Download the Full June 2005 Issue PDF
Preparing Your Dog For a Newborn Baby
Children have never been a consideration for me, and since neither my husband nor I have children of our own, I’m also not likely to have grandbabies visiting. So why should I care whether my dogs are good with children or not?
Because children exist.

Wherever you go in today’s world, there are likely to be young humans. Unless you plan to keep your dog cloistered in your own home, shut away when friends with children visit, you need to help her be comfortable with children. Your dog’s very life could depend on it.
At one time, our culture was far more tolerant of dog bites than it is today. When I was a kid, if a dog bit a child, Mom’s response was, “So, what did you do to Nipper to make him bite you?” Children were expected to learn how to respect a dog’s space, and if Johnnie acquired a few nicks from a dog’s teeth in the process, so be it. Today, one bite, even a minor nip, can be a death sentence for a dog. Of course, in the “old” days, Mom and Dad didn’t risk losing their homeowner’s insurance over a minor dog bite or two, either.
According to statistics from the Centers for Disease Control in Atlanta, Georgia, children are the most frequent victims of dog bites in this country. That’s no accident. From a dog’s perspective, babies and children are weird, unpredictable, noisy, move erratically, make long, hard, direct eye contact, often cause pain, and don’t respond appropriately to a dog’s appeasement, deference, or self-defense signals.
Since most children aren’t allowed to learn by experience that when a dog stiffens, growls, and curls his lip, the next thing that usually happens is a snap or bite, kids tend to be oblivious to the various levels and intensities of a dog’s warning signals. No wonder dogs perceive children as threatening!
Veterinary behaviorist Dr. Ian Dunbar, of Berkeley, California, tells audiences at every opportunity that the best insurance against future dog bites to humans, young and old, is puppy socialization. If it’s too late for puppy socialization, it’s not too late to start playing catch-up with remedial socialization. If you already have a baby, are planning to have one soon, have distant plans for children or, like me, don’t ever intend to have human puppies, now’s the time to start your personal kid-bite insurance program.
Socializing Puppies to Babies and Kids
Many young couples acquire a puppy early in the relationship, long before the advent of the first baby. The puppy is a surrogate child, and the couple dotes on him – taking him everywhere, allowing him to sleep on the furniture, even share the marriage bed. For several years the dog enjoys his status as an only child. The couple tends to socialize with other childless adults, and the dog rarely sees human babies. Then the couple decides it is time to have a baby. Now they have a problem.
Puppies go through a critical learning period in the first few months of their lives. During this time, usually between the ages of four weeks and four months, they learn which things in the world are safe and rewarding, which ones are painful and dangerous and should be avoided, and which have no consequence. Anything not experienced during this critical period tends to automatically fall into the “dangerous” category.
This is an important survival tool for wild animals; if they don’t know for sure that something is harmless, it’s safest for them to behave as though it’s not. Herein lies the problem. If a puppy doesn’t learn that children are “safe and rewarding” during those critical months, he’s likely to assume that they are a threat.
This assumption is often supported by the behavior of many of the children that a dog meets. Human puppies poke fingers into canine ears, prod them with pencils, hit them over the head with wooden blocks, and pull fur in sensitive places. They stare directly into a dog’s eyes (a direct stare is a threat in the canine world). They compete for food, toys, and the attention of grownups. They move erratically – running, tripping, falling, swinging their arms around – and make weird noises. If you stop and think about it, it’s a miracle that dogs tolerate kids at all!
In a perfect world, every new puppy would be thoroughly socialized to babies, toddlers, and children while she was in her critical learning period. Unfortunately, many vets recommend that their clients wrap their puppies in cotton wool and keep them strictly at home until they have been fully vaccinated – which won’t occur until weeks after the critical learning period.
It’s vitally important that your puppy have positive experiences with the big wide world during her first four months, long before she’s fully vaccinated. The good news is that you can do this without going against your vet’s recommendation or exposing your puppy to life-threatening diseases. Here’s how:
Invite lots of people – including babies and children, vaccinated healthy puppies, and vaccinated, healthy, friendly dogs – over to your house for puppy parties. Give everyone handfuls of really yummy treats to feed to the puppy. (Tell everyone the puppy has to sit to get her treats and you’ll also be teaching her not to jump up on people at the same time.) Monitor your pup’s interactions with children to be sure they are all positive. Have children of all ages feed your puppy lots of treats and she’ll quickly decide that kids are a good thing, not dangerous.
