Download the Full September 2003 Issue
Dogs are Body Language Communicators
NONVERBAL COMMUNICATION OVERVIEW
What you can do…
– Pay attention to your dog’s responses to your movements. Our dogs watch us much more carefully than most of us realize.
– Be consistent with your physical cues. The more consistently you use them, the faster your dog will understand what they mean.
– With a new or young dog, avoid using body language that dogs find threatening, such as hugging or looming over the dog, staring him straight in the eyes, or grabbing his collar at the scruff of his neck.
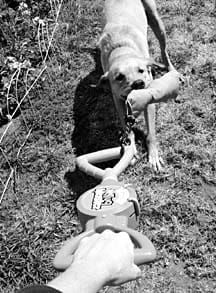
Week Three of our training class. We are working on “verbal downs” – getting the dogs to lie down on just a verbal cue. Diane and her exceptionally sweet and compliant eight-month-old Great Dane, Gable, aren’t succeeding. I ask her if I can try.
“Sure!” she says cheerfully. A lazy wag of Gable’s long tail signals his willingness as Diane passes me his leash. I wait for Gable to offer a sit, which he does as promptly as his gangly, adolescent body allows.

Arms relaxed by my sides, I say “Down!” in a clear and happy voice. He stares adoringly into my eyes and remains sitting. I wait three seconds, then lure him down with the treat hidden in my right hand. He follows the lure to the floor, I click the clicker in my left hand, and pop the treat in his mouth. We repeat this a couple of more times, with a click! and treat each time.
I ask for the down again, and give an almost imperceptible nod of my head. He drops halfway to the floor and glances up at me, eyes bright. I give him an enthusiastic “Good boy!” and quickly lure him the rest of the way down, then click and treat. On the fifth trial, I give the verbal down cue without moving. He stares into my eyes for a heartbeat, then sinks all the way to the floor. Click! and jackpot (a cascade of treats).
Canine Body Language
Dogs are, first and foremost, body language communicators. While they do have a limited ability to communicate vocally, they are much more articulate with their subtle body movements, and much more intuitively able to understand ours. As Patricia McConnell says in the introduction of her excellent book, The Other End of the Leash, “All dogs are brilliant at perceiving the slightest movement that we make, and they assume that each tiny movement has meaning.”
Watching my students in class, I can see that the ones who tend to be most successful are those who are most consistent with their body movements. Consistency allows the dog to attach a consistent meaning (and response) to the movement. The more inconsistent the movement, the harder it is for the dog to connect the human’s random motions to a specific behavioral response. Gable was able to do a verbal “Down” for me in just five repetitions because:
1. Diane had done three weeks of work with him luring the down (and some work on the verbal cue “Down”), so he was very familiar with the cue and the behavior. I just had to fade the lure.
2. On the first three attempts, I separated the verbal cue from the motion of the lure, so he had the opportunity to process the word separately from the lure.
3. On the fourth repetition I gave the verbal cue, along with a body language cue to help him translate, then gave him a few seconds to process it. His half-down was a question – “Is this right?” My “Good boy!”, lure, click!, and treat constituted a big combined “YES!” answer to his question. Dog owners often miss their dogs’ questions, or fail to answer them.
4. By the fifth iteration, it was clear to Gable that the verbal “Down!” meant the same thing as the lure. The tiny movement of my head served to bridge the gap between the verbal cue and the behavior for him. We had successfully translated the body language into spoken English.
It is because of a dog’s use of body movement as a first language that we can train so successfully using lure-and-reward methods, and easily teach hand signals. However, the importance of understanding and responding appropriately to our dogs’ body language goes far beyond formal training. Body talk can make everyday life with your dog easier, enhance your relationship, and overcome some of the canine behaviors that are giving you grief.
Cross-Species Communication
One of the reasons humans and canines co-exist so beautifully is that we are both social species – we live in groups and create social rankings within those groups. Both species intuitively understand the concept of a “group leader” (Alpha Dog = Head of Household, Employer, President of the US); both species have members in their various groups who lead more naturally than others; and in both groups, ranking (or status) is fluid: You might be the head of your household, but subordinate to your boss at work, or to a colonel in the Army, or the Queen of England. Your dog might be the leader of your dog pack, but have very low status among the regular canine visitors at your local dog park.
However, canine and primate body talk have very different vocabularies, which can cause serious conflict between our species. For example:
– Humans meet face-to-face and hug. Dogs tend to meet obliquely, and a dog who puts his chin or paws over another’s shoulders in greeting is probably making an assertive statement about his rank – which may well elicit an aggressive response. This is why dogs have a tendency to bite when kids (or adults) hug them.
It is considered polite by humans in the Western world to make direct eye contact. Failure to do so is considered evidence of lack of character – disrespectful, shifty, or outright untruthfulness. (This is not true in some other human cultures, where direct eye contact is considered rude.)
– In the canine dictionary, direct eye contact is an assertion or a threat. The dog on the receiving end either looks away, a sign of submission – in order to avoid a fight – or takes offense and engages in agonistic (aggressive) behavior in response. The other dog backs off, or a fight occurs. This is one reason why so many children are bitten. They tend to stare at dogs anyway, and the more strangely (aggressively) the dog behaves, the more a child stares. Adults who insist on direct eye contact with strange dogs also tend to get bitten.
– We naturally face another person that we are speaking to, and our force-based culture encourages us to get more strident if a subordinate fails to comply with our requests. We were once taught to call our dogs by standing squarely facing them, arms at our sides, and saying “Come!” in a commanding tone of voice. Our voices got louder, more insistent, perhaps even angry, if our dogs failed to come.
Dogs see a full-frontal communication as a threat, and loud, firm, angry vocalizations as aggressive. Their natural response is to turn away in appeasement, or at best, to approach slowly, in a submissive curve, rather than the speedy, enthusiastic straight line that we strive for.
– We often reach for our dogs’ collars over the top of their heads. They see this as a direct threat; they duck away in submission (or they bite), and learn to avoid us when we are trying to catch them. We follow or chase them, intimidating them further or, alternatively, teaching them that if they take the lead, we follow. The more we try to catch them, the more they avoid us.
– We bend over them to pet them on the top of their heads, or to cuddle them. Again, we are unwittingly offering a posture of threat and intimidation. Primate “hovering” is a very off-putting posture for dogs. Dogs back away in fear or submission, or worse, bite in an aggressive response.
Prompted by ill-advised old-fashioned thinking, some people still use force (such as alpha rolls and scruff shakes) to overpower and dominate their dogs. Most dog body language is very subtle and in large part ritualistic, including the “belly-up” position, which is usually offered voluntarily by the subordinate pack member, not forced by the higher ranking one. Dogs experience the alpha roll as a violent, terrifying attack, and some will respond out of a likely belief that they are fighting for their very lives.
Doggy Adaptability
If you think about it, it’s surprising that we get along with our dogs as well as we do! The good news is that both of our species are pretty darned adaptable. We can teach our dogs to appreciate some of our bizarre primate behaviors, and we can learn to use canine body talk to our advantage.
We humans pretty much insist on hugging our dogs. Touch is so important to us that as much as we may intellectually understand our dogs’ resistance to such close body contact, our hearts overpower our heads and we just have to hug them.
When a dog reacts badly to being hugged, it’s often an innate response, not a conscious decision. The dog doesn’t sit next to the hugger, ponder his options, and make a deliberate decision to bite. Rather, the hug triggers a subconscious response: “Threat! Fight or flee! If the dog can’t flee – because he is being hugged – or is one of those dogs whose fight response is stronger than his flight response, he bites.
It’s easiest to teach a dog to accept hugging if you start associating gentle restraint with something yummy when he is very young. Using counter-conditioning and desensitization to change his natural association with close contact from bad (Danger! Run away!) to good (Oh yay! Cheese!), you can convince the part of his brain that reacts subconsciously, that being hugged is a very good thing.
To do this, hold the dog at a level of restraint with which he is very comfortable – perhaps just a light touch of your hand on his back. Feed him a tiny tidbit of something wonderful, and remove your hand. Repeat this step until he turns his head eagerly toward you in anticipation of his tidbit when he feels your hand touch his back.
Now, very slightly increase the intensity of your touch, by holding your hand on his back longer and feeding him several treats in a row; by pressing a tiny bit harder on his back; or by moving your arm a little farther over his back, so your hand brushes his ribs on the other side. The more your dog accepts touch, the more quickly you will be able to move through the counter-conditioning and desensitization process.
Note: Increase the intensity of only one stimulus at a time. For example, work on length of time until he is perfectly comfortable with long “hand-rests,” then shorten the time while you work on increased pressure. When he is comfortable with each new stimulus, add them together. When he can handle more pressure happily, start using more pressure for longer periods. Then ease up on both of these while you work on moving more of your arm over his back.
Of course, it is vitally important to teach children (and uninitiated adults) not to hug dogs unless they know the dog very well and are totally confident that the dog is fully comfortable with such intimate contact. Even then, young children should never be left unattended with any dog.
The same approach used to teach your dog to appreciate a hug works with many “culture clash” behaviors. If you want your dog to love having his collar grabbed, pair the action with cheese, or hot dog, or chicken. This particular exercise should be taught to every dog. Perhaps you know that the safest way to take hold of a dog’s collar is gently, under the chin. But if a friend tries to grab the collar over your dog’s head, it would be nice if she doesn’t get bitten for her primate behavior, because your dog has learned to accept it.
You can also teach your dog that eye contact is a good thing, by encouraging him to look into your eyes, and rewarding him when he does. (The clicker is very useful here.) Have your dog practice this with other people as well, if you want him to be comfortable with that pervasive and offensive primate penchant for staring rudely into canine eyes. And, again, teach your children not to stare into a dog’s eyes.
Human-Dog Communication is a Two-Way Street
While you are teaching your dog to understand and accept primate language, you can also learn and use canine body language. This will greatly enhance your relationship and your training program, since your dog can respond very quickly when he realizes you are speaking Dog.
McConnell describes a process that she calls “body blocking,” which simply means taking up the space to prevent your dog from doing so. Let’s say your dog is on a Sit/Stay while you are cooking in the kitchen, and you drop a fried drumstick on the floor. Tess starts to get up to get it. Rather than grabbing at her or yelling “STAY!” simply step forward into the space she was about to occupy. Like magic, she settles back into her Sit/Stay. McConnell reminds us that the sooner you react the better, and says that once you get good at it, you can simply lean forward an inch or two to express your intent to occupy the space.
You can also use body blocking with dogs who jump on you. Next time you are sitting in a chair and your wild Westie makes a running charge for your lap, clasp your hands against your stomach and lean slightly forward, blocking the space with your shoulder or elbow. It also helps to look away, rather than make eye contact. You may have to do several repetitions of this, especially if your dog has had much practice lap leaping, but it can be very effective if you are consistent. He can learn to wait for permission to jump up – on your lap, or on the sofa next to you.
I used body blocking for years without thinking about it or defining it as clearly as McConnell does. When our four dogs are all doing “Wait” at the door, I can release them one by one, by name, in part because I use subtle body blocking movements to indicate which dogs are to remain in place. As with the “Stay” blocking, the more you do it, the more subtle the movements can become, because dogs are so good at reading tiny body language signals.
This is just one example of the many ways you can make the canine/primate difference work for you as you build a relationship with your dog based on mutual trust and respect, and as you encounter other dogs. Move (run!) away from your dog when you want her to come, rather than moving toward her. She will follow the leader, instead of moving away from an intimidating direct approach. Look away from the challenging stare of an aggressive dog, instead of returning the eye-contact challenge, and you are more likely to escape from the experience bite-free.
We, as the supposedly more intelligent species, should be able to understand and forgive canine behaviors that clash with our human social expectations. It seems that our dogs are pretty darned good at understanding and forgiving ours, thank goodness. As you and your dog journey together through life, each translating primate to canine and vice versa, appreciate the great value of this cultural diversity.
Pat Miller, WDJ’s Training Editor, is also a freelance author and Certified Pet Dog Trainer in Chattanooga, Tennessee. She is the president of the Board of Directors of the Association of Pet Dog Trainers, and published her first book, The Power of Positive Dog Training, in 2001.
Veterinary Housecalls – Make the Most of Them
By Shannon Wilkinson
Picture this: A friend comes over for a visit. She settles herself on your living room floor and plays with your dog. She talks to him and to you, offering him a few of his favorite treats. After 30-60 minutes of enjoying one another’s company, she leaves.
