BLOAT IN DOGS: OVERVIEW
1. If your dog is a breed at high risk for bloating, discuss with your vet the merits of a prophylactic gastropexy at the time of neutering.
2. Familiarize yourself and your dog with the emergency veterinary services in your area, or anywhere you’ll be traveling with your dog. You never know when you’ll need to rush your bloating dog to the animal hospital.
3. Feed your dog several smaller meals daily rather than one or two bigger meals to reduce your dog’s risk of gastric dilatation.
4. Consider feeding your dog a home-prepared diet; while there have not been studies that support the assertion, many dog owners who make their dogs’ food swear that it prevents GDV.
Imagine seeing your dog exhibit some strange symptoms, rushing him to the vet within minutes, only to have the vet proclaim his case to be hopeless and recommend euthanasia. For too many pet parents, that’s the story of dog bloat, an acute medical condition characterized by a rapid accumulation of gas in the stomach.
In fact, that was exactly the case with Remo, a Great Dane owned by Sharon Hansen of Tucson, Arizona. “He was at the vet’s in under seven minutes,” says Hansen, in describing how quickly she was able to respond to Remo’s symptoms. He had just arisen from an unremarkable, hour-long nap, so Hansen was stunned to see Remo displaying some of the classic symptoms of dog bloat, including restlessness, distended belly, and unproductive vomiting.
Despite Hansen’s quick action, Remo’s situation rapidly became critical. Radiographs showed that his stomach had twisted 180 degrees. Remo was in great pain and the vet felt the damage was irreversible. Hansen made the difficult decision to have Remo euthanized at that time.
Canine bloat, or more technically, gastric dilatation and volvulus (GDV), is a top killer of dogs, especially of deep-chested giant and large breeds, such as Great Danes and Standard Poodles. A study published in Veterinary Surgery in 1996 estimated that 40,000 to 60,000 dogs in the United States are affected with GDV each year with a mortality rate of up to 33 percent.
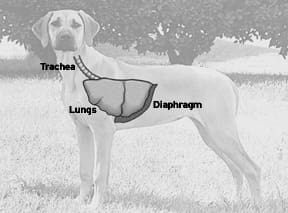
Gas accumulation alone is known as dog bloat, or dilatation. The accumulation of gas sometimes causes the stomach to rotate or twist on its axis; this is referred to as torsion or volvulus. Bloat can occur on its own, or as a precursor to torsion. In this article, to simplify the terms, bloat and GDV are used interchangeably.
Both conditions can be life-threatening, although it often takes longer for a straightforward gastric dilatation without volvulus to become critical. “Bloats without torsion can last for minutes to hours, even days in low-level chronic situations, without it becoming life-threatening. But with torsion, the dog can progress to shock rapidly, even within minutes,” explains Alicia Faggella DVM, DACVECC, a board-certified specialist in veterinary emergency and critical care.
“A dog can go into shock from bloat because the stomach expands, putting pressure on several large arteries and veins. Blood does not get through the body as quickly as it should,” continues Dr. Faggella. In addition, the blood supply gets cut off to the stomach, which can cause tissue to die, while toxic products build up.
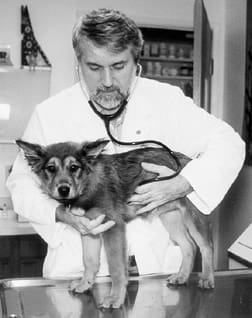
While some less acute cases of dog bloat may resolve themselves, it often takes an experienced veterinarian to know just how serious the problem may be, and whether surgical intervention is required to save the dog’s life.
Symptoms of Bloat in Dogs
– Unproductive vomiting
– Apparent distress
– Distended abdomen, which may or may not be visible
– Restlessness
– Excessive salivation/drooling
– Panting
– The dog’s stomach is hard or feels taut to the touch, like a drum
– Pacing
– Repeated turning to look at flank/abdomen
– Owner feels like something just isn’t right!
Dog Bloat is Frighteningly Deadly
Various studies have estimated the mortality rate for dogs who have experienced an episode of GDV, and while the results varied, they were all frighteningly high – from about 18 percent to more than 30 percent. The rates used to be much higher, however.
“Veterinarians over the past two decades have reduced dramatically the postoperative fatality rate from gastric dilatation-volvulus from more than 50 percent to less than 20 percent by using improved therapy for shock, safer anesthetic agents, and better surgical techniques,” says Lawrence Glickman, VMD, DrPH, and lead researcher on a number of studies related to GDV at Purdue University in West Lafayette, Indiana.