You can also take your puppy out into the community to safe, canine-friendly locations. Don’t go to busy dog parks and turn her loose to play, but do take her with you to places such as a well-run puppy kindergarten class, where you can monitor her inter-actions with kids and prevent her exposure to potential disease threats. Teach her that the world, especially the small humans of the world, are a source of pleasure and reward, and you greatly reduce the risk of “Dog Mauls Toddler” headlines in your dog’s future.
Adult Dog/Kid Conditioning
Maybe it’s too late to socialize your dog to babies and children during her critical learning period. That stage of her life has long passed. Is it too late to teach her to live with children? Not necessarily. It’s more difficult, but not impossible.
If your dog’s experiences with children up until now have been neutral and she’s otherwise well-socialized, seek out gentle children and have them feed her treats. Watch her closely. If she seems cheerful and happy, continue to find opportunities for her to have positive experiences with kids.
If your dog is tense or nervous with children, take it more slowly. Let her see babies and kids at a distance, and you feed her treats. Select a very special treat, like steak or chicken, and feed it to her only in the presence of children and babies. When she notices a child in the distance, steak starts raining from the heavens – tiny tidbits, nonstop. When the child leaves, the flood of steak stops. Every time a child appears, the steak starts. When the child leaves, the steak stops. You want your dog to think that children and babies, and only children and babies, make steak happen.
When your dog looks at you happily for her steak when she sees a child in the distance, you know she’s starting to perceive children as reliable predictors of steak. Your goal is to convince her to like them close up as well, through the continued association with really wonderful food.

Gradually move closer to the children, repeating the exercise, always watching your dog’s body language to be sure she’s comfortable.
This is critical: Never punish your dog for showing signs of discomfort or even aggression, such as growling, when children are around. The growl is a critically important warning sign. It’s your dog’s way of telling us she’s not comfortable around kids. If you punish her, she may learn to suppress the warning sign, making her far more likely to bite a child one day, severely and without warning.
Think about it: You can’t punish your dog into loving children! You have to use positive conditioning and reinforcement to convince her that kids are good to have around.
The older your dog is, the longer she’s been uncomfortable around children, and the stronger her response to them is, the longer this process (known as counter-conditioning and desensitization or CC&D) will take.
Of course, you’ll always supervise her around children, even if she loves them. If your dog is merely tolerant of children, you’ll have to supervise much more closely. If she’s truly uncomfortable with them, you’ll need to confine her in a safe place where children aren’t permitted, such as her crate in your bedroom, whenever you cannot actively supervise their interactions.
Preparing Your Dog for Baby’s Arrival
When a baby – and eventually a child – is coming to live at your house, your task is more daunting, and more vitally important. As soon as you know Baby’s on the way, start helping your dog get ready. Whatever changes are going to occur in her routine should happen long before Baby arrives, so she won’t associate them with the arrival of the new family member. Ideally, you’ll keep her as much of a full-fledged member of the family as she is now, finding ways to incorporate her presence into your daily baby-routine rather than excluding her.
Here are some suggestions for helping the baby’s introduction to the family positive for your dog:
• The nursery: If this is now the dog’s room, don’t wait until the final countdown to repaint and restrict her access to it. Redecorate as far in advance as possible. Put a soft cushion for your dog in one corner of the room and teach her a “Go to your bed” exercise. Whenever you’re puttering in the nursery, reinforce her with treats for lying there quietly. You can give her a food-stuffed Kong there. When you’re not in the room, use a baby gate across the doorway to keep your dog out.
• Restricted access: If you plan to restrict your dog’s access to other rooms after the baby is born, do it now, using baby gates and closed doors, and positive reinforcement to reward her for staying in approved areas. Try to allow her access to as much of the home as possible.
• Your dog’s routine: Anticipate any changes in your routine that will change your dog’s. If Mom walks her three times a day and Dad will be taking over dog-walking for a while, start making that switch now. If Dad will become your dog’s primary caretaker, have him assume those duties as soon as possible. Plan to include Baby’s presence in as many of your dog’s activities as possible, so she thinks Baby makes all the fun stuff happen.