Your dog might not have realized it, but he just had a veterinary exam. And neither he, nor you, had to leave the comfort of your own home.
This is the kind of appointment you can expect when choosing one of the growing number of mobile, or housecall veterinarians. The American Association of Housecall Veterinarians says that membership in their organization has increased 150 percent over the last 10 years. It’s not hard to understand why.
“An animal is much more at home in his own environment. My clients are pleased with the whole situation,” says Rose DiLeva, DVM. Her practice, Animal Wellness Center in Chadds Ford, Pennsylvania, currently consists of about 30 percent housecalls. The animals she sees at a client’s home aren’t stressed out, there are no worries about the possibility of carsickness, plus she has the opportunity to see the animal’s day-to-day environment.
Comfort, convenience, and personalized service
It’s not uncommon for animals to show signs of stress or trauma at the veterinarian’s office. These kinds of reactions at a veterinary hospital can become a conditioned response. It doesn’t take many unpleasant experiences – sometimes just one – for a dog to generalize that the veterinary clinic, or a person in a white lab coat, is going to do something to him that he doesn’t like or causes pain.
In fact, it is not even necessary for a dog to have personally experienced a bad visit to the vet. As the American Association of Housecall Veterinarians explains on its Web site, some animals release pheromones related to fear and trauma. The vet clinic waiting room and the exam rooms are a veritable potpourri of these scents. When other animals detect the pheromones, a fear response may be triggered.
Of course, most veterinary clinics are populated with sick dogs, and, despite even the most assiduous cleaning and disinfecting routines, the hospitals expose dogs to an increased risk of contagious disease. Housecalls, then, offer a particularly desirable option for those who wish to limit their dog’s exposure to infectious agents, such as guardians who practice natural rearing methods and either don’t use vaccinations at all or limit their use significantly (particularly for well-puppy exams), or people whose dogs have a compromised immune system.
Anna Maria Gardner (née Anna Maria Scholey), DVM, of PetSynergy in Spokane, Washington, says that some of her clients choose housecalls because of mobility issues – either their own, or their dogs. She has elderly clients who don’t drive, or because of arthritis, have a difficult time handling their dogs on a trip to a clinic. Some of the dogs suffer from arthritis themselves, or may be too large to ride in the car comfortably. She even provides housecalls to a religious cloister whose members never leave the convent.
Convenience is another common motivator for housecall clients. They might have multiple animals or small children at home. When the vet comes to them, they do not have to load everyone in the car, arrange for childcare, or make separate appointments for each of their animals.
Considerations
There may be limitations to the services your housecall vet can provide. Some veterinarians have “clinics-on-wheels” and can provide every level of care and even perform surgery. Other vets who provide housecalls may limit their practice to different types of hands-on exams and complementary practices that don’t require much equipment. They may even choose to mail remedies or supplements so that they don’t have to carry a large inventory of products with them.
Dr. Gardner found it difficult to maintain a clinic when she was primarily doing housecalls and telephone consultations. The overhead and time required to keep up the administrative side of things and the facility itself took away from her ability to spend time with clients and their animals. She discontinued the office and went back to working with all patients either through housecalls or telephone consultations. Because of this, many of her clients maintain an additional veterinary relationship where the animal can be taken for bloodwork or other laboratory tests as needed. This vet can act as a backup in a more urgent situation as well.
Not all health situations are conducive to treatment at home. It is important to know exactly what kinds of treatments your housecall vet can provide. Dr. DiLeva started her housecall practice with a fully equipped mobile clinic. She could provide any service, including those requiring anesthesia for surgery, either in the client’s home or in her mobile clinic parked just outside.
After opening her office, Dr. DiLeva found the complete mobile clinic was redundant. Now her housecalls are for more simple exams and treatments such as acupuncture and herbs. She travels to these appointments with at least one assistant who helps her draw blood and facilitate the examinations.
A veterinary appointment at your home may even help solve a previously unresolved health or behavioral issue. Environment can be a crucial piece of the puzzle, and while most animal guardians attempt to convey all the information that is pertinent to their dogs’ cases, they may leave out something important. They may not recognize the significance of a detail, or may not even notice a particular situation. Sometimes when the veterinarian can actually see the dog’s environment, she can make a link that otherwise would be missed.
Dr. DiLeva discovered this with a six-month-old black Labrador puppy who was having seizures. While on a housecall to the family, Dr. DiLeva noticed that they lived in an older home that was undergoing renovation one room at a time. Near the puppy’s crate, areas of the wall had been chewed. This triggered a thought with her – perhaps the seizures were caused by lead poisoning.
In fact, blood testing did show that he had been exposed to toxic levels of lead. This discovery also led the family to test their child, who also showed excess blood lead levels. Dr. DiLeva was able to treat the puppy, and the family was able to take care of the environmental situation as well as their own health before a more significant impact was felt.
How to find your housecall vet
The best option for finding a vet that provides housecalls is a referral from a trusted source. Start asking around. Your local animal “health food store,” doggie daycare, or even the dog park are good places to begin.
You can also check the online listings of the American Association of Housecall Veterinarians. The organization lists member practitioners online (athomevet.org), but does not have a referring phone number or address. Keep in mind that this listing includes all types of veterinarians and does not delineate between those who practice holistic, alternative, and complementary modalities and those who use only conventional veterinary medicine.
It may be helpful to contact the veterinarians in your area who are listed with various holistically oriented organizations such as the American Holistic Veterinary Medical Association, the Academy for Veterinary Homeopathy, or the International Veterinary Acupuncture Society.
Be sure to find out all the particulars before making an appointment (see sidebar, below). When starting a new relationship, it’s always a good idea to reduce the possibility of unpleasant surprises.
Getting the most out of a housecall visit
After finding a veterinarian who provides the services you’re interested in, it’s time for your first appointment. The more preparation you do in advance, the more you can relax during the actual visit and focus on the health and well-being of your dog.
Remember that just like at the vet’s office, sometimes you will need to be flexible with scheduling. Dr. DiLeva schedules a 30-60 minute range of time rather than a set appointment time. “Weather, traffic or an unexpected treatment can affect the schedule,” she says. Know your vet’s policy on scheduling and allow for problems with traffic or emergency situations.
Determine how your dog behaves when visitors come to the house. Is he nervous or shy around newcomers? Or, conversely, if your dog has a tendency to be reactive or even aggressive around strangers in the home, perhaps housecalls aren’t the best option. Or, the vet may ask you to use a muzzle to ensure the safety of everyone involved. In any situation, it makes sense to have him contained in a safe and non-stressful manner.
“Don’t get in a confrontational situation to begin,” suggests Dr. Gardner. She has found avoiding a greeting at the door is very important with any type of dog. Containing the animals in a different area until she is in the house can decrease these types of problems. Once she is in the house and settled in the room where she’ll be working with the dog, then the dog can come in for his greeting. Many dogs will accept her presence and settle more quickly in this manner.
It can be distracting, disruptive to the doctor’s schedule, and just plain rude to keep a veterinarian waiting while you attend to other household matters during a housecall. Allow the answering machine to take phone messages, and make any communications with other household members as brief as possible during the vet visit.
Parents of small children may find that it is easier to supervise their kids with a veterinarian in their home than to bring the children with the pet to an animal hospital. However, parents should discuss the doctor’s visit with their children in advance, asking for the kids’ cooperation in not distracting them, the dog, or the doctor.
It can be very helpful to the veterinarian if you have thought about and prepared a great location for her to examine your dog. It should be a comfortable room for the dog, with plenty of light available for the vet. If the floor is slippery, you can use a rubber-backed bath mat to provide a soft, comfortable place for your dog to be examined. Practice having your dog lie on the rug and permit a brief mock examination, giving her lots of cookies and praise for her quiet compliance. This sort of preparation can save time when the vet arrives.
Also, prepare by writing down specific questions, problems, or issues, suggests Dr. Gardner. Just like when you actually go to the clinic it can be easy to forget some of your questions at a home visit. Often, it is even easier to become distracted at home than at the clinic. You are likely to get much more out of your visit if you are able to keep on track and focused.
At first glance, housecalls may seem more expensive than an office visit. Dr. DiLeva charges $44 for an office exam and $59 plus mileage for a housecall. Additional animals are seen on the same visit for a reduced fee.
While her housecall fee is higher than her office fee, there are other types of savings. You don’t have to spend time traveling to the appointment. In addition, there is the benefit of convenience and maybe saving your dog from undue stress, fear, or the possibility of carsickness. Plus, the entire appointment is spent with the vet personally, rather than with a tech or in the waiting room. You have the vet’s undivided attention once she is at your home for the appointment.
Also With This Article
Click here to view “When a Difficult Event – Euthanasia – Is Made Far More Difficult”
———–
Shannon Wilkinson is a TTouch practitioner who lives with two dogs, two cats, and a husband in Portland, Oregon.
Calmative Herbs for Canine Panic Attack Occurrences
Dark clouds boil on the horizon, and a slow rumble of distant thunder delivers a slight vibration in the window panes. Jake, a large long-haired Chow-mix, is already nervous. He paces the living room, wild-eyed and panting, his body trembling with anticipation of the first dreaded clap of thunder. When it strikes, he tries to hide under the coffee table, and just like last time, he is too big to fit. The very same vase that was glued together after Fourth of July is reduced to a heap of jagged shards.
Jake’s problem is not uncommon. Millions of dogs have panic attacks, some quite severe – and each one is unique to the individual and the circumstances that trigger his or her fear.
Take the case of Mercury, a rescued Greyhound in San Diego. Terror comes whenever his people invite company over. He whines and barks, interrupting conversation, and sometimes getting so excited that he throws up his dinner, ruining the party for everyone.
Mitsy, a miniature poodle who lives in an upstairs apartment on Manhattan’s East side, has panic attacks, too. Although she is a show dog who enjoys meeting people, she is terrified of the groomer. And although each grooming ends with a tail-wagging romp around the salon with a gourmet cookie that she must dream of between visits, her anticipation of buzzing trimmers and squirting hoses is too much. With each visit she hides under the car seat, then leaves a trail of fear-forced urine between the car and the grooming table.
Although chronic behavior problems may be due to underlying nutritional, emotional, or physical health issues, most sudden-onset cases are caused by the fear or confusion of a stimulating event. Finding a lasting cure for your dog’s phobia can be difficult, and the stimuli that triggers your companion’s panic attacks might be impossible to avoid.
However, the intensity of her attacks may be safely minimized with the use of calmative herbs – those that promote relaxation and help take the nervous edge off exciting events.
One of the greatest advantages of using calmative herbs is the gentle manner by which they can promote relaxation without affecting mental capacity or physical performance. The medicinal effects of the herbs I mention in this article are very subtle; they help take the edge off nervous anxiety, but do not induce a state of sluggishness or impaired consciousness.
However, it is important to note that each and every dog is unique in what their bodies and behavioral traits require. Some herbs work well in some dogs but not others. Likewise, an herb that is appropriate for calming down dog A may be a poor choice for dog B. For example, valerian will sometimes make a hot, red-tongued, perpetually panting dog grumpy. For such a dog, passionflower, lemon balm, or skullcap may be better.
It also makes little sense to increase the dose of an herbal calming remedy that does not appear to be working well. Instead of running the unnecessary risk of nausea (the most common side effect of overdose), it is better to opt for a different herb – one that is better suited to the individual and circumstances.
It is also important to remember that calmative herbs should not be used within 24 hours of anesthesia or in combination with sedative or antidepressant drugs. Although safe and forgiving (especially when compared to most pharmaceutical drugs), most calmative herbs work their magic by acting upon the central nervous system. Therefore, they may add to the effects of drugs that work by similar means.
Following is a descriptive list of four calmative herbs that I frequently recommend for dogs. You will see that each one possesses one or more qualities that make it unique and especially useful in specific circumstances.
Any or all of these herbs can be combined to create a multi-purpose formula that will appeal to a broad variety of individuals and needs. For instance, I frequently use and recommend a liquid extract formula that combines valerian, skullcap, oat flower, and passionflower. This formula works well as a general-purpose herbal calmative in most dogs – even the aggressive, hot-blooded types for which valerian, if used alone, is not indicated.
Valerian (Valeriana spp.)
Valerian is, without doubt, the most widely recognized herbal sedative in existence. As a sedative, valerian works safely and gently to help calm the nerves and achieve physical relaxation. It does not induce an altered state like one would expect from a prescription sedative or from consumption of alcohol.