In many acute cases of GDV, surgery is the only option to save the life of the animal. In addition to repositioning the stomach, it may also be “tacked” to the abdominal wall in a procedure called gastropexy. While dogs who have had gastropexy may experience gastric dilatation again, it is impossible for the stomach to rotate, as in volvulus or torsion.
What Causes Bloat in Dogs?
Theories about the causes of bloat in dogs abound, including issues related to anatomy, environment, and care. Research from Purdue University, particularly over the past 10 years, has shown that there are certain factors and practices that appear to increase the risk of GDV, some of which fly in the face of conventional wisdom.
“We don’t know exactly why GDV happens,” says Dr. Faggella. Some people do all of the “wrong” things, and their dogs don’t experience it, she says, while some do all of what we think are the “right” things, and their dogs do.
The most widely recognized and accepted risk factor is anatomical – being a larger, deep-chested dog. When viewed from the side, these dogs have chest cavities that are significantly longer from spine to sternum, when compared to the width of the chest cavity viewed from the front.
This body shape may increase the risk of bloat because of a change in the relationship between the esophagus and the stomach. “In dogs with deeper abdomens, the stretching of the gastric ligaments over time may allow the stomach to descend relative to the esophagus, thus increasing the gastroesophageal angle, and this may promote bloat,” says Dr. Glickman.
Can Small Dogs Get Bloat?
It isn’t just large- and giant-breed dogs that can bloat; smaller breeds do as well. “I’ve seen Dachshunds, Yorkies, and other small Terrier breeds with bloat,” says Dr. Faggella. She emphasizes that all dog guardians should be familiar with the signs of bloat, and be ready to rush their dog to the vet if any of the symptoms are present.
Likelihood of an incident of dog bloat seems to increase with age. Purdue reports that there is a 20 percent increase in risk for each year increase in age. This may be related to increased weakness, over time, in the ligaments holding the stomach in place, Dr. Glickman explains.
Another key risk factor is having a close relative that has experienced GDV. According to one of the Purdue studies that focused on nondietary risk factors for GDV, there is a 63 percent increase in risk associated with having a first degree relative (sibling, parent, or offspring) who experienced bloat.
Personality and stress also seem to play a role. Dr. Glickman’s research found that risk of GDV was increased by 257 percent in fearful dogs versus nonfearful dogs. Dogs described as having a happy personality bloated less frequently than other dogs. “These findings seem to be consistent from study to study,” adds Dr. Glickman.
Dogs who eat rapidly and are given just one large meal per day have an increased susceptibility to GDV than other dogs. The Purdue research found that “for both large- and giant-breed dogs, the risk of GDV was highest for dogs fed a larger volume of food once daily.”
The ingredients of a dog’s diet also appear to factor into susceptibility to bloat. A Purdue study examined the diets of over 300 dogs, 106 of whom had bloated. This study found that dogs fed a dry food that included a fat source in the first four ingredients were 170 percent more likely to bloat than dogs who were fed food without fat in the first four ingredients. In addition, the risk of GDV increased 320 percent in dogs fed dry foods that contained citric acid and were moistened before feeding. On the other hand, a rendered meat meal that included bone among the first four ingredients lowered risk by 53 percent.
Another study by Purdue found that adding “table foods in the diet of large- and giant-breed dogs was associated with a 59 percent decreased risk of GDV, while inclusion of canned foods was associated with a 28 percent decreased risk.” The relationship between feeding a home-prepared diet, either cooked or raw, hasn’t been formally researched.
Anecdotally, however, many holistic vets believe that a home-prepared diet significantly reduces the risk of bloat. “I haven’t seen bloat in more than five years,” says Monique Maniet, DVM, of Veterinary Holistic Care in Bethesda, Maryland. She estimates that 75 to 80 percent of her clients feed a raw or home-cooked diet to their dogs.
Dr. Faggella also noticed a difference in the occurrence of bloat while in Australia, helping a university set up a veterinary critical care program. “I didn’t see bloat as commonly there [as compared to the US],” she says. They feed differently there, with fewer prepared diets and more raw meat and bones, which may contribute to the lower incidence of GDV, she adds.
It is often recommended that limiting exercise and water before and after eating will decrease the risk of bloat. However, in one of the Purdue studies, while exercise or excessive water consumption around meal time initially seemed to affect likelihood of GDV, when other factors were taken into account, such as having a close relative with a history of GDV, in a “multivariate model,” these factors were no longer associated with an increased risk of bloat.
Or, more simply put, “there seems to be no advantage to restricting water intake or exercise before or after eating,” says Dr. Glickman.