If you intend to hire a pet-sitter to provide some dog care, integrate him or her into the routine several months before Baby arrives. If Mom plans to walk the dog while pushing the stroller, practice this while Mom is still active and agile, so she can figure out the logistics of managing leash, dog, and stroller without tipping Baby onto the sidewalk. In fact, if your dog doesn’t already have good leash manners, start immediately by standing still when she pulls on the leash and consistently rewarding her for walking with you (see “Loose Leash Walking: Training Your Dog Not to Pull“).
• Greetings: If your dog hasn’t already learned how to greet people politely, give yourself several months to teach and reinforce polite greetings. Reward her with treats and attention for sitting in front of you. If she jumps up, turn your back and step away from her. Be consistent! If you sometimes reward her for jumping up, she won’t understand that it’s inappropriate to jump up when Mom or Dad’s arms are full of Baby.
• Doorways: If your dog doesn’t already know how to wait before going through a door, there’s no time like now to teach her (see “Training Your Dog to Stay Using Cues“). You don’t want her to knock over a pregnant Mom as she comes and goes, and you certainly don’t want to worry about chasing an escaped dog down the street while Baby lies unattended on his blanket on the living room floor.
• Stairways: If you have stairs in your home, your dog may think it’s a great game to charge up and down them at your side. It’s much safer for your babe-in-arms – or for the very pregnant Mom – to either have the dog wait at the top or send her down the stairs ahead of you. Start this routine now, making it a fun, positive game. You can toss a treat or toy down the stairs for her and have her wait there until you join her, or ask her to “Wait” until you get to the bottom and then invite her to “Come on down!”
• Leave it: Teach your dog a positive “leave it” cue so she’ll happily respond (and be rewarded for it) when you ask her to stop kissing the baby, or to drop the pacifier that will inevitably fall on the floor (see “Teaching Your Dog to “Leave It” On Cue).
• Escape route: Before you know it, Baby will be crawling around after your dog on the floor. Even dogs who love kids need a getaway plan. Provide your dog with an escape route, such as a low barrier she can jump over or an elevated surface she can jump on so she can escape from Baby’s grasp when she’s had enough. Show your dog how to use it, and practice until she’s skilled at the maneuver. Dogs who are cornered by small tormenters without a way to escape may feel compelled to bite in self-defense.
How to Handle Your Dog When the Baby Comes Home

When Baby arrives, your dog will be excited to see Mom after she’s been away. The day before Mom and Baby come home, have Dad bring home a blanket that’s been wrapped around Baby, to pick up his scent. Show the blanket to your dog. Let her sniff it, and feed her yummy treats. Then put the blanket in her bed. When Baby comes home the next day, his scent will already be familiar to your dog.
When you all get home, have Dad hold Baby outside while Mom goes in to greet your dog. If the dog forgets her polite greeting manners in her excitement, she won’t hurt Baby, and she won’t get yelled at. You don’t want her first introduction to Baby to be negative! Then have Dad come in with Baby, while Mom has treats ready to reward the dog for greeting Dad and the human puppy nicely.
Rather than banishing the dog to the backyard while everyone settles in, encourage her to lie calmly on her rug, or if necessary, use a tether to keep her out of the midst of chaos until things calm down (see “Tethering Your Dog for Training“). Have Mom sit on the sofa with Baby while Dad rewards the dog’s good behavior on her rug with treats, praise, and a Kong stuffed with irresistible goodies.
If you’ve done your homework well, your dog will soon love Baby as much as you do, and you’ll have successfully set the stage for a long and happy relationship between your dog and your child.
NEWBORNS AND DOGS: OVERVIEW
1. Enlist the help of friends with children and neighborhood children to socialize your pup during his optimum socialization period up to the age of 14 weeks and beyond.
2. Find locations (vet’s office? groomer’s?) where there will be sympathetic, dog-friendly folks willing to help you with remedial socialization for your adult dog.
3. Make preparations for your new baby well in advance so the experience is as positive and stress-free for your dog as possible.
Download the Full May 2005 Issue PDF
Join Whole Dog Journal
Already a member?
Click Here to Sign In | Forgot your password? | Activate Web AccessWhen a Low-Protein “Kidney Diet” Is Not the Answer

Every day, thousands of dogs are diagnosed with kidney disease. The first suggestion most conventional veterinarians make is to switch from whatever the dog has been eating to a low-protein “kidney diet” food. Clients are sent home with bags or cans of “prescription” food and warned not to feed high-protein foods or treats of any kind.