Herbalists use valerian for insomnia, nervous anxiety, and to help the body relax in the presence of physical pain. It is very useful for calming animals during thunderstorms, trips to the vet or groomer, or to help your companion rest after surgery.
When employed as a sedative, valerian is most effective fed in small doses, given several times daily over a period of several days. This is especially true when it is used in anticipation of a high-anxiety event, such as a planned interstate trip or a show. In these circumstances, dogs can be fed five drops of a low-alcohol valerian tincture, three or four times daily, starting three days prior to an anticipated fearful event.
In the digestive tract, valerian serves as an antispasmodic, making it useful in situations where nervousness is compounded by a spastic colon or an upset stomach.
Keep in mind, however, that valerian may have a reverse, stimulating effect in a small percentage of animals. If this happens, simply stop use and opt for another calmative herb. It also considered a “warming” herb, meaning that it may not be appropriate for dogs with a hot, aggressive disposition unless it is combined with other calmative herbs.
Skullcap (Scutellaria laterifolia)
For centuries, herbalists have recognized skullcap as one of the most effective nerve-calming herbs available. It is commonly used for acute or chronic cases of nervous tension or anxiety, and to help relieve pain from nerve-related injury or disease.
Skullcap is useful for general nervousness and excitability in dogs and cats, especially when the animal’s condition is characterized by jumpiness, trembling, or oversensitivity of the peripheral nerves. It is also useful for relieving nervous tension related to pain or a traumatic experience.
Skullcap acts to moderate an animal’s responsiveness to physical or non-physical stimuli, and helps alleviate general restlessness and nervous twitching. This makes it very useful in high-strung felines who are recovering from a frightful experience, but who need all of their survival mechanisms intact during their daily outdoor adventures.
Oat (flowering tops of Avena sativa)
The flowering tops of the oat plant are an excellent nervous system tonic for aging or debilitated animals. This herb contains considerable amounts of protein (gluten), vitamins, and minerals (especially calcium, manganese, iron, copper, and zinc) that are essential to the maintenance of health.
It also contains various alkaloid, sterol, and flavonoid constituents that act together to safely optimize nervous system functions while stabilizing the highs and lows between nervousness and mental lethargy.
For instance, when fed in moderation to animals with chronic nervousness, oat tends to have a calming effect, but when fed to debilitated animals, it tends to stimulate the nervous system. Oat flower tea or tincture is an excellent choice for animals recovering from exhaustion, or for those suffering from depression disorders.
It is known to improve nerve transmission, and can be useful in problems such as epilepsy, tremors, paralysis, and twitching. It is a very good tonic for nourishing the body and strengthening nerve function following periods of sedation or anesthesia.
Passionflower (Passiflora incarnata)
Passionflower is my first choice for fear-biters and other dogs who take on aggressive behavior during stressful situations. It is indicated where valerian is not – for hot-tempered animals or rare instances where valerian has a reverse, stimulant effect.
Passionflower is an excellent choice for taking a bit of the nervous edge off of jealous types who don’t want other dogs to visit their homes or who insist on being the grump of the toy party at doggie daycare.
How to feed these herbs
A number of calmative herb products manufactured specifically for use in dogs and other companion animals are available. Many come in the form of pills and capsules, while others are in liquid extracts. Some products also contain melatonin or other nonherb, calm-inducing supplements. Virtually all natural calming products are most effective when fed prior to actual need. By feeding the remedy to your companion 20 minutes to an hour before he will be exposed to his stress triggers, you allow the active constituents to be fully absorbed and working when chaos ensues.
Also With This Article
Click here to view “Holistic Help For Everything”
Training the Hearing Impaired Dog
[Updated December 10, 2018]
DEAF DOG TRAINING: OVERVIEW
– Consider adopting a deaf dog if you want a dog who does not bark at environmental noise.
– Teach your deaf dog a “look at me” or “watch me” signal first. This makes it easier to add hand signals to cue other behaviors later.
– Owners of elderly dogs should consider teaching their dogs hand signals; hearing loss is common in very old dogs.
Each year, as many as tens of thousands of dogs are born or become deaf. Unfortunately, given the number of hearing-impaired canines, there is a lot of misinformation promulgated about deaf dogs, even among dog lovers. Well-meaning but misinformed breeders and other “experts” commonly perpetuate myths about deaf dogs – that they are difficult to live with, hard to train, aggressive, and that they are only suitable dogs for a few “special” people. But the people who really know deaf dogs – those who live with and love them – tell a very different story.
“We got our first deaf dog when going to a pet fair ‘just to look’ at the cute dogs,” says Deb Sell, an animal chiropractor in Prunedale, California, and the proud guardian of four dogs. “We already had a 1½- year-old Aussie mix, Hawi (pronounced Ha-Vee; it’s Hawaiian), and really hadn’t planned on getting a second dog.”

But when Dr. Sell and her husband Stacey got to the pet fair that night, they saw one cute little white dog quietly watching everyone and became intrigued by her calm nature. They didn’t adopt Echo right away. Deb and Stacey went home that evening without her, but couldn’t stop thinking about her all week.
“We decided that if she was at the pet fair the following Friday night, we could consider adopting her. As fate would have it, she was there!” Echo soon came to live with the couple. Echo would begin for Dr. Sell what some might consider a “calling” into the world of living with and loving deaf dogs. The Sells now share their home and lives with three deaf dogs – Echo, Nefe, and Cooper – as well as their hearing dog, Hawi.
Suzan Mark and Gary Lomax of Santa Cruz also found their deaf dog, Cleo, somewhat through chance. They were visiting a local shelter, searching for a small dog, when they first met Cleo. Anything but a small dog (she is a Dalmatian), Cleo nonetheless caught their attention when in the midst of kennels full of barking, jumping dogs, she came to the kennel door and sat looking at them.
“It was as if she was saying, ‘OK, I’m ready to go home,’ ” says Mark. Not knowing Cleo was deaf, they went into an exercise yard to meet with her. It was then that one of the volunteers at the shelter mentioned that she might be hard of hearing. Gary experimented by clapping his hands over Cleo’s head. When he got no response to the sound, they realized that she was probably completely deaf.
Suzan and Gary also went away that day without Cleo. “We just weren’t sure about having a dog with a perceived handicap,” says Mark. They were also concerned that a Dalmatian might simply have too much energy for them.
The couple left the shelter with Cleo on their minds and in their hearts. Though they did look further for a small dog, they also did research to find out more about living with a deaf dog and living with a Dalmatian. They decided it just might be something they could do.
“We were still very nervous. We tried to think about all of the advantages – like she wouldn’t bark at the doorbell!” In the end, though, it was Cleo’s personality, not the fact that she could or could not hear, that won them over. “She is just a really sweet dog!” says Mark.
Why are Some Dogs Deaf?
Dogs are deaf for many of the same reasons that some people are deaf. Many deaf dogs are born that way – called congenital deafness – and there is often a genetic component. While the causes of genetically determined deafness in dogs are not completely understood, experts seem to agree that in many cases there is a relationship to a dog’s coat and eye coloring.
“I think that everyone agrees,” says Jack Edwards, Executive Director of the Deaf Dog Education Action Fund (DDEAF), “that the genes for merle patterning that affect the color of individual hairs, the spotting patterns (especially the piebald series) that overlay whole sections of coat color and even eye color, all carry a portion of the code that determines whether a dog can hear or not.” But there may be other, less understood, genetic factors involved as well.
Edwards also notes other reasons – not related to color or pigment – that may cause a dog to be born deaf. A malnourished mother dog, birth difficulties, illness during pregnancy, plus the normal occurrence of birth defects can all be factors.
Dogs, just like people, can also lose their hearing later in life. Illness, infection, or injury to the ear can cause deafness. Older dogs may also experience a sudden or gradual loss of hearing. Dogs can be deaf in only one ear (unilateral), in both ears (bilateral), or experience only a partial deafness.
Many people with deaf dogs know their dogs are deaf without having any special medical evaluation. Some people do “sound tests” at home, much the way Gary Lomax did with Cleo at the shelter – whistling, clapping hands, or making other noises to see if the dog responds. These are not foolproof testing methods, as a dog may respond to the vibration of a sound or the movement of the air caused by making the sound, and appear to hear a certain sound when she does not. However, home tests can be helpful indicators and are a way for people to confirm what they may suspect.
For dog guardians who want to know absolutely the extent of hearing loss, there is a procedure called a “brainstem auditory evoked response” (BAER) test that measures hearing loss through measuring brain responses. Electrodes are placed under the skin on the dog’s head and hooked up to a computer that records the brain’s response to sounds. The test does not appear to cause the dog any pain, but some dogs do become agitated because of being restrained and because of wires dangling about their faces. BAER tests are performed at some university veterinary schools, hospitals, and specialty clinics.
“Special Needs” Dogs
Sell, Mark, and Lomax all agree that living with a deaf dog, for the most part, is really not so different than living with a hearing dog – they are, after all, just dogs! Some are friendly, some are shy, some are cautious, and some approach life with gusto. Each dog – hearing or deaf – has his or her own personality characteristics and needs. Deaf dogs do not have “special needs” per se. Sell emphasizes that living with her deaf dogs has “taught me that deafness is such a non-issue when it comes to dogs.”

DDEAF’s Jack Edwards agrees that deaf dogs really don’t have “special needs.” He emphasizes, “Every dog needs food, water, shelter, and routine veterinary care. They need owners to love, exercise, and train them. They need protection from man-made dangers like household chemicals and street traffic and that nasty little boy down the street. Whether they are deaf from birth and unaware that something is missing or deaf from old age where the sounds of life slowly fade away, deaf dogs do not have any needs beyond those of every other companion animal.”
Edwards argues that “special needs” are those that take extra care or work. He cites examples of dogs with medical conditions that require specific diets or medications, dogs with allergies and skin problems that need special shampoo, or even dogs who have behavioral problems that require additional training or behavior modification as having “special needs.”
The exception may be a dog that experiences a sudden deafness later in life. “There are differences when working with dogs who became deaf at different times,” says Edwards. “Congenital and geriatric deafness are really not a lot different. One never heard anything and the other learned to compensate while the surrounding world grew quiet. The biggest challenge working with these dogs is getting the owners past the initial shock and ‘what do I do now’ stage.”
“In the case of sudden-onset deafness, whether from a trauma, a toxic reaction, or a surgery, it is a little more difficult,” Edwards says. “These dogs are used to getting information about their surroundings that is no longer available – and they have grown to depend on that input. They do have a special, albeit temporary, need. You may have to help them adjust the changes they are living through because of suddenly not being able to hear.”
But there are other considerations for a person considering adopting a dog who was born deaf. One in particular, Sell says, is that you have to be much more careful about letting your dog off leash in an unfenced area. In fact, many deaf dog guardians choose not to have their dog off leash at all unless the area is fenced.
Gary Lomax and Suzan Mark agree that the fear of losing Cleo, of her wandering off, is the one thing they consider significant and different about living with a deaf dog. A hearing dog, obviously, can also get lost or run away, but they believe Cleo’s lack of hearing would make it more difficult for them to locate her if she were to become lost. Because of their fear of losing her, they are careful to allow her off leash only in secured areas, such as a fenced dog park.
Deaf Dogs and Aggression
One of the predominant myths about deaf dogs is that they will become aggressive. To this day, some breed and rescue organizations recommend that all deaf dogs be killed as puppies, in part because of the belief that deaf dogs are aggressive.
Aggression is not caused by deafness. Aggression is linked to genetic predisposition and socialization. While there are no studies on the incidents of aggressive behaviors in deaf dogs as compared to hearing dogs, people who live with deaf dogs agree: a dog that has a sound temperament and is wellsocialized is much less likely to be aggressive, whether he can hear or not.
“I don’t believe there is any correlation between deafness and aggression. It’s a question of personalities and handling,” says Jack Edwards, Executive Director of the Deaf Dog Education Action Fund (DDEAF). He has come to this conclusion through sharing his home with five deaf Dalmatians, as well as through his experience as a trainer, and his extensive contact with other deaf dog guardians.
Edwards notes that through a deaf dog email list (with more than 1,100 members) the subject of aggression comes up periodically in regard to specific dogs (as it does on most email dog lists that discuss behavioral and training issues), but it is not a regular topic.
