with his loving and grateful owner to begin his weight loss journey at a much slower pace!
Avoiding Heat Stroke in Dogs

Summer is a great time to be a dog owner. Long warm days mean plenty of outdoor activities like swimming, hiking, and playing. It’s important to remember however, that just like us, our canine friends can overheat. As a result, taking precautions in the spring and summer is critical. With attention to your dog’s behavior in the heat and preparation for the season, you can avoid a heat stroke.
What Causes Heat Stroke?
The canine body operates best in a very narrow temperature range – usually from 99 to 102 degrees. Above 109, and body systems will become severely damaged.
The dog’s temperature is tightly controlled by the hypothalamus, an area in the brain. Elevations in temperature can be caused either by endogenous factors (inside the body) or exogenous (outside).
Fever occurs when the hypothalamus resets the normal body temperature higher as a result of infection or inflammation. It is initially a beneficial response, as it enhances the ability of the immune system to destroy viruses and bacteria. With fever, trying to cool a dog down will not help, as the brain is controlling the body temperature. It will only lead to shivering as the body tries to rewarm to the new set point. This is uncomfortable and expends energy. Cooling is not recommended for fevers.
Heat stroke (hyperthermia) is caused by external factors such as a hot environment or overexertion in the heat. The brain set temperature is normal, but a dog is unable to cool effectively, and so body temperature rises.
Dogs cool by two mechanisms: evaporation and conduction. Evaporation of heat occurs with heavy panting. Conduction occurs when a hot dog lies on a cool surface and heat is transferred. Dogs sweat very minimally and only through their footpads, so this is not a significant means of cooling.
Heat stroke progresses through three stages. It begins with heat stress. Initially, a dog will pant heavily, seek a cool surface, and drink water to bring body temperature down.
If a dog cannot do these things or cannot do them effectively (such as when trapped in a hot car), heat stress develops into heat exhaustion. The panting becomes much faster, heart rate elevates, the gums become red and tacky, and body temperature is likely greater than 106 degrees.
If this goes unaddressed, heat stroke develops. Body temperature exceeds 109 degrees. A dog will vomit, have profuse diarrhea, begin to seizure, and collapse.
Most Susceptible Dogs
All dogs can have heat strokes, but some are more prone to developing problems. Brachycephalic breeds like Bulldogs, Boston Terriers, and Boxers are notorious for overheating. Due to breed-related airway abnormalities such as small nostrils, long floppy palates and tonsils, and narrow, weak windpipes, brachycephalic dogs can overheat very quickly.
However, Labradors and other breeds vulnerable to laryngeal paralysis, another obstructive upper airway disease, are also at significantly increased risk. Dogs with cardiac disease can be predisposed, as well.
Another consideration is whether a dog is conditioned enough to be in the heat. Dogs who are not accustomed to exercise and exert themselves in hot weather can suffer heat stroke very rapidly. This is especially true if they are overweight or elderly.
Most commonly, any dog left in an unventilated car in temperatures above 65 degrees can suffer from heat stroke. This is most often seen in the spring and summer.
Symptoms
Heat stroke is not immediate. Symptoms begin with heavy panting and restlessness. This progresses to weakness and collapse, followed by profuse vomiting and diarrhea (often bloody). As heat stroke continues, a dog will become extremely dull to non-responsive. Seizures can develop in the late stages. Red to purple spots and patches may become visible on the skin.
Once the heat stroke goes untreated, every body system becomes involved. Shock develops. This means decreased oxygen delivery to tissue, which eventually leads to multiple organ dysfunction syndrome (MODS).
In the kidneys, the renal tubules (responsible for conserving water and electrolytes) are damaged. Water, glucose, and electrolytes are lost instead of conserved. Potassium, instead of being excreted, is retained. High levels of potassium causes cardiac arrhythmias.