Most dogs, even chow hounds, approach their new, low-protein food with suspicion, since these diets are generally much less palatable than foods that contain more animal protein. Many refuse to eat. Conventional veterinarians are used to this response and tell their clients to stick to the new food for their dogs’ own good. “Your old food is too high in protein and will actually speed kidney failure,” they warn. “Keep giving him the prescription food. He’ll come around when he gets hungry enough.”
Eventually most CRF patients do accept their new food, though without much gusto or enthusiasm. Worse, despite their food’s low protein levels, the dogs’ slow deterioration continues.
After their dogs have died, many owners look back and wonder whether they did the right thing. Now a new approach to feeding dogs with kidney disease offers a different scenario – one that’s more likely to keep CRF dogs, and their human companions, happy.
A paradigm shift
It’s a fact of life that not all medical discoveries and “breakthroughs” in disease treatment prove to be as promising as they seemed at first. Adopted on the basis of a few small, encouraging studies, some strategies are found later to cause mixed or even adverse results.
This is definitely the case with the currently predominant treatment strategy of giving dogs with CRF a low-protein diet. Newer research has radically changed and fine-tuned the dietary recommendations for canine CRF patients. Those using the latest recommendations to feed their CRF dogs a therapeutic home-prepared diet report excellent results. Best of all, most dogs love the combination of high-quality protein and freshly prepared ingredients.
About CRF
Chronic renal failure affects male and female dogs of all breeds and all ages. Its underlying cause may be hereditary or related to inflammation, tick disease, progressive degeneration, damage following acute renal failure, or unknown causes. Acute renal failure may be triggered by a trauma injury, exposure to poisons like antifreeze or rat poison, or damage caused by medications, bacterial infections (such as leptospirosis), fungal infections, or dehydration.
Many animals born with poorly constructed or poorly functioning kidneys succumb to kidney failure at a young age. Most cases of chronic renal failure are seen in dogs age seven or older. Chronic nephritis, a common diagnosis in CRF patients, involves low-grade, long-term inflammation of kidney tissue that causes permanent damage to delicate renal tissue.
The protein debate
As soon as they diagnose kidney disease, most American veterinarians prescribe a low-protein diet. They believe that protein harms the kidneys and that reducing protein consumption slows the progress of kidney degeneration. This is because early research on rats was assumed to be true for dogs, and excess protein causes problems for rats. A number of pet food manufacturers sell low-protein prescription diets for dogs with chronic renal failure, and those who prepare their own food at home are warned against feeding meat, poultry, and other foods that are high in protein.
“Those recommendations are based on a myth,” says Wendy Volhard, author of Holistic Guide for a Healthy Dog. “In fact, the whole theory of low-protein diets for dogs with kidney disease was blown apart in 1975 by David Kronfeld, PhD, who was at the time a veterinary researcher at the University of Pennsylvania. His concept was not to feed less protein but rather to feed higher-quality protein.
“The low-protein myth is like an old-wive’s tale, something based on ignorance that just won’t die. Yes, inferior-quality protein can harm a dog’s kidneys, but the solution isn’t to continue with inferior-quality ingredients and feed less of them. The solution is to improve the quality of ingredients and in that way provide what the dog needs for good health.”
Studies disproving the prevalent low-protein prescription have been widely published in veterinary journals and textbooks. But it is moving into the mainstream very slowly.
“Most vets who did not graduate from college in the last few years (and some of those as well) are still unaware of or dismiss the newer studies that show low-protein diets neither slow the progression of kidney disease nor prolong life,” says Mary Straus, a lifetime dog lover from the San Francisco Bay area who researches health and nutrition issues.
“Too many dogs are forced to eat Prescription Diet k/d® or similar low-protein prescription foods,” says Straus. “These can actually cause harm. When protein levels are very low, the body will cannibalize itself to get the protein it needs. This creates more waste products than if you feed the proper amount of high-quality protein in the first place. Also, k/d is not very palatable, and many dogs with kidney disease will eat only enough of it to survive, or stop eating entirely if that is all they are offered.”