How to Prevent Bloating in Dogs
Because the theories and research on what causes bloat aren’t always in agreement, the ways to prevent GDV can conflict as well. One thing that everyone can agree on, though, is that feeding smaller meals several times a day is the best option for reducing the risk.
One of the top recommendations to reduce the occurrence of GDV from the Purdue researchers is to not breed a dog that has a first-degree relative that has bloated. Results of their study suggest that “the incidence of GDV could be reduced by approximately 60 percent, and there may be 14 percent fewer cases in the population, if such advice were followed.”
In addition, Glickman says they recommend prophylactic gastropexy for dogs “at a very high risk, such as Great Danes. Also, we do not recommend that dogs have this surgery unless they have been neutered or will be neutered at the same time.”
The concern about performing a gastropexy on an unneutered dog is that it “might mask expression of a disease with a genetic component in a dog that might be bred.”
While gastropexy hasn’t been evaluated in its ability to prevent GDV from happening the first time, research has shown that just five percent of dogs whose stomachs are tacked as a result of an episode of GDV will experience a repeat occurrence, whereas up to 80 percent of dogs whose stomachs are simply repositioned experience a reoccurrence.
Raised Bowls Raise the Risk of Bloating
It has long been an accepted practice to elevate the food bowls of giant-breed and taller large-breed dogs. The theory is that, in addition to comfort, a raised food bowl will prevent the dog from gulping extra air while eating, which in turn should reduce the likelihood of bloat. However, this recommendation has never been evaluated formally.
It was included in the large variety of factors followed in a Purdue study,* and one of the most controversial findings. The research suggests that feeding from an elevated bowl seems to actually increase the risk of GDV.
The researchers created a “multivariate model” that took into account a number of factors, such as whether there was a history of GDV in a first-degree relative, and whether the dog was fed from an elevated bowl. Of the incidences of GDV that occurred during the study, about 20 percent in large-breed dogs and 52 percent in giant-breed dogs were attributed to having a raised food bowl.
The raw data, which doesn’t take into account any of the additional factors, shows that more than 68 percent of the 58 large-breed dogs that bloated during the study were fed from raised bowls. More than 66 percent of the 51 giant-breed dogs that bloated during the study were fed from raised bowls.
* These findings were reported in “Non-dietary risk factors for gastric dilatation-volvulus in large- and giant-breed dogs,” an article published November 15, 2000, in Volume 217, No. 10 of Journal of the American Veterinary Medical Association. The study followed more than 1,600 dogs from specific breeds for a number of years, gathering information on medical history, genetic background, personality, and diet.
Phazyme: The Controversial Gas-Reliever
After Remo’s death, Sharon Hansen learned that some large-breed dog owners swear by an anti-gas product called Phazyme for emergency use when bloat is suspected. Phazyme is the brand name of gelcaps containing simethicone, an over-the-counter anti-gas remedy for people. GlaxoSmith-Kline, maker of Phazyme, describes it as a defoaming agent that reduces the surface tension of gas bubbles, allowing the gas to be eliminated more easily by the body.
Less than a year and a half later, Hansen had an opportunity to try the product when her new rescue dog Bella, a Dane/Mastiff mix, bloated. “Bella came looking for me one afternoon, panting and obviously in distress,” explains Hansen, who immediately recognized the signs of bloat.
Hansen was prepared with caplets of Phazyme on hand. “I was giving her the caplets as we headed out to the car,” says Hansen. Almost immediately, Bella began to pass gas on the short ride to the vet. “She started passing gas from both ends,” Hansen says. By the time they arrived at the vet, Bella was acting much more comfortable, and seemed significantly less distressed.
At the vet’s office, gastric dilatation was confirmed, and luckily, there was no evidence of torsion. Hansen credits the Phazyme for reducing the seriousness of Bella’s episode. This is a generally accepted practice among guardians of bloat-prone dogs, but not all experts agree with it.
Dr. Faggella cautions against giving anything by mouth, as it could cause vomiting, which could lead to aspiration. “If you suspect bloat, simply bring your dog to the vet immediately. The earlier we catch it, the better,” she says.
Dr. Nancy Curran, DVM, a holistic vet in Portland, Oregon, agrees that trying to administer anything orally could lead to greater problems. However, she suggests that Rescue Remedy, a combination of flower essences that is absorbed through the mucous membranes of the mouth, may help ease the shock and trauma. “Rescue Remedy helps defuse the situation for everyone involved. It won’t cure anything, but it can be helpful on the way to the vet,” she says, recommending that the guardian take some as well as dosing the dog.