The ability to clot blood is also severely affected. Coagulation proteins are made in the liver, and they function within the body’s normal temperature range. At above 109 degrees, they are damaged, and clotting becomes difficult. This leads to visible bruising on the skin called petechiae. When these coalesce into large patches, they are called ecchymoses. It is especially visible on the belly, where there is less hair, on the gums, the white of the eye (sclera), and inside the ear pinna.
Liver damage also occurs due to shock. The liver is essential for many functions. Two of the most important are production and storage of glucose, the body’s energy source, and the manufacture of clotting factors. Most dogs suffering heat stroke will have low blood glucose levels due to liver damage. Brain tissue is likewise affected leading to swelling of neurons. This can cause stupor, seizures, coma, and death.
The cells lining the gastrointestinal tract start to die as a result of the hyperthermia. Once those cells are damaged, the protective lining of the intestines weakens and thins, leading to bacteria moving freely into the bloodstream (bacterial translocation). This causes “blood poisoning” or sepsis.
Every system of the body feels the effects of heat stroke, making prompt care imperative to recovery.
Treatment
Treatment of true heat stroke must be rapid and aggressive. Immediately cool your dog if you suspect heat exhaustion. If you have a hose or bathtub, wet your dog down with cold water thoroughly, especially the paw pads and thinly haired areas like the stomach (this will help dissipate heat quicker). If you are outdoors and near a body of water, a quick dip can help bring down temperature.
After cooling, take your dog to the veterinarian. Do not wait to see if he improves, as heat stroke can be deadly in a matter of hours.
Heat stroke causes shock, and this must be treated quickly. Initial vitals will be taken while the veterinary team works to stabilize your dog. If you have already cooled your dog at home, the temperature may be lower than expected, but this does not mean your dog has not had a heat stroke.
An intravenous (IV) catheter will be placed, and cool fluids will be given rapidly. This will increase blood flow to all parts of the body and improve oxygen delivery. Fans and cold water will be applied to bring body temperature down. Oxygen should be supplied either via face mask or nasal prongs. Ice chips in the oxygen mask can cool and moisten the air to further increase cooling.
Additional treatments should include broad spectrum antibiotics to protect against bacterial translocation and sepsis, IV dextrose to maintain normal blood sugar levels, mannitol or hypertonic saline to decrease cerebral edema (swelling in the brain), and continued oxygen and IV fluids. Fresh frozen plasma may be given in cases where clotting abnormalities have already developed. The plasma can provide clotting factors when the liver cannot manufacture its own or when they are deactivated by hyperthermia.
Prognosis
The prognosis is always guarded, as uncontrolled hyperthermia leads to multiple organ damage. Immediate, intensive care will improve the prognosis. Hospitalization can be prolonged, often at least 48 to 72 hours. During that time, frequent vitals and bloodwork should be conducted, including tests of clotting times and blood glucose.
Avoiding Heat Stroke
When the weather warms up, it is important to slowly acclimate your canine companion to the weather. Heat and humidity both play a role in overheating, and even on moderately warm days, if the humidity is high, overheating can occur. Plan exercise and activities for the cooler parts of the day – around sunset and early in the morning. If the temperature is moderately hot, your dog can spend short periods of time outdoors to acclimate. Do not exercise an unconditioned dog in the heat.
Any dog with upper airway abnormalities or cardiac disease should have minimal outdoor time in the summer. At the first sign of any overheating, they should be calmed and aggressively cooled with a hose or bath. This includes brachycephalic breeds and dogs with laryngeal paralysis and heart disease.
Make sure when your dog is outside that he has shade and plentiful fresh water. Keeping it cold and fresh may encourage your dog to drink more. Replenish frequently and add ice cubes. A kiddie pool filled with cold water is also excellent for the water-loving canines. If you plan to visit a dog park, choose one that has water nearby for swimming and playing.
There are an array of cooling devices that can be found for purchase including vests, sleeping pads, dog houses, and collars. (The best of these were recommended in “How to Prevent Heat Stroke in Dogs,” in the July 2015 issue.)