Older dogs actually require a higher level of protein to maintain their body stores of protein than do younger adult dogs, says veterinary nutritionist Patricia Schenck, DVM, PhD, of Michigan State University’s Center for Veterinary Medicine. In an article published in Veterinary Nutritionist, Dr. Schenck wrote, “Reducing dietary protein in older pets may have adverse effects. As pets age, their ability to utilize nutrients decreases. The only time dietary protein restriction is appropriate in renal failure is when the disease has become severe.”
Healthy geriatric dogs require about 50 percent more protein than young adults, say canine health writers Susan Thorpe-Vargas, PhD, and John C. Cargill, MA. Depending on the quality of the protein, they say, it should make up 20 to 30 percent of total calories ingested. “Protein restriction can result in impaired wound healing, diminished immune function, and lowered enzyme activities and cellular turnover. Dogs with impaired renal function do better with dietary phosphorus restrictions.”
A new action plan
Mary Straus’s dog Nattie was a healthy, athletic Chinese Shar-Pei who had no trouble keeping up with young dogs even at 10 and 11 years of age. She ate kibble and received annual vaccinations until 1997, when Straus learned about the health benefits of raw diets and the harm that can be caused by repeated vaccinations. Nattie was 10 years old when she was converted to a raw diet and stopped receiving vaccinations. Four years later, at age 14, Nattie was diagnosed with kidney disease. After much research, Straus put the newest diet plan into place for Nattie.
“I modified her diet to reduce its phosphorus but kept her protein levels high,” says Straus. “Her diet was around 37 percent protein on a dry matter basis, and she thrived. Her kidney numbers actually improved for two years, and when she died at age 16, her illness had nothing to do with kidney disease.
“People need to know this information, as well as how to formulate a homemade diet or what foods to add if they are going to feed k/d or one of the other low-protein commercial diets for kidney disease.”
Dietary goals
When developing a diet for dogs with kidney failure, the recommendations from leading experts are to feed:
- Moderate to high amounts of fat
- Moderate amounts of high-quality protein
- Low amounts of phosphorus
- Moderate amounts of low-phosphorus carbohydrates
- Plenty of water, juices, broth, and other liquids
Although guidelines vary, a sensible goal is a diet whose total calories come 1/3 from fat, 1/3 from protein, and 1/3 from carbohydrates.
Fat provides calories and energy, and most dogs have an easy time digesting it. Good sources of saturated fat include fatty meats, butter, whole-milk yogurt, egg yolks, and coconut oil.
Polyunsaturated vegetable oils, such as canola, corn, soy, safflower, sunflower, and flax seed oil, are not recommended for CRF patients. Neither is cod liver oil, because of its high vitamin D content, which failing kidneys have difficulty processing. But fish oil (fish body oil, not fish liver oil) has been shown to help dogs with CRF.
When adding fats and oils to the home-prepared diet, start with small amounts and increase quantities gradually. Too much too soon can lead to diarrhea. Dogs prone to pancreatitis should be carefully monitored.
What are the best sources of protein? Most experts consider eggs to contain the highest-quality protein, but their yolks contain moderate amounts of phosphorous. One strategy for feeding eggs to CRF dogs is to feed one or two egg whites for every whole egg. Calcium is a phosphorus binder, so add small amounts of finely ground eggshell to each meal (½ teaspoon per pound of food) to help reduce the amount of phosphorus absorbed by the body.
Other foods high in phosphorous include bones, fish with bones, cheese, and organ meats. “Bones are so high in phosphorus,” says Straus. “that I would avoid them or feed them in small amounts, such as one-third the normal quantity, even with early stage CRF. Like egg yolks, organ meats such as kidney and liver contain many nutrients that are important for canine health and should be included, but in moderate amounts.”
Feeding a low-phosphorus diet has been shown to benefit dogs with kidney disease. Bones are very high in phosphorus and should be eliminated or fed in very small amounts. When formulating a diet for a CRF patient, never add bone meal, but instead use a calcium source that does not include phosphorus, such as ground eggshells or calcium carbonate.
Other foods high in phosphorus include dairy products (especially cheese), fish with bones, organ meats, and egg yolks. These are nutritionally dense foods, so they should not be eliminated from the diet. Instead, feed them in reduced amounts in combination with low-phosphorus grains and vegetables. Low-fat meat is higher in phosphorus than fatty cuts, so unless your dog has a problem with fat, feed higher-fat meats and whole-milk dairy. Always add calcium, which acts as a phosphorus binder, to all meals. You can use ½ teaspoon ground eggshell, or around 1 gram (1,000 mg) calcium, per pound of food.