In addition, Edwards has helped plan and has attended six Florida Deaf Dog Picnics. These events are held in public off-leash parks and are open to everyone. Edwards says that these events have been attended by all sorts of dogs, from Boston Terriers, Dachshunds, American Pit Bull Terriers, and Catahoulas, to the ever-present Australian Shepherds, Border Collies, Boxers, and Dalmatians. “I have yet to see any problems or scuffles started by a deaf dog at one of these events.”
This of course does not mean that deaf dogs do not have aggression issues – they are, after all, dogs. But the incidence of aggression in deaf dogs does not seem to be any higher than among the general dog population. And specific training and behavior modification used to deal with aggression issues works just as well with deaf dogs as with hearing dogs.
Dogs Don’t Speak English
Of course, people who decide to adopt a deaf dog will need to be willing to overcome any reluctance they may have to communicating nonverbally. Dogs, whose primary mode of communication appears to be body language, don’t seem to have a problem with nonverbal communication; they don’t depend on English or any other spoken language to begin with! But some people do fear that they will not be able to adjust to using hand and visual signals rather than words to communicate.
Mark and Lomax said they had expected communication to be a problem, but discovered that it really hasn’t been. Cleo, Mark notes, is very intuitive about body language and picks up on hand signals very quickly.
“A slight flick of the wrist tells her to sit,” she says, “and using your whole arm is like shouting at her.”
People who live and work with deaf dogs do develop a whole series of nonverbal communication signals – including facial expressions, body postures, hand signals, and even high-tech devices such as vibrating collars. Some of the communication signals are intentional. Others happen naturally, for example when the dog learns what it means when people open a certain kitchen cabinet or reach for the leash. Of course, many people continue to talk to their dogs, too. When people speak, we incorporate a whole slew of facial expressions that may actually prove beneficial in communicating in spite of the fact that the dog doesn’t hear the words.
Do you have to learn special hand signals, like American Sign Language (ASL), to communicate with a deaf dog? Not necessarily. For some people, adopting signals from ASL means that they do not have to invent their own. Others use a combination of ASL signals and common obedience hand signals. Still others use whatever hand signals come naturally. One advantage to using certain ASL or “obedience” style hand signals is that other people may also know them and be able to communicate with your dog. For example, if you take your dog to a training class, the instructor is more likely to already know traditional obedience hand signals.
Isn’t Training More Difficult?
Deaf dogs, like hearing dogs, do not train themselves. Just as with any dog, your job will be to devote time and energy to their training and socialization in order to help them become well-adjusted members of the community. The principles of training apply to a deaf dog in the same way they do to a hearing dog. The main difference in the way you train a deaf dog is just in the way you communicate.
“I expected it to be difficult and it wasn’t. ‘Deafies’ (at least the deaf Aussies I have) are so tuned in to your hand signals and body language, they seem to stay more focused on me when I am training them than a hearing dog,” says Sell. “We have been involved in agility training and use only hand signals to do so. Echo buzzes around the course like a pro!”
Just as when training a hearing dog, you must first teach a deaf dog to understand when you want her attention. This is akin to teaching a hearing dog to understand her name. You can choose a signal for her name or teach a signal for “look at me” or “watch me.” In addition, you can teach a physical cue, such as a tap on the shoulder, for attention. Some people choose to use lights or vibrating collars (not shock collars) to get their dog’s attention.
In addition, you will need to teach a deaf dog one or more reward marker signals, and signals that are the equivalent to verbal praise. If this seems like a lot, just remember that we must also teach our hearing dogs what these things mean. No dog automatically knows his name, nor does he know the word “good” is praise.
Special issues around training do come up in regards to calling your dog at a distance – especially if she is not looking at you. Using a laser light (shined in front of a dog who is looking away, not at his eyes!) or a vibrating collar are two good solutions to getting attention at a distance, and thus being able to signal your dog to come.
“At the dog park,” Suzan Mark notes, “it is a little harder to get Cleo’s attention to call her back to us than it is with other dogs. Of course that does depend on who you are comparing her to – lots of dogs at the dog park don’t respond when they are called!”
Getting a Deaf Dog’s Attention
My students with deaf dogs frequently relate that their biggest challenge is getting their dogs’ attention, whether at home or out in the world. I watched one student, early in her training, do some incredible acrobatics to try and keep herself positioned in her dog’s line of sight. She seemed very happy when she realized she could teach her dog to look at her, instead. Here are some tips for getting a deaf dog’s attention (these tips work well with dogs who hear, too.)
• Reward “offered” attention
One of the most important ways to teach dogs to pay attention to you is to reward all “offers” of attention. This will encourage your dog to check in with you regularly, whether you ask for attention or not. At first, just for giving attention, you can offer a reward. In other words, if you are out on a walk and your dog looks up at you, give him a treat!
Once your dog starts to realize that checking in with you regularly earns rewards, you can start asking for additional behaviors before rewarding him. For example, if your dog looks at you expecting a treat, ask for a “sit,” then reward. Do continue to occasionally reward simply “checking in” with treats, play, or petting.
Jack Edwards from DDEAF suggests a game of “hide and seek” for teaching a dog to offer attention. “It starts out as ‘find me and get a reward.’ Then it turns into ‘whenever you see me, you get a signal to do something rewarding.’ Sometimes it’s a signal to go back to playing and sometimes it’s a ‘how fast can you get here’ recall. These games sure teach the dog to pay a lot of attention!”
• Hand signal for his name
Just as you teach a dog to respond to “Max” or “Spot,” you can teach a deaf dog to respond to a signal that means, “I’m talking to you now.” A simple finger point or a wave will each work and are easy to teach, but any signal will do.
To teach that the finger point or wave means “Max,” start by simply pointing or waving at the dog, then offering a reward such as a great treat. Throughout your daily life, use his “name signal” much as you would a verbal name. If you are about to feed your dog, point or wave in her direction, then walk to the kitchen and prepare his dinner. Before walks, point or wave to your dog, then get out the leash.
Soon the dog will respond to the hand signal just as a hearing dog would respond to the sound of his name spoken verbally.
• “Look” or “watch me” hand signal
Many dogs, hearing and deaf, need to be taught that they must pay attention at times. A “watch me” signal is a great way to teach them that they need to focus on you.
Take a treat between your thumb and middle finger. Briefly swipe the treat under your dog’s nose, then bring your hand up to your face and point your index finger to your eyes. As your dog’s eyes follow the treat to your eyes, give your “thumbs up” or other reward marker and give the dog the treat.
As your dog learns the game, begin to do the hand motion without having a treat in your hand. Do continue to give your dog the “thumbs up” and a treat for looking at your face.
Keep playing the game, increasing the length of time your dog “watches” you, before giving the thumbs up and the treat. One to three minutes of sustained eye contact is a good goal for a solid “watch me.”
Once your dog knows the signal from sitting in front of you in the living room, teach it with your dog in different positions. For example, ask him to watch you as he walks beside you as if walking on a leash. Then begin to practice in a variety of environments.
• Tap on the shoulder
In order to avoid the acrobatic antics of trying to make your dog see a hand signal, you can teach a physical cue that means “look” or “watch me” too. I like a tap on the shoulder or rear end as the signal for “Hey, look at me now.”
Start by tapping your dog on the shoulder when he is already looking at you, and offering a treat. Then move to tapping on the shoulder and treating when he is off to your side. Gradually move so that you are behind your dog. Tap him on the shoulder, and when he turns his head, give him a treat.
Once he knows that tapping means looking your way for a treat, you can add the other steps for “watch me.”
Clicker Training for Deaf Dogs?
Of course! Clicker training is simply a style of training that uses a “reward marker” to tell the dog when he “got it right!” With hearing dogs, people most commonly use a “clicker” or a word such as “Yes” as the reward marker. With a deaf dog, you can use the flick of a penlight or a hand signal such as a “thumbs up” for your reward marker.
To teach your dog that the flash of a penlight or a “thumbs up” signal means the dog just got it right, simply pair the signal with a treat. For example, first do a “thumbs up,” and then give your dog a great treat. Repeat 20 to 30 times in a row.
Now you can use your “thumbs up” the same as you would a clicker. For example, to shape a “sit,” wait for your dog to offer a sit or lure him into position just as you would a hearing dog. When he sits, give a “thumbs up” followed by a treat. As with a hearing dog, remember to get the behavior first, then put it on cue. When teaching the dog to sit, make sure your dog will, first, offer the sit reliably. Then give your hand signal for “sit” just before your dog sits. When he sits, immediately give him a “thumbs up” and a treat. He will quickly learn that your hand signal cue means sit, and the thumbs up means he did something right.
In addition to teaching a reward marker, consider teaching a signal such as a hand clap motion that means “good dog” or “keep going.” This can help bridge the communication gap when a dog is trying, but hasn’t quite hit the target for a “thumbs up.” A “reward marker” is a visual signal that alerts the dog that she has done the right thing and can expect a reward.
From here, it’s all up to you. You can teach a deaf dog as many behaviors and tricks as a dog who hears.
Using Technology with Deaf Dogs
High tech devices are not necessary when training a deaf dog; many people do without them just fine. But they do offer another alternative for getting a dog’s attention.
Consider a vibrating collar. (Not a shock collar. Be careful if you get a collar that doubles as both; you could accidentally shock your dog when you mean to vibrate.) The Deaf Dog Education Action Fund has a list of vibration collar manufacturers on its Web site (deafdogs.org). By itself, a vibrating collar will not teach a dog anything, but if you pair the vibration with great rewards like chicken or tuna, your dog will learn to look at you when he feels the vibration. This signal can work to get your dog’s attention when he is across the park from you.
You can use a laser light in a similar fashion to get a dog’s attention. Flash the light in front of the dog on the ground or another surface, and then give the dog a treat. (Be sure not to flash the light directly at the dog, as it could damage his eyes.) A laser light can be used in the daytime as well as at night and some lights can focus a spot up to 100 yards away.
Other Attention-Getters
Stomping your foot or banging a door can get your dog’s attention because they create a vibration that the dog may feel. Flicking the light switch or flashing a flashlight will attract their attention visually. Waving your arms in a wide circle over your head and out at your side can get a dog’s attention through his peripheral vision. Each of these will work even better if they are paired with a great reward.
“All Done” Signal
When you spend a whole lot of time teaching a dog to pay attention to you, you can end up with a dog who will never leave you alone. This can be trying for both the dog and the person!
By teaching your dog an “all done” or a release signal, you have a way to tell your dog when he is off duty and no longer needs to give you his undivided attention. This one is easy; simply pair a signal such as a flat hand or a “go away” motion with absolutely no attention from you! Your dog will soon learn that when you signal “all done,” the game is over.
Startling Myths About Dog Deafness
When I began working with my first student with a deaf dog, I did research trying to discover special issues that come up with deaf dogs. One of the “myths” surrounding deaf dogs that I saw repeatedly was that if you startle a deaf dog, they will bite.
“I think you can just take ‘deaf’ out of that sentence,” says Mark. In other words, if you startle any dog, he might bite. Hearing dogs can be startled too, and any dog who is frightened might react defensively. Deaf dogs aren’t necessarily startled more easily, just differently. And not all dogs react to being startled with aggression. Take Cleo, for example. “You can startle her and she reacts. But she thinks good things are going to happen!” Mark says.
The combination of Cleo’s good nature, possibly coupled with startle conditioning exercises shortly after they brought her home, has made startling a non-issue in their life. In fact recently, while playing at a local dog park, two young children ran up behind Cleo and grabbed her in a big hug. Cleo was obviously startled, but seemed to simply enjoy the experience. She greeted the girls, then happily received their pets and hugs.
Jack Edwards agrees. “It is my opinion that all dogs startle to unexpected stimuli – hearing dogs even more so because of the additional surprises. The phrase to ‘let sleeping dogs lie’ was not written about deaf dogs but has been passed through generations of people who know better than to startle a dog.”
Edwards does also emphasize, however, that dogs who have suddenly become deaf may be more likely to suffer all the negative side effects of being startled. “These are the dogs where you really do need to take the time to help desensitize them.”
Like hearing dogs, not every deaf dog will be as easygoing as Cleo about being surprised or startled. For example, Deb Sell’s Border Collie mix, Nefe, did have trouble with people suddenly “appearing” in the doorway at her office. (This issue may be more related to her being a Border Collie, than to her having trouble hearing – one of my herding dogs has had a similar problem when she accompanies me to work.) Through counter-conditioning, Nefe has learned that people appearing in a doorway is not such a scary thing after all.