The best tip to remember is, if you’re in doubt, err on the side of caution and avoid overdoing it!
Doing Time in the Waiting Room
It’s June, and northern California, so we’re here (probably) for a foxtail. My tenant left the side gate to my office/house open, and Odin was out in the (unfenced!) front yard for anywhere from 10 minutes to an hour – grr! I looked up from my computer when I heard the sound of vomiting and glanced around me to find the source of the sound. I simultaneously noticed that Odin was not lying on the office couch with Woody as per usual and that the vomiting sound was coming from the front yard. I stood and looked out the window, and there was Odin, puking on the front lawn.
I went out and called him, and he looked up at me miserably, giving a weak tail wag. “I don’t feel so good!” I brought him in the house and got a fork, with which to poke through the vomit, to try to determine what he ate that was making him throw up. It looked like it was entirely comprised of his breakfast kibble and a lot of grass – fortunately, no sign of rotten things or chicken bones or rat poison. But then, over the next couple of hours, he kept having strange hiccuping sessions, with moments of gagging. It could be that his esophagus is just irritated. Or it could be he has a foxtail stuck in there somehere. Only one way to find out.
You can’t wait with foxtails. The longer the grass awns have been in a dog, whether between his toes or up his nose or down his ear, the more damage they cause. If you can get them out on the first day, the bill will be less. So here we are.
Also here: An old Labrador, lumpy with (presumably, I hope) lipomas. He’s shaking with anxiety and balking a bit, and his owner gives the leash a rough yank. Oh, c’mon. Why do people do that at a time like this?
I watched a lovely black and white Standard Poodle, immaculately groomed. She’s pulling for the front door, and her owner stops for a moment and says something to her in a quiet voice. She immediately stops pulling, circles back to his side, and they resume their walk to the front door at a sedate pace. That’s better.
A lady sits near us, waiting to pick up her dog. Odin strains to reach her, wagging his tail. She smiles and asks if she can pet him. “He’ll jump in your lap!” I warn her, laughing. “He will kiss you on the lips!” He does just that as she giggles and wraps her arms around him in a warm embrace, and he buries his head in her chest. “I have had my rescue dog for six years, and she’s never let me do that!” she exclaims. Wow. I can’t even imagine.
We had a three-hour wait for a room. After observing Odin’s hiccups and hard swallowing, the vet sedated Odin to examine his throat. Four hours and a nap in my car later I picked up a still dopey pup; the vet hadn’t found anything besides irritated tonsils, but at least we know. Life with dogs!
When It Comes to Dog Training, Practice Makes Perfect
Anyone who has ever learned to do something physical – hitting a baseball, sewing a garment, driving a car, you name it – understands that you gain competence only through practice and repetition. At first, your movements and timing are clumsy and imperfect. You probably overcorrect, making crooked or zig-zagging seams or driving the car over the centerline bumps. But over time – and especially if you have some expert guidance – your movements become smooth and coordinated, and it seems to any observers that you’re a natural! Ha! If only they could see you at the beginning!
Learning new skills is hard work – for people AND dogs
Now, think about learning something new with a partner who is also learning the same skill, such as a new dance or perhaps sign language. The difficulty factor goes way up! It’s going to take a bit longer for the result to look smooth.

Now imagine that your dance partner or sign language conversation partner speaks a different language! If this is the case, all of your clumsy efforts require that much MORE patience, creativity, and humor with each other as you try to figure out how to communicate while simultaneously managing intricate dance steps or movements of the hands.
This latter scenario, you may have already guessed, is exactly what’s at play with new dog owners and their new dogs or puppies!
Every new owner wants their puppies or dogs to behave well – to stop doing uncomfortable or naughty things like chewing shoes, jumping on people, or barking at the leaves falling in the back yard, and to perform good behaviors on cue, such as sit, down, wait, and leave it. It adds quite a layer of difficulty to teach them to do what we want, in a language that is not their own, while we are simultaneously learning to use our posture and movements (body language!) for cues and the timely delivery of reinforcers!