Holistic Prevention of Dog Bloat
“We may be able to recognize an imbalance from a Chinese medical perspective,” says Dr. Curran. She’s found that typically dogs prone to bloat have a liver/stomach disharmony. Depending on the dog’s situation, she may prescribe a Chinese herbal formula, use acupuncture, and/or suggest dietary changes and supplements to correct the underlying imbalance, thereby possibly preventing an episode in the first place.
Dr. Maniet also looks to balance a dog’s system early on as the best form of prevention. Each of her patients is evaluated individually and treated accordingly, most often with Chinese herbs or homeopathic remedies.
Both holistic vets also recommend the use of digestive enzymes and probiotics, particularly for breeds susceptible to canine bloat, or with existing digestive issues. “Probiotics and digestive enzymes can reduce gas, so I’d expect that they will also help reduce bloat,” explains Dr. Maniet.
Another avenue to consider is helping your fearful or easily stressed dog cope better in stressful situations. While no formal research has been conducted to confirm that this in fact would reduce the risk of bloat, given the statistics that indicate how much more at risk of GDV fearful dogs are, it certainly couldn’t hurt. Things to consider include positive training, desensitization, Tellington TTouch Method, calming herbs, aromatherapy, or flower essences.
While there is an abundance of information on how to prevent and treat bloat, much of it is conflicting. The best you can do is to familiarize yourself with the symptoms of GDV and know your emergency care options. While it may be difficult to prevent completely, one thing is clear. The quicker a bloating dog gets professional treatment the better.
Case History: Laparoscopically Assisted Gastropexy
On May 6, 2004, Dusty, a nine-year-old Doberman, was in obvious distress. “He was panting, pacing, and wanting to be near me,” his guardian, Pat Mangelsdorf explains. Dusty didn’t have any signs of tenderness or injury, and his appetite and elimination were fine. Mangelsdorf wasn’t sure what the problem could be. After a few hours, his behavior didn’t improve, so she took Dusty to the vet.
“By that time, he had calmed a bit, and there still wasn’t any tenderness or distension. Radiographs showed some arthritis in his spine, so we thought that was causing him pain,” she says. A few hours later, Dusty lay down to rest and seemed normal.
Three days later, Mangelsdorf received a surprise call. “A radiologist had reviewed the X-rays and noticed that Dusty had a partial torsion,” she says. The vet suggested that to help prevent another incident of torsion, Dusty’s activity level, food, and water should be more tightly controlled, and a gastropexy should be considered to rule out future occurrences.
Mangelsdorf began researching her options. Was the surgery necessary? If so, which would be best, the full abdominal surgery or the laparoscopic procedure? Before she could decide, Dusty had another apparent torsion episode. “He had exactly the same symptoms,” says Mangelsdorf. Dusty spent a night at the emergency clinic, and more radiographs were taken, but they were inconclusive. Nevertheless, Mangelsdorf had made up her mind.
After reviewing the options and the potential risks and rewards, Mangelsdorf opted for a laparoscopically assisted gastropexy, rather than a traditional gastropexy with a full abdominal incision. “A laparoscopic gastropexy is minimally invasive, with just two small incisions,” explains Dusty’s surgeon, Dr. Timothy McCarthy, of Surgical Specialty Clinic for Animals in Beaverton, Oregon. Dr. McCarthy, who specializes in minimally invasive surgeries and endoscopic diagnostic procedures, has been performing this type of gastropexy for about four years.
This specialized procedure for gastropexy was developed by Dr. Clarence Rawlings, a surgeon and professor of small animal medicine at University of Georgia. The technique involves two small incisions. The first incision is to insert the scope for visualizing the procedure, the second incision is used to access the stomach for suturing. After palpating the stomach, it is pulled up toward the abdominal wall, near the second incision. The stomach is then sutured directly to the abdominal wall, as in a standard gastropexy. The incisions are then closed as normal, usually with staples.
“This is a very quick procedure. An experienced surgeon can do it in 15 minutes,” says McCarthy. While quick, the surgery isn’t inexpensive. It costs about $1,500 at McCarthy’s clinic.
On July 27, Dusty underwent surgery. The procedure went well, without any complications. Later that evening, Dusty started heavy panting and shivering, but X-rays and bloodwork showed everything normal. With IV fluids, he was more settled in a few hours, and back to normal by morning.
“Afterwards, we did short walks, no stairs, and three or four small meals a day for two weeks,” says Mangelsdorf. Gradually, she increased Dusty’s exercise until he was back to normal levels. She added acidophilus as well as more moisture into his diet, including cottage cheese and canned food, while keeping his water bowl at lower levels so he doesn’t drink excessive amounts at any one time.
Shannon Wilkinson, of Portland, Oregon, is a freelance writer, life coach, and TTouch practitioner.