Socializing any dog to lots of people, places, sites, and touches will help him learn not to be as startled by any one factor. In addition, people living with deaf or hearing dogs can consciously condition their dogs so that they actually enjoy being startled. By pairing the dog’s favorite treat with a “startle,” she can learn, like Cleo did, that being startled means good things happen.
Speaking Louder Than Words
I must admit that I wanted to write this article to help dispel myths about deaf dogs, and to help put a wedge into the shameful practice of killing deaf dogs simply because they cannot hear. But I had a second motivation: to share with other caring dog people that living with a dog that has a physical difference isn’t about being altruistic or noble. Rather, it’s about being open to sharing your life with an animal who comes your way – the one who is meant to be your companion whether she can hear or not.
Sell notes, “People shy away from adopting a dog that is ‘defective.’ Those people are really missing out on sharing their life with a very special animal. I truly believe animals come into our lives for a reason. I think mine are here to teach me that a ‘handicap’ is something that you need to look beyond, to see the real inner person (dog). If we had not adopted these three deafies, we would have missed out on one of life’s great gifts . . . an amazing and strong bond between people and their dogs.”
Suzan Mark and Gary Lomax began their journey with Cleo with some apprehension. They were understandably nervous about adopting a deaf dog. But now, after having shared their life with her, when asked if they would do it again, Suzan and Gary say, “For sure! She picked us.”
When asked if she would do it again, Sell just laughs. “Well, I think the fact that we have already adopted three pretty much answers this question!”
Mardi Richmond is a writer, editor and dog trainer who lives in Santa Cruz, California. She is grateful to Jack Edwards of the Deaf Dog Education Action Fund, Dr. Deb Sell, and Suzan Mark and Gary Lomax for sharing their experiences for this article.
Holistic Dog Care and Holistic Checkups for Athletic Dogs
By Lorie Long
Being married to a NASCAR fan means that I spend a number of Sunday afternoons watching precision-engineered stock cars and their steely-eyed drivers burn up a race track for 500 miles or so, pushing the limits of man and machine.
A few cars crash in catastrophic events that render the vehicle totally unfit for future competition. Other cars get “tight” or “loose” in their handling, receive a ding or lose a body panel, and limp to the garage under their own power, misaligned but still operational. The top finishing cars escape such misfortune, careening over the finish line in apparently good form, but having been supported before, after, and throughout the race by a professional pit crew.

The NASCAR races bring to mind my agility trials and other canine performance events. At these competitions, handlers from around the region converge on the site, offering their canine partners the chance to jump, twist, climb, balance, and run at high speed through obstacle courses, catch an airborne Frisbee, rocket over jumps with a tennis ball in their mouths, or herd flocks of recalcitrant farm stock. Here, too, a spectator may witness tragic “crashes” and temporary setbacks experienced by some of the competitors.
I have become resolute in my desire to do all I can to prevent my performance dogs from crashes, burns, and burnouts. As the pit crew chief for my canine athletes, I have decided to take the steps necessary to responsibly prepare my dogs for their active lifestyles, utilizing the best supportive and preventative therapies.
I enlisted the assistance of Chris Bessent, DVM, a Wisconsin veterinarian who uses chiropractic, acupuncture, and Chinese herbs in her canine and equine sports medicine practice. I asked her to help me develop a routine maintenance regimen – a sort of “pit stop” program – for my Border Terriers competing in agility. Both dogs have good conformation, solid working ability, and a clean record (so far, no injuries!).
Dr. Bessent explained to me how she performs a thorough maintenance evaluation of her athletic canine patients and then applies holistic therapies to support them in their active lifestyles: chiropractic, acupuncture, nutriceuticals, dietary supplements, pharmaceuticals, Chinese herbs, therapeutic massage, and warm-up stretching exercises. The program that Dr. Bessent outlined to me could actually serve as a model for any canine athletic health-maintenance plan.
Thorough evaluation
It goes without saying that every dog should undergo an annual health examination, complete with laboratory tests to evaluate blood chemistry and composition. Hard-working dogs – whether they are athletes or used for emotional therapy work – should be taken to the veterinarian for additional exams if their performance or attitude sours.
In addition to conventional veterinary examination techniques, Dr. Bessent employs an age-old practice, taken from traditional Chinese medicine: tongue and pulse examination of the dog. Dr. Bessent checks the dog’s tongue, looking for a nice pink color. Any indication of bright redness, purple, yellow, or paleness of the tongue suggests a disharmony or imbalance of the energy flow in the dog’s body.
Dr. Bessent immediately follows the tongue evaluation with a pulse evaluation. Other assessments or holistic treatments, such as chiropractic or acupuncture, release endorphins into the dog’s system that can change the dog’s normal pulse rate and affect the quality of Dr. Bessent’s initial appraisal, so tongue and pulse evaluations are the first order of business.
With the tips of her fingers, Dr. Bessent feels the dog’s pulse at the top, midpoint, and bottom of the dog’s right and left hind legs, checking both the “deep” and the “superficial” qualities of the pulse. She carefully monitors the balance and harmony of the energy flowing through the “meridians” or energy pathways of the dog’s body.
A “tight” pulse, for instance, may indicate a stagnation of the energy in the liver. A “slippery” pulse, or one that “feels like a pearl” flowing through the body, may indicate excessive phlegm in the body. A pulse that is too deep may indicate an energy deficiency. In order to promote the free flow of energy, or life force, in the dog’s body, Dr. Bessent corrects any of these imbalances with acupuncture treatments and Chinese herbs.
In many cases, especially in dogs who are active and do not have a diagnosed injury, the pulse is already well balanced. For these dogs, Dr. Bessent recommends two Chinese herbal combinations that support general good health and athletic potential:
• Liu Wei Di Huang Wan, also known as the “Six Ingredient Pill” with Rehmannia.
• Tangkuei and Rehmannia, which helps to tone the liver as well as the kidneys.
These herbal combinations, or decoctions, which Dr. Bessent calls “herbal Gatorade,” benefit the bones in the lower back and nourish the kidneys, thereby toning bodily fluids and rehydrating the dog. The kidneys, known in Chinese medicine as the “flame of life,” support the flow of energy and fluids in the body, which is helpful even for dogs that are not very athletic.
You can readily purchase these Chinese herbal combinations at Chinese pharmacies, Chinese pharmaceutical Web sites, and directly from Dr. Bessent (see sidebar, below). However, no supplement should be added to your dog’s regimen without some support and guidance from your holistic veterinarian.
Joint and muscle evaluation
After appraising the balance of the energy flow in the dog’s body, Dr. Bessent checks the dog’s joints in both his spine and limbs.
In a maintenance evaluation, the veterinarian watches the dog move, looking for any deviations from proper alignment or movement, like one hip placed higher than the other, pacing (walking with the two left legs and then the two right legs moving forward at the same time, rather than the normal diagonal movement of the legs), dog tracking (the two front legs moving on a different front-to-back plane than the two rear legs), roaching (a rise or hump in the dog’s back), or a visible limit in the normal range of any joint motion.
Then, while the dog is standing, Dr. Bessent feels each joint of the spine, starting at the atlas (the first vertebrae of the neck) and occiput (the back of the skull), and continuing all the way to the tail. She checks for a lack of normal motion, usually due to a subluxation (a vertebrae out of position), too much motion, sensitivity, or tenseness during the examination that may indicate discomfort in that area of the dog’s body.
With the dog lying on his right and then left side, Dr. Bessent examines each of the joints in the dog’s front and hind limbs, from shoulder to toes in the front, and from hip to toes in the rear. She checks for pathologies like crepitation, indicated by a cracking, creaking, or popping sound in the joints as they move. She notes any tendency of the dog to pull away when she manipulates his joints, or any reluctance to complete the full range of motion.
The causes of joint crepitation can be as simple as the presence of gas pockets in the joints or a decrease in the viscosity, or thickness, of the lubricating fluid in the joints. Healthy joint lubrication fluid is almost as thick as jelly, but can become more watery with age or overuse, thereby reducing its effectiveness as a protectant.
Dr. Bessent recommends a glucosamine supplement to help restore the joint lubrication fluid to a more normal viscosity. More serious and complex causes of joint crepitation include arthritis, tendonitis, and bursitis, which may benefit from regular chiropractic treatments, acupuncture, and a combination of supplements in addition to glucosamine.
Based upon her survey of the dog’s conformation, Dr. Bessent works with the dog’s owners to make training recommendations that will reduce wear and tear in areas of the dog’s body at risk for injury.
For instance, dogs who are high in the back end or straight in the shoulders will benefit from a training regimen that reduces stress to the dog’s front end. Handlers can limit the amount of jumping they ask of their dogs in their training sessions, or alternate training sessions at low jump heights with sessions at regulation jump heights. Handlers can also train their dogs to hit the flyball box straight on rather than at an angle that directs the impact at the same single shoulder joint each time.
Dr. Bessent says she sometimes notes obedience dogs, who are usually worked on the handler’s left side, may tend to curve their spines and necks up and to the right during heeling exercises. Dogs with a tendency to develop neck injuries, like Dobermans, benefit from performing their heeling exercises on both sides of the handler to balance the strain on their necks.
Supplements
One of the most popular nutritional supplements for the relief of joint and soft tissue pain and inflammation is MSM (methylsulfonylmethane), a natural substance found in food and in the body. MSM provides biologically active sulfur, a mineral that is deficient in many diets and certainly lacking in therapeutic quantities.
Taken orally in the form of a powder or in capsules, this substance provides excellent maintenance support, especially to dogs with an inclination to develop tendonitis and muscle strains. Most of the agility competitors I know take MSM for their own well-being in addition to including it in their dog’s diet. Dr. Bessent recommends the following maintenance dosages of MSM for her canine patients:
• For dogs under 45 pounds: ¼ teaspoon two times a day for seven days, then ¼ teaspoon once a day thereafter.
• For dogs 45-90 pounds: ½ teaspoon two times a day for seven days, then ½ teaspoon once a day thereafter.
• For dogs over 90 pounds: ½ teaspoon given as indicated above should be adequate, but more can be given, based upon the dog’s response, up to 1 gram per 45 pounds of weight per day.
MSM is readily available at health food stores, pharmacies, and from discount vitamin suppliers.
After several years of studying canine dietary supplements to find just the right ones to recommend for her active canine patients, Dr. Bessent personally favors Canine Platinum Performance® by Platinum Performance Inc. (Buellton, California), and The Missing Link® by Designing Health (Valencia, California).
Developed in 1996 by equine veterinarian Doug Herthel, Platinum Performance sped bone and tissue healing and reduced the swelling after orthopedic surgeries in thoroughbred horses competing on the racing circuit. Dr. Herthel found that the product aided in post-operative healing, and produced a decrease in allergic reactions and a boost to overall health and energy levels in the horses taking the supplement. He suspects that most horses have diets deficient in trace minerals and, especially, in Omega 3 and Omega 6 fatty acids, a key ingredient in cell membrane repair. His investigations resulted in the Platinum Performance family of nutritional supplements for horses, dogs, exotic animals, and humans.
Canine Platinum Performance, a dry granular powder, is not a prescription drug, but is available only from a veterinarian or directly from Platinum Performance Inc. Although the company’s Web site states that an order requires a referral from a veterinarian, I purchased the product for my dogs simply by providing my primary care veterinarian’s name.
A one-pound canister contains a 60-day supply of the supplement for a 30-pound dog, and costs $15. Larger size containers are more cost-effective. The newest addition to the line is Canine Platinum Performance Plus®, with glucosamine added to the formula.
The Missing Link, also a granular powder, is more widely available from dog supply catalog houses and pet supply chain stores. It comes in a vegetarian formula, as well. A one-pound bag of The Missing Link costs $16 when purchased directly from Designing Health and will support a 40-80 pound dog for about 60 days.
Both supplements derive their Omega 3 and 6 fatty acids from flaxseed. If, at first, your dog develops stomach gas or other symptoms of not tolerating flaxseed well, Dr. Bessent suggests gradually building up the product in your dog’s diet or, if necessary, switching to a fish oil-based source of Omega 3 and 6 fatty acids.
Joint therapy
A less well-known but highly effective treatment for canine osteoarthritis and joint crepitation is Adequan® Canine (polysulfated glycosaminoglycan) produced by Luitpold Pharmaceuticals Inc. in Shirley, New York. Approved by the FDA and developing a following among small animal veterinarians as a preventative for highly active dogs at risk for developing arthritis, as well as a disease medication, Adequan Canine not only treats the pain of arthritis but also stimulates the cartilage repair processes.