Using markers and reinforcers
In the late 1940s, pioneering animal trainers Keller and Marian Breland started teaching other animal trainers to use a marker and the immediate delivery of a reinforcer to teach animals to perform behaviors. They found that chickens were a great species to use to help trainers learn the physicality of cues and reinforcement delivery – especially, the timing of the marker and reinforcer delivery, as well as the location and presention of the both the cue and the reinforcer.
Chickens who were raised around people aren’t afraid of humans, they notice very minute differences in the appearance of things, they are very quick to react when they notice these differences, and they are very motivated by food to try new behaviors. They also don’t carry a lot of behavioral “baggage” along with them, resulting from living with sometimes-intemperate humans! They make amazing practice partners for anyone who is learning how to observe animal behavior and learn to change it swiftly and without force, and there is a long legacy of trainers who still use chickens to teach dog trainers how to refine and improve their training technique.
Don’t blame the chicken!
Another brilliant thing about using chickens to teach people how to train: people don’t get mad at chickens when they are failing to get the chicken to perform a specific behavior! They don’t tend to start calling the chicken “stubborn” or “spiteful” – or blame the chicken’s breed, origins as a “rescue chicken” or anything else. They are able to easily see that training the chicken is just a matter of presenting the training challenge to the chicken in a precise way that makes it easy for the chicken to do the behavior (or some approximation of it), for the behavior to instantly be “marked” (with the click of a clicker or a verbal marker, such as the word “Yes!”, or the flash of a penlight, or what have you!) and be reinforced for it immediately.
They are also able to see that if they are late with the marker, or fail to deliver the reinforcer in a timely fashion and in a location that doesn’t pull the chicken out of the position the trainer wanted her in, that it’s impossible for the chicken to “get” the point of the exercise! They see that it’s their own clumsiness or bad timing, not the chicken being “bad.”
Get a second set of eyes

If you are having trouble teaching your dog some new behavior, consider taking a little video of yourself as you work with your dog, or ask someone who you consider to be a good trainer to watch you. It might develop that you simply need a little coaching on how you are presenting the cue, or marking the desired behavior, or delivering the reinforcer. Strike that: It is undoubtedly a problem with one of those things, not that your dog is being dumb, lazy, or a non-native speaker of English.
Honestly, if you are motivated to learn how to more effectively teach your dog new behaviors quickly, sign up for a class or even just a private lesson or two with someone who is experienced with positive reinforcement-based training (and who does NOT use punitive, physical “corrections” AT ALL). With a few pointers, you will be amazed at how quickly you and your dog or puppy will be happily speaking the same language as you dance through life together.
Dog Kisses: Is Your Dog Really Kissing You?
You either love it or hate it: the wet, warm sensation of a dog licking your face. Many of us seek out this kind of interaction with our dogs (sometimes much to the horror of onlookers) while others try to discourage the behavior. Many dog lovers attribute a lot of meaning to dogs licking us, especially if we’re the sort that enjoy it – we say our dogs are giving us kisses and we interpret that as a sign of affection, but are dog kisses really a sign of affection? Or are they just after the leftovers we forgot to wipe off our chins?

Why do Dogs Lick People?
Certified Professional Dog Trainer and Chair of The Association of Professional Dog Trainers Nick Hof, CPDT-KA, CBCC-KA, KPA-CTP, CSAT, explains there are a lot of reasons why dogs lick people’s hands, feet or faces. It might mean your dog wants to show you affection, but it could also be because you taste good or that your dog is struggling with compulsive behavior.

If you are wearing sweet-scented lotion, or come home sweaty, your dog might be licking you because you taste good. I know my own dogs are very excited to lick my hands if I’ve been eating something greasy or salty, like potato chips. Hof mentions that dog guardians shouldn’t be alarmed by their dogs finding them delicious – they probably won’t take a bite out of you!