Adequan has been used by large animal veterinarians on their athletic equine patients for many years. The drug is supposed to suppress the enzymes that eat away at joints, help to lubricate the joints, and reduce inflammation from overuse.
Adequan Canine is a prescription-only pharmaceutical administered by intramuscular injection. Many dog owners inject their own active and working dogs once a month, but others prefer that their veterinarians do the honors. Because of the route of administration, this drug is stronger and more effective than oral supplements like Cosequin®, but Adequan Canine also can be used in conjunction with these supplements. A single injection for a 45-pound dog costs about $20 – $25.
Physical therapy
Immediately before participating in a canine sport or performance activity, Dr. Bessent recommends working through some stretching exercises that take your dog’s joints gently through their range of motion. Here are a few exercises you can do with your dog:
• Straddle your dog behind his shoulders while he is standing, hold a treat in front of your dog’s nose and move the treat from side to side, encouraging your dog to bend his neck. Try to have your dog bend to touch your knee on each side.
• While your dog is standing, hold your hand against his chest and hold a treat in front of his nose. Encourage him to push against your hand and stretch his neck toward the treat.
• While your dog is lying on his right side, slowly stretch his left legs forward and back, holding each stretch for five seconds. Repeat with his right legs while lying on his left side.
• Teach your dog stretching behaviors like spinning in a circle left and right, bowing his head down, play bowing his entire front end on command, and “sitting pretty,” or “begging,” on his hind legs.
• Remember, never to force your dog’s body into any position or movement; just encourage comfortable motion.
After an agility-filled day, I enjoy giving my dogs a gentle rubdown. Indeed, therapeutic massage or hands-on soft-tissue work increases the flow of blood and lymph fluids to the large muscle groups of the body, carrying away the toxins and metabolic wastes produced by athletic activity. Massage also relieves tension, enhances muscle tone, and increases the flow of nutrients to the skin.
There are a host of different methods you can use, including direct pressure, stroking, kneading, compression, and cross-fiber massage. Dr. Bessent recommends enlisting the services of a professional canine massage therapist, both for therapy and to help you learn to perform the techniques that are most useful for your dog.
Some canine massage therapists offer massages at the site of agility trials and other dog sports events. As massage tends to relax muscles and sometimes makes dogs who are not used to having a massage “goofy,” Dr. Bessent suggests that handlers visit these massage therapists only after running their events. Actually, getting your dog used to a massage at home is the best way to gauge your dog’s reaction to a massage and to decide how to best incorporate it into your schedule. Stretching is the most appropriate warm-up therapy to engage in directly before participating in an event.
My new plan
After my consultation with Dr. Bessent, I have pledged to broaden the support therapies I offer to my dogs in order to sustain them both through many years of athletic activity.
In addition to the fresh, home prepared diet I regularly provide, along with pure, distilled water, my orders of Platinum Performance Plus and The Six Ingredient Pill with Rehmannia are on the way. I will begin sharing my own jar of MSM with my dogs in the future. After adding these supportive supplements to their diets I will consult with my veterinarian about incorporating Adequan injections into their healthcare routine when appropriate. And I’m committed to a monthly chiropractic adjustment and holistic evaluation for my dogs, rather than just the occasional visit.
As usual, I will retrieve my dogs out of their crates in plenty of time to stretch their muscles before an agility run. And they can both look forward to a rubdown when back at home or in the motel room, or perhaps enjoy a therapeutic massage at the site, after their events.
I hope to see you “in the pits” with your athletic, healthy canine companions.
Also With This Article
Click here to view “Selecting a Holistic Veterinarian”
Click here to view “Considering a Holistic Approach to Your Dog’s Health”
Click here to view “Non Traditional Treatments for Athletic Dogs”
———-
Lorie Long lives in Oriental, North Carolina, and is an avid agility competitor.
Whole Dog Journal Reviews Some “New and Exciting” Dog Toys
By Nancy Kerns
My husband is a diehard catch-and-release fisherman, and my Border Collie is a tennis ball maniac, so when I first saw Reel Dog, a toy that combines the concepts of fetch, tug, and fishing, I thought we had a real winner on our hands. I snapped one up and brought it home to try out.
Examining its packaging, I noted that its maker, Happy Dog Toys, of Phoenix, Arizona (a division of Farnam Pet Products), has created a small line of innovative interactive dog toys. I tracked down two more products from the line – Bubble Buddy and Tug Master– and tested all three.
I have some good news to report and some bad news. First, the good news: Happy Dog Toys is really on to something. Their products are highly appealing to playful people, so much so that they can’t wait to go try them out with their dogs. The concepts behind the toys are novel, creative variations on old favorite human/canine play themes: fetch, jump, tug. The company’s marketing and distribution network seems very advanced; the toys can be found in most of the “big box” pet supply chains and in many small pet supply stores, too.
Finally, Happy Dog Toys goes to the extra effort to conform to the ASTM testing standards of the toy industry, ensuring that the toys are as safe for your dog as they are for your children.
The bad news? None of the three interactive toys I tested performed quite as well as their packaging suggested. Each had a fatal flaw (or two) that kept me and my test dogs from fully reaping the riches of fun promised by the product’s design.
It’s my sincere hope that Happy Dog Toys continues to develop products like these, but my fear is that the toys’ shortcomings will discourage repeat purchases. Will the line of toys survive long enough to improve? I’ll have to wait and see. In the meantime, I have a lot of (I hope) constructive criticism to offer!
While I don’t often publish product reviews that don’t include at least one item that garners WDJ’s top (four-paw) rating (see sidebar, below), I’m doing that very thing this month. The Happy Dog Toys products are so engaging and so promising . . . and maybe other dog owners will find them less problematic than I did. Fortunately, the toys are not prohibitively expensive, so buy one anyway if one of them seems pretty fun to you, despite my criticism.
Reel Dog
The first Happy Dog Toy I saw in a pet supply store, Reel Dog is built along the lines of a child’s play fishing rod, but with a tennis ball (rather than some sort of hook or lure) at the end of a 30-foot line. The “fisherman” pulls the crank out a notch to release the line, and then casts the ball in the direction they want the dog to go. Ostensibly, the dog grabs the ball and the “fight” is on, with the fisherman providing resistance by pulling on the rod and cranking in the line, and the dog enjoying a novel game of tug.
The biggest problem I had with this toy is that it took only two games of tug for my canine “fish” to realize that they could win much faster if they grabbed the line, rather than the ball. Each of my first two test dogs (the ball-crazy Border Collie and a tug-crazy Lab) snipped through the line with their teeth within minutes. The line appears to be a cotton/poly cord, which proved very strong when reeling in even a large dog, but is not at all resistant to sharp teeth.
Also, while it’s nice that the toy contains 30-plus feet of cord, so a dog can enjoy a good dash on his way to fetch the ball, the reel that brings in the line is relatively small, so it takes a long time to land that fish! In addition, I found it very awkward to turn the crank that reels in the line with my left hand (since the crank is positioned on the left side of the toy handle); I thought it was due to my own inept technique. But my husband had barely touched the Reel Dog when he blurted out, “The darn reel handle is on the wrong side!” It wasn’t just me! It’s awkward for all right-handed fishermen.
On the other hand, perhaps the designers at Happy Dog Toys thought it would be easier for the average right-handed person to “play” the dog with his strong hand, pulling the dog toward him with the right hand and using the left hand to quickly wind in any line that is gained. I don’t know if this was their thinking, but after a little practice, I got the hang of it.
Happy Dog Toys also makes a huge number of simpler tennis ball-based toys, such as Tennis Bones (two balls affixed to either end of a plastic “bone”) and Tennis Buddies (tennis balls that look like little cartoony animals, with little arms and legs and faces attached). All these toys are constructed with specially made pressureless and double-thick natural rubber balls, which makes them virtually impossible to pop and chew.
Tug Master
If you’re like me, you won’t be able to get this phrase out of your head, once you’ve heard the recorded voice inside this toy repeat its eponymous refrain, spoken in a deep superhero voice: “Tug Master!”
Again, this novel toy has some engaging features. It has two handles: a hard plastic handle for a person to pull in, and a softer plastic one for a dog to grip with his teeth. A spring or similar mechanism provides resistance, so the handles can be (with great effort) pulled in opposite directions to effect greater or lesser scores on the “Tug-O-Meter,” a gauge that records the strongest tugs. (This toy, I should note, is intended for big, strong dogs.) As the handles are pulled, an electronic voice barks, exhorts the contestants to “Get tough!” or suggests “You’re the dog; you’re the big dog!”
Unfortunately, I couldn’t convince even Paws, my rowdiest Labrador acquaintance who is a huge fan of tug o’ war, to take hold of the end of the toy intended for him. He didn’t appear to be either put off or encouraged by the recorded noises; he just didn’t appear to be comfortable gripping the semi-hard plastic handle.
As soon as I tied a rope toy around his end of the Tug Master, however, Paws was off to the races. He pulled and pulled with delight . . . but he does that with any old rope. I tried to get several other dogs to play Tug Master with me, but couldn’t find a single one that would grip the hard handle. Maybe your “tug master” would’t mind mouthing the toy. You won’t know unless you try it.
Even though I’m not getting much tug-time, I like to keep the toy around, mostly so I can press the button that makes it chortle, “You’re the dog!”
Bubble Buddy
Even after the first two disappointments, I was certain that I would be pleased with Bubble Buddy. Many dogs enjoy leaping about and chasing bubbles, and, incredibly, Happy Dog Toys has developed edible bubble solutions that smell like savory bacon, peanut butter, or barbecued chicken. Wowee!
Well, the odoriferous bubbles are impressive, but the plastic “gun” that is supposed to produce them is not. Only a tiny reservoir is provided to contain the bubble solution, and within just a minute of pulling the trigger more or less constantly to manufacture enough bubbles for the dog to chase, I had to stop and refill it. Plus, the reservoir is not only too small, but also difficult to pour the bubble solution into without spilling. And, once it’s full, it’s hard to walk with the gun without tipping the solution out of the reservoir.
My advice is to buy the Bubble Buddy Replacement Bubbles (sold separately, $3 for two four-ounce bottles) and use an old-fashioned bubble wand – the little plastic circle you blow through. That is, at least until Happy Dog Toys redesigns the Bubble Buddy with a big, deep, spill-proof reservoir.
Happy Dog Toys is on the right track; if they keep improving the design of these innovative toys, and we’ll happily buy ‘em all, and recommend them to all our playful doggie friends, too.
Also With This Article
Click here to view “Super Durable Dog Balls for Fetching and Beyond”
Must-See Dog Book
Every month, I receive anywhere from a dozen to several dozen dog-related books, sent by publishers who are eager for a published review or just a casual editorial mention. My home office is pretty small, and already jam-packed with piles of press releases and boxes of products, but I do my best to find room on the already overflowing bookshelves. About once every couple of months, I weed through the stack, holding onto the most useful books and donating the rest to my local library.
Only rarely does a book arrive on my porch that immediately compels me to open it and read it right away; only once in six years of publishing WDJ have I received one that was so good that I couldn’t put it down until I had consumed the entire volume.
It shouldn’t be surprising to hear that the book that brought an abrupt halt to my work day is a product of National Geographic Books. Dog Stories is a 128-page softcover book featuring text and photographs by Richard Olsenius, an award-winning photographer, filmmaker, and former photo editor for National Geographic.
Dog books produced by outsiders journalists from the mainstream press often present a skewed look at our world. They tend to exaggerate the most eccentric aspects of our obsessions and overlook the serious, useful ways we benefit from our association with our dogs. However inaccurately portrayed we might appear, these books tend to look attractive and professional.
In contrast are the many book offerings from dog-world insiders. These publications, written or edited by dog breeders, trainers, judges, or veterinarians, are usually factually accurate, but sometimes lack graphic appeal or professional appearance.
Richard Olsenius does all the right things, and none of the wrong, in Dog Stories. Yes, he shows dog owners at our obsessive extremes, with pictures of dogs dressed in zany outfits, dogs enduring excesses of grooming in preparation for the show ring, and people who spend fortunes on medical marvels to extend their dog’s lives. However, these portraits are not made in fun or to mock us, but as a continuation of Olsenius exploration of the range and depth of the human/canine bond.
Olsenius also includes lush, gorgeous portraits of dogs who work sheep, assist disabled people, provide emotional support, sniff out drugs and bombs, and rescue disaster victims. Perhaps the most moving portrayals, however, are his written and photographic depictions of the relationships between ordinary people and their beloved canine companions. I promise; youll love this book.
-Nancy Kerns
Download the Full August 2003 Issue
Join Whole Dog Journal
Already a member?
Click Here to Sign In | Forgot your password? | Activate Web AccessHot Topics
All I can say about Training Editor Pat Millers article this month is that This stuff really works!
Like most dog owners over 15 years of age (younger owners have learned to train in a more enlightened time), I was taught to train dogs with a fair number of physical corrections and a certain amount of intimidation. Force-based training worked with all the dogs I ever lived with . . . except, of course, my parents tiny Yorkshire Terriers, who never learned a single desirable behavior, but they were dimwits. Punishment only made our Lab/Chesapeake-mix more aggressive, but he was pathologically angry, and had to be put down eventually. And it worked on Rupert, the 13-year-old Border Collie I still have today. Of course, hes sort of a soft dog, and still tends to freeze (and maybe even snap) when hes scared.
Im being sarcastic, of course. Before I was educated and exposed to positive training, I really thought I had done well with the dogs in my life. If the dogs didnt turn out, it was their fault, not how I handled them. Now I see how the force-based training methods I used failed again and again and again.
Today, I share my home with tiny Mokie, a young Chihuahua. Hes the first dog Ive ever trained completely without force or intimidation, and guess what? Hes turning out so great. Hes confident without being pushy. Hes friendly without being rude. Hes obedient in a cheerful and happy way. And best of all, when hes not sure what hes supposed to do, he sits down and fixes me with an intent stare, visibly willing me to tell him what to do.
Ill repeat: This stuff really works. Try it.
As a native Californian and lifelong dog owner, Ive probably spent thousands of dollars at various vet clinics, having foxtails removed from various canine orifices. Its taken me years to learn what author C.C. Holland passes along in her article on the noxious weeds in this issue.
My mom called me once at college, after her German Shepherd had been treated for an abscess (foxtail!) on his front paw. Our family vet gave my mother an Elizabethan collar and told her to put it on the dog if he started licking his paw, but she wasnt sure how it was supposed to go.
In her inimitably sweet and concerned tone, my mom asked, When I put the collar on him, is he supposed to look like a tulip or a prince? I laughed, considering both images. To this day, I can still see my mom in my minds eye, giggling as she dressed up her amiable Shepherd as a tulip, according to my instructions. Goodness knows what she would have made of all the alternatives to the traditional cones we review this month.
-Nancy Kerns
Why Force-Based Training Methods Are Not Advocated
By Pat Miller
Dominance has become something of a dirty word in many dog-training circles, and for good cause. Behaviorists once used the word to appropriately define a relationship between two individuals in a social group. However, over recent decades, the word has been warped and twisted to inappropriately describe an assertive dog’s personality.
Sadly, “dominance” has often been used as justification to inflict a litany of punishment on dogs, especially those dogs who react defensively to force-based training methods. In the past, if a dog responded to compulsion-based training or punishment by defending himself with a growl or snap, this was interpreted as dominance and defiance. In addition, many natural, normal dog behaviors, such as the desire to sleep on soft surfaces (beds and sofas), jumping up in greeting, and an eagerness to dash through doorways to get to the great outdoors, were also interpreted by some people as “dominant” behaviors that needed correcting.

According to these outdated theories, a dog’s owners should be the only dominant figures in the household, and they were exhorted to establish dominance over their dogs by being forceful. We were cautioned by our trainers and by the dog-training books of the day not to tolerate any of our dogs’ resistance – and warned that if we failed to fiercely squash any opposition, disaster would ensue. We were urged to leap to the offense if a dog objected to our rough handling, and told to apply violent techniques such as scruff shakes and alpha rolls if our dogs dared resist.
Some trainers went even further, advocating extremely abusive methods such as hanging a dog by the choke chain and leash, “helicoptering” him in the air at the end of a chain and leash, or holding his head in a hole filled with water until unconsciousness, for behaviors ranging from something as mild as digging to as serious as aggression.
We’re past that
Fortunately for dogs, modern behavioral science has moved past the simplistic notion that a dog owner’s absolute dominance will solve all (or any) of a dog’s behavior or training issues. This is especially true in cases involving a dog who “fights back” when physically hurt or frightened. Severe physical punishments may force a dog to comply, but this can cause the dog to fear the person meting out the punishment, or become violent in return.
Today’s positive trainers recognize the importance of the relationship between dogs and their owners, and realize that, while force-based methods can effectively train dogs, they also risk damaging the relationship between dog and owner, sometimes beyond repair.
Gentle, humane training methods are as effective as pain-based techniques (if not more so) and can accomplish the same training goals without force and the attendant risk of negative reactions such as fear and aggression that are possible whenever force is applied.
Learning to lead
A good leader doesn’t need to be violent – she simply needs to create an environment where it is easy and rewarding for her followers to comply with her wishes, and difficult for them to make mistakes. She helps them succeed. Attending a positive training class with your dog is a good place to start establishing yourself as a benevolent leader to your dog. A training class helps you and your dog understand each other better, and your trainer can help the two of you problem solve if the road gets bumpy along the way.
A successful leader/owner controls valuable resources, and shares them with her dogs generously and judiciously. Appropriate behaviors earn rewards. Inappropriate behaviors do not. If resources are consistently awarded on the basis of desirable behaviors, and withheld in the presence of undesirable behaviors, what dog in his right mind would not choose to be well-behaved? It’s no different than teaching a toddler that he has to say “Please” to get a cookie rather than scream “Gimme!” at the top of his lungs while his face turns blue.
Dominance myths
When the “you have to dominate your dog” concept was in vogue, many trainers instructed their clients to establish “dominance” (used incorrectly here) over their dogs. This was supposed to be accomplished by, among other things, eating before the dog eats, going through doorways before the dog, and routinely rolling the dog on his back in a show of force.
Fortunately, current and more in-depth behavior studies have shown that in wild and domesticated dogs, it’s not true that the pack leader always eats first, goes through doorways first, or routinely rolls other pack members onto their backs to keep them in line. She may be able to do all those things if she wants, but it really is in the pack’s best interest – and hers – to be in a state of equilibrium that doesn’t involve a constant show of force.
When there is plenty of food to go around, there is no need for the pack leader to assert herself at the feed trough. If she is eager to go through a door, she may choose to go first, in which case lower-ranking pack members defer to her.
And anyone who has ever watched dogs greeting and interacting quickly realizes that a “belly-up” posture on the part of a subordinate dog is usually voluntary. In fact, this voluntary submission posture normally triggers a response in the more assertive dog to call a truce. If one dog violently forces another onto his back and/or ignores the subordinate dog’s voluntary attempt at appeasement, the “underdog” is probably fighting for his life.
Similarly, the dog who is gets alpha-rolled by an owner may fear for his life and, terrified by his owner’s inexplicable violence, fight back accordingly.
Lower-ranking pack members show their deference to the leader with a number of body-language behaviors. Our Scottie, Dubhy, has learned the fine art of appeasing our very assertive Kelpie by keeping his eyes averted to avoid Katie’s intense Kelpie glare. As long as he avoids eye contact, she lets him pass without comment. He has, in essence, learned to say “please.”
Teaching your dog to “ask”
Your dog need not physically submit to you by offering his vulnerable underside – he only needs to defer. There are a number of quick and easy exercises you can insert painlessly into your daily routine to remind your dog that you are in charge of the resources, and he receives them thanks to your benevolence.
Say Please for Meals: It is perfectly okay to feed your dog before you eat your own meal – as long as you remind your dog that you control the food bowl. For starters, there should be no free-feeding. If your dog can pick from his dish whenever he wants, you allow him to believe that he controls the very valuable food-bowl resource, and you miss a golden opportunity to reinforce deference one or more times a day. (I feed my adult dogs twice a day.)
Each mealtime, after preparing your dog’s food, lift the bowl off the counter with his meal in it, and hold it at your chest. Wait for him to sit. If necessary, move the bowl over his head to lure the sit, or ask him to sit verbally. When he sits, tell him he’s a good boy and lower the bowl toward the floor. If he starts to get up, cheerfully say “Oops!” and lift the bowl to chest level again. Keep doing this until you can set the bowl on the floor without him moving. Then tell him “okay!” and encourage him to eat.
This is actually engaging in a little friendly food-guarding, a concept his canine brain should grasp easily. You are saying, “This food is really mine, because as leader all things belong to me, but because I’m nice I’m letting you have some of my food.”
Say Please to Go Outside: Anytime you are going to open a door to the outside world, ask your dog to “Wait!” (See “Wait a Bit, Stay a While,” WDJ, May 2001.) Open the door a crack, and if he starts to go through, say “Oops!” and gently close the door. Caution: do not slam the door on his nose! Then tell him “Wait!” and open the door a crack again. If he stays still, tell him he’s a good boy and close the door again. Gradually work up until you can open the door wide and he doesn’t go through unless you tell him he can.
Sometimes you will release him with an “okay” so he can run out the door into his fenced yard; sometimes you will go through the door and then invite him out; and sometimes you will go through and close it behind you, leaving him in the house.
You are telling him, “This is my door. I get to decide who goes through, and when. Sometimes you can go first, sometimes I go first, and sometimes you don’t get to go through at all.”
If you have more than one dog, vary the order in which you release them so that each goes first some of the time.
Say Please for Treats: Take advantage of every opportunity to instill “sit” as a default behavior – the thing the dog will do when he’s not sure what to do. Instead of popping a treat in his mouth just because he’s cute and you love him, wait for a sit – then pop the treat in his mouth. You are telling him, “These are my treats, and I will share them with you if I feel like it. You can make me feel like it by sitting.” A gratuitous treat is a missed opportunity to reinforce “sit” as his default behavior.
Say Please for Greeting: When your dog runs up to greet you, all excited because he hasn’t seen you for at least three full minutes, watch him closely. If he gathers himself to jump on you, say “Oops!” and turn your back. Watch him over your shoulder, and when he settles solidly on all fours, or even better, sits (because that has become his default behavior) say “Yes!” and turn back to greet him. If he jumps up, turn away again. Keep repeating until he will sit politely to be greeted.
You are telling him, “I am the leader, and as leader, my greeting is a valuable resource that I only give to dogs who are sitting.”
Say Please for Fun: Does your dog like to chase the ball? Play tug-o-war? Visit with his canine pals at the park? Go for a ride in the car? A walk on the leash? A swim in the pond? Precede all his favorite activities with a polite sit. “Sit” makes the ball go. “Sit” brings the tug toy to dog-mouth level. “Sit” gets the leash attached for a walk, or removed for a romp in the park. “Sit” elicits the release cue for a dive into the lake. “Sit” makes all good things happen.
If you want to take it a step further, “sit” makes the ball go, but the dog can only go when you give him an “Okay!” or “Go” release cue. Similarly, “sit” lowers the tug toy to mouth level, but he can only grab it when you say, “Take it!”
You are telling him, “I control all these wonderful resources – you can have access to them at my whim and pleasure, when I decide you can, and not before.”
Say Please for Attention: Rather than allowing your dog to demand your attention, make him ask by – you guessed it – sitting. If he is a big dog and you are sitting in a chair or on the sofa, a “down” is an even better “please” for attention.
You are telling him that this very valuable resource (your attention) must be earned with a sit or a down; he doesn’t get it on demand.
Kindly controlling
You should be getting the picture by now. The more assertive your dog’s personality, the more important it is that you control as many available resources as possible, and are consistent about paying them out for appropriate behavior. Whatever your dog’s personality, the better you are at controlling resources and awarding them for desirable behavior, the better behaved your dog is likely to be.
The benevolent leader concept comes naturally for some people. These are the folks who always seem to end up with well-mannered dogs without appearing to think much about it – it just happens. Either they were born with good “animal instincts,” or they had good human models to imitate from an early age. If it doesn’t come to you naturally, don’t despair, you can learn! Just start asking your dog to say “Please!” for everything you can think of.
-Pat Miller, WDJ’s Training Editor, is also a freelance author and Certified Pet Dog Trainer in Chattanooga, Tennessee. She is the president of the Board of Directors of the Association of Pet Dog Trainers, and published her first book, The Power of Positive Dog Training, in 2001.
Commercially Produced Recreational Chew Bones
By C.C. Holland
With the third twist of the vise handle, the bone held snugly inside splintered along its length with a sickening crunch. Splinters and fragments sprouted from the crack like thistle.