While most of the time dog kisses aren’t anything to be concerned about, Hof warns there are times when the kissing might be a sign of something else going on with your dog. He advises that there might be an underlying health issue “if the licking seems to be compulsive, excessive, or self-destructive; if it is difficult to redirect your dog or they are harming themselves, you should consult with your veterinarian for help addressing this issue.”

Are Dog Kisses Actually Signs of Affection?
Unfortunately, there’s no easy answer to dogs’ intentions when licking their people, but it seems to come down to whether your dog is seeking you out, or if you are seeking your dog out.
Hof explains, “It’s helpful to look at the context of the licking to better understand and pay attention to other signals besides the licking or the kiss, such as the dog approaching the owner and choosing to engage in the behavior despite having the option to move away or leave; or was the dog thrust upon and looking away and licking his lips as well?” In other words, forced affection on the part of the guardian can warp the true intention of a dog’s kiss – a dog will “kiss” your face to appease you and make go away rather than to display their love for you.

Hof offers the following important reminder: “it’s always best to invite your dog to approach you so that you feel more confident they’ve made that choice willingly. When you begin to respect your dog’s autonomy, you see more comfort and confidence in their behavior.” What you can count on as a result is knowing the way your dog behaves with you is genuine.
For safety reasons (and this is a hard one for many of us who share our lives with dogs), Hof states that it is not recommended for people to put their faces up to their dogs’ faces. Although this is often done as a sign of affection from us, it is very commonly invasive to our dogs and they may not appreciate it. This is where we most often see dogs licking or “kissing” their person’s face as a way for the dog to avoid conflict.
This “Kiss to Dismiss”, as coined by the Family Paws Organization, is often paired with a look away from the person and licking of lips. If you would like to have a close moment with your dog, invite them to do so with you, and if they want to come up to your face, they will – but if not, respect it when they say ‘no’. Obviously we want our dogs to be comfortable so it’s important to be thoughtful of how we physically show emotions to our dogs, so that our dogs don’t feel pressured to appease us through kisses.
How to Get Your Dog to Stop Licking You
If your dog is prone to kisses and you or your family and guests aren’t fans of it, Hof explains the best thing you can do is to be proactive with training your dog.
“If you see them approaching and you know they’re going to lick you, ask them to sit as they approach, then redirect their affection and energy onto a toy or other activity. If, when you sit down to watch TV, your dog tries to give you a tongue bath, give them a stuffed Kong or a bone to enjoy instead of your sweat or lotion.”
Getting ahead of the behavior is particularly important. “If you wait until they are already licking you to always redirect, you may inadvertently reinforce the licking behavior with a treat or chew,” Hof cautioned. Simply this means your dog may increase his licking in order to get the treats you were using to redirect the licking in the first place.
If you have a hard time redirecting your dog or discouraging licking behavior, it’s a good idea to talk with your veterinarian or a veterinary behaviorist to determine if there is something going on with your dog causing what might be obsessive licking behavior. Dog trainer Jill Breitner reminds us that, “Licking as in lip licking or tongue flicks are a sign of stress.” She also points out that it can happen quickly and that dog guardians may not even realize that their dog is stressed.
“Context is always key in decoding the emotional state of a dog,” explains Breitner, creator of the Dog Decoder App in collaboration with artist Lili Chin of Doggie Drawings. This interactive education app teaches users about canine body language and how to better read what your dog is telling you about their emotional wellbeing through body language. The app is available for iPhones and Androids.
Sassafras Lowrey is an award-winning author and Certified Trick Dog Instructor. Sassafras lives and writes in Portland, Oregon, with her partner, a senior Chihuahua mix, rescued Cattle Dog mix, young Newfoundland, two bossy cats, and a formerly semi-feral kitten.