The scene of a gruesome torture chamber? Hardly. Rather, this was a common result during informal testing conducted by WDJ in an attempt to ascertain whether certain types of “recreational” bones pose more hazards than others to the dogs who chew them.

First, some background. Our plan was to create a companion piece to an article about rawhide chews that ran in our May 2002 issue. We decided to take a look at the wide variety of commercially prepared bones available to dog owners in pet supply stores and catalogs. We hoped to learn whether these bones originated from U.S. livestock (which tends to be better safeguarded and regulated than animal products from some foreign sources) and what sorts of chemicals – if any – were commonly used in the preparation or preservation of the products. On both these counts, we heard good news.
Production methods
All the manufacturers whose representatives were willing to be interviewed told us that their companies obtain raw products from American slaughterhouses, and some (such as Abbyland Foods) get bones from their own slaughtering plants. Bones either were received frozen and thawed for processing or were processed fresh.
Production techniques were similar among the four companies whose representatives we interviewed, including Merrick Pet Foods in Texas; Redbarn in California; Abbyland Foods in Wisconsin; MI Industries (Nature’s Variety) in Nebraska; and Jones Natural Chews in Illinois. (Gimborn Pet Specialties in Atlanta, which sells bones through the Petsmart chain, declined our requests for an interview.) In all cases, creating the final product pretty much consists of simply cleaning and drying the bones in industrial ovens.
Some companies go the extra mile to ensure a quality product. Nature’s Variety – the only one of these companies that also sells frozen raw bones – prides itself on strict adherence to food-safety guidelines.
“We work in very close cooperation with the University of Nebraska food processing center,” says company president Bob Milligan. “They help us with processing techniques, selecting oven temperatures, testing for bacteria, and upgrading sanitation methods, things like that.”
Creating the cooked bones is a no-frills process. “We slow-roast them and then dry them down to a moisture content of approximately 10 to 12 percent,” says Milligan. “That allows them to be shelf-stable without having to add any preservatives, chemicals, or artificial colors. Our opinion, and that of our nutritionists and vets we work with, is that the product doesn’t need to have a smoked flavor to be appealing to the dog. And many times smoking is used to cover up an ‘off’ odor or condition.”
Other companies choose to add flavoring to the bones, either for marketing appeal or, in some cases, to prevent mold.
“We dip them in a solution of liquid smoke, for smell, and a marinate solution that helps inhibit mold growth,” says Jane Langman of Abbyland, which sells bones through Drs. Foster & Smith. “It’s an all-natural product – there are no preservatives.”
Most of these recreational bone manufacturers say preservatives are not necessary for bone products.
“Typically, with products under 10 percent moisture, there’s no need for preservatives,” explains Garth Merrick, president of Merrick Pet Foods. “Lack of moisture means a lack of protein to degenerate to the point where you get bacteria.”
But that doesn’t mean every finished product is immune. All it takes is the right conditions – such as damaged wrapping and humid weather. We’ve seen shrink-wrapped meaty bones (not produced by any of the companies listed here) laced with mold on the shelves of a local Trader Joe’s grocery store. Once moisture content rises inside the packaging, green fuzz can sprout.
“Also, where there’s enough moisture for mold to grow, you can have elevated bacteria levels,” adds Milligan. “You can have concerns about salmonella and E.coli.”
These issues are more likely to affect consumers and their food-handling practices, since healthy, adult dogs are usually unaffected by bugs that would lay humans low. Hand-washing is always recommended after touching a dog’s chew bones.
Well-dried bones in a dry environment can last a very long time on a shelf or in your pantry, which explains part of their appeal. Some owners trade weekly trips to the butcher shop for a box of dried bones. Others don’t have access to butcher shops, but can get dried or cooked bones from local pet stores.
Laura Herr of Jones Natural Chews said her company labels its products with sell-by dates, but it’s more to give the distributor, retailer, or consumer a benchmark than to warn against spoilage. “They have a very long shelf life,” she says. “We put our (sell-by dates) two years out. But we’ve had some bones in our testing area for eight years, and they still look beautiful.”
Additives?
By reducing the moisture content of their products, most of these companies are able to forego the use of preservatives to keep the animal-based products from decomposing. An exception is Redbarn, which uses preservatives in its “stuffed” bones, which have artificially flavored and colored filling. The stuffing is either cheese-and-bacon, chicken, beef, or lamb flavored.

Jeff Baikie, co-president of Redbarn, defends the filling, which is mostly meat by-products with meat or poultry meal and lots of sugars, salt, and other flavor enhancers, on the basis that it’s meant as an occasional treat. “I’m not saying you’d want to feed this as a full diet, but two ounces once a week isn’t a big deal,” Baikie says.
Stuffing a bone creates added value for the consumer, Baikie told us, because a dog will remain interested in it much longer. And the processing of the bones Redbarn uses – stuffed or not – is minimal, he says; they are simply cleaned and dried.
At WDJ, we’re not wild about these filled bones. For one thing, with so many all-natural, unpreserved, and uncolored treats available today, we think owners can afford to be choosier about their dogs’ treats. Filling aside, we’re even more concerned about the bones themselves.
Dental dangers
There are two main knocks on dogs chewing bones: dental and gastrointestinal concerns.
Frank J.M. Verstraete, DVM, a diplomate of the American Veterinary Dental College and a professor of dentistry and oral surgery at the University of California, Davis School of Veterinary Medicine, agreed to evaluate a variety of cooked treat bones with regard to dental health. We brought him a bag full of commercial recreational chew bones to examine – roasted, smoked, dried, meat-on, hollow, stuffed, and so on. From his perspective, he says, none are safe for canine consumption.
“Basically, the main rule that we use is that you should be able to make an impression in the item with your thumbnail,” he says. “If you cannot, it’s too hard.” All the bones in our bag flunked his test.
Dr. Verstraete explains that hard, dried bones present an opportunity for dogs to crack premolars while gnawing. (There are four premolars on each side of the upper and lower jaws, directly behind the canine teeth.) Fresh, raw bones are preferable, but once they dry out they also pose a problem. In fact, on the day we interviewed him, he’d treated two dogs – both described by their owners as non-aggressive chewers – who had broken teeth on desiccated raw bones.
Nature’s Variety uses a slow-roasting process they say makes the cooked bone less brittle and hard. According to company president Bob Milligan, the final products have a moisture content of about 10 to 12 percent. “It probably is softer and contains more moisture at the time of manufacturing,” allowed Dr. Verstraete when he looked over some Nature’s Variety bones. “But once this has been on a shelf for a while, it’s too dry.”
Whether certain types of bones – say, ribs or bones from younger animals – tend to be safer is an open question. Dr. Verstraete says all evidence either way is purely anecdotal. But the extra-hard bones sometimes designated as appropriate for “aggressive chewers”? Steer clear. “Much too hard,” he says. “Good for a hyena, but not for a dog.”
While he is very critical of cooked and dried bones, Dr. Verstraete doesn’t go so far as to proscribe bones entirely, especially if a dog has been brought up on bones and uses them regularly for recreational chewing.
“As long as it’s a fresh bone, and an appropriate size and shape for the dog,” he says, letting your dog chew is fine. Dr. Verstraete recommends condyles (the lumpy knobs at the end of bones) over the tubular, middle portions of leg bones, because they are softer. Those leg bones are cortical bones, which have a high resistance to bending and torsion.
Cathy Dyer, DVM, a colleague of Dr. Verstraete’s at UC Davis, says the size of the bone is also very important. “For those people who really want to give their dog a bone – because let’s face it, it does really clean the teeth – I’ve always said give a great big bone, like a beef knuckle bone,” she says. The idea is to provide a bone that’s too large for a dog to get between his jaws and bear down, which could lead to tooth damage.
Splinters
In addition to posing dental dangers, bones can also do something else: splinter. The reality is that virtually any bone, cooked or not, can splinter or break in the right circumstances. However, the manufacturers we spoke with said complaints about splintering were virtually nil.
Bob Milligan of Nature’s Variety says the secret to safer bones lies in the selection. “We try to select bones like the ham bone, which is the main femur bone of the pig,” he explains. “That is a medium hardness bone, either in the raw or roasted state. We found that the slow roasting helps soften that bone so splintering has not been a problem. We sell literally hundreds of thousands of those bones and have not had problems. I should add we always caution the pet caregiver to supervise the pet with bones, whether the bones are raw or slow-roasted.”
Jeff Baikie of Redbarn says his company has fielded “a few” complaints. “Any manufacturer who tells you different is probably lying,” he says. “But it’s very, very limited. What you’re worried about is splintering, and splinters getting lodged in the dog’s throat or intestines. But for the number of bones we sell, we might get three complaints a year, and we’re talking million and millions of bones.”
Then again, some said they were aware of problems with certain types of bones. “We have had requests from some customers to make a sterilized bone; they want it boiled, free of meat,” says Milligan, adding that Nature’s Variety does not make such a bone. “The problem we had, and why we did not pursue it, is the bones became very brittle, almost like glass. You could literally drop them and they would break or crack.”
Breaking bones
That was certainly our own experience in our informal test lab – the backyard of the editorial office of WDJ. Just for kicks, we decided to subject a wide range of commercial bones and some plain old “butcher bones” to some admittedly unscientific tests, to compare how the different products responded to various physical pressures. We included raw frozen bones, raw thawed bones, and a number of commercially prepared bones, including those with attached meat and tissues, sterilized bones, slow-roasted bones, joints, long bones, and even rib bones. Some of these commercial products were from the companies whose representatives we interviewed, while others were either not labeled or were competing brands.
While we did not attempt to exactly simulate the forces applied by a dog’s teeth and jaws, we did subject each of them to a couple of light taps with a hammer, as well as a brief session of squeezing in a large iron vise. What we found was disheartening.
Every bone yielded to our tests – some even shattered like porcelain, leaving behind razor-sharp shards, and others resisted several whacks and/or turns of the vise before cracking. The raw bones were marginally softer, as was a ham bone from Nature’s Variety; these cracked and flaked apart. Still, they yielded small pieces. If ingested, what havoc could these splinters wreak on a dog’s mouth, throat, or stomach?
In the vise test, we wanted to approximate the pressure caused by a dog’s jaws closing down on a bone. Once again our test bones gave way – although the Nature’s Variety dry-roasted ham bone (which included condyles) did best, changing shape but not splitting or breaking.
When the bones cracked in the vise, they splintered. Some, like Smokehouse’s roasted rib bone, lost small, crumbly chunks; others, like Redbarn’s plain white bone, split up their length and fell apart. Even the moist raw bones split off sharp shards.
At the end of our experiment, sitting amid the rubble of broken bones and needle-sharp shards, we had some decisions to make.
We decided that it would be courting danger to recommend giving any cooked treat bones to a dog with large, strong jaws and an aggressive chewing style. Any of the offerings could be reduced to a pile of potentially harmful pieces or could cause a broken tooth.
For moderate chewers or small dogs, we could see giving them an extra-large bone – one that they couldn’t fit between their back teeth – and keeping a watchful eye on their activity.
Garth Merrick responded to our concerns by acknowledging that dangers do exist.
“There’s no question, if you break one it’s going to have some sharp edges,” he says. “If the customer will use common sense, I really think the amount of risk is minimized.”
Proper sizing, he says, is most crucial.
“If the people who buy the bones will size the bone to the size of the dog’s jaws and keep it big enough so they cannot fit it in and bear down with their back teeth, they cannot put enough pressure on it to break it,” he says. “Even though there is a risk, there are millions of satisfied people whose dogs have never had a problem.”
Laura Herr of Jones Natural Chews agreed that owner supervision and sizing were important, but also took it a step further, noting that certain types of bones are less prone to problems.
“There are several bones that do not splinter,” she says. “If you put a shank bone or a knee cap from the knee joint to your test, neither of these bones will splinter even for the most aggressive chewer. Any knuckle bone does not present danger of splinters. The bones that do splinter for the aggressive chewer are the straight bones, which we call center bones.”
Should you avoid bones entirely? There’s no easy answer, and it’s an individual decision. Some dogs will do fine on just about any sort of bone, while others will make mincemeat of even bones that are considered very safe.
After collecting chips, shards, and sharp fragments of bone from our testing grounds, we can’t help but think that sometimes it’s better not to give your dog that bone.
Also With This Article
Click here to view “Choosing The Right Dog Chew For Your Dog”
Click here to view “Feeding Bones or Raw Foods to Puppies”
-C.C. Holland is a freelance writer from Oakland, California.