On her DogAware website, Mary Straus lists recommended phosphorus levels for dogs of different weights in different stages of kidney disease along with nutritional information, including calories and phosphorus levels, of dozens of common foods. To help caregivers plan their dogs’ menus around phosphorus levels while providing enough calories to prevent weight loss, a common problem in CRF dogs, Straus color-codes these foods.
■ Code Red: Feed in small amounts. These include low-fat meats such as ground turkey, lean ground beef, or skinless chicken breast; organ meats, such as beef heart, chicken liver, beef liver, or beef kidney; canned fish, such as jack mackerel, pink salmon, or sardines in tomato sauce or water (not oil); high-phosphorus grains such as oatmeal; dairy products such as cottage cheese, whole-milk yogurt, whole-milk mozzarella cheese, cheddar cheese, or whole eggs and egg yolks. Raw meaty bones, including chicken parts (backs, necks, wings, and legs) and turkey necks should be fed in limited amounts, if at all.
■ Code Blue: Feed in moderate amounts. Higher-fat meats such as dark-meat chicken and skin, 20-percent-fat ground beef, pork, lamb, and liverwurst; green tripe; winter squash such as acorn or butternut; and whole grains such as brown rice, millet, and whole-wheat bread.
■ Code Green: Okay to feed in large amounts. Egg whites, yams or sweet potatoes, white potatoes, cereals such as Cream of Wheat, Cream of Rice, or Malt-o-Meal, glutinous (sticky) rice, white rice, barley, and white bread. Grains should be cooked, and boiling vegetables may reduce their phosphorus levels.
Further diet tips
Recently, green tripe, a food traditionally fed in Europe, has become a staple for many American dogs, including CRF patients. Green tripe is the raw, unprocessed stomachs of cud-chewing animals like cows, goats, or sheep. Supermarket tripe is white because it has been bleached and deodorized, which destroys fragile nutrients. Green tripe contains easily digestible protein, beneficial bacteria, abundant enzymes, and relatively low phosphorus levels.
Tripe smells awful to humans but sublime to dogs, including CRF patients who have otherwise lost interest in food. Thanks to increasing demand, frozen green tripe is available from mail order sources and some local distributors of raw frozen foods.
If you choose to feed a prescription dry or canned food rather than a home-prepared diet, add fresh protein foods, either raw or cooked, such as meat, eggs, egg whites, and tripe, especially in the early stages of the disease.
If you feed a diet based on raw meaty bones, substantially reduce the amount of bone. If the diet calls for bone meal, like the Natural Diet developed by Wendy Volhard, follow her advice to switch from lean to fatty meats and substitute calcium carbonate for the bone meal to reduce phosphorus levels.
While dogs are not designed to consume grains or starchy vegetables, most CRF diets include up to 50 percent carbohydrates in order to provide calories and nutrients while keeping phosphorus levels low. Steaming or boiling vegetables reduces phosphorus levels if you discard the cooking water. Alternatively, puree or juice them to improve assimilation. Note, however, that dogs with arthritis may be sensitive to nightshade plants, which include white potatoes, peppers, eggplant, and tomatoes.
Whole wheat, oatmeal, brown rice, millet, and other whole grains are moderately high in phosphorus and should not be fed often or in large amounts. White rice is low in phosphorus, and glutinous or sticky rice is the lowest-phosphorus grain. To help make grains more digestible (as described in “It’s All in How You Make It,” WDJ March 2001), soak them overnight to remove enzyme-suppressors and naturally occurring toxins.
“I have had good luck with Malt-o-Meal, which is low in phosphorus,” says Straus. “You have to be careful about feeding vegetables to dogs with kidney disease. I recommend using white potatoes and yams because they provide a lot of calories without adding much phosphorus, unlike many of the low-cal veggies.”
Dogs with high blood pressure, which can be related to kidney disease, may need reduced salt in their food. Home-prepared diets are naturally low in salt, but cottage cheese is high in salt, canned fish can be rinsed to remove salt, and processed foods should be checked for their sodium content.
Because dehydration creates serious problems for dogs with kidney disease, it’s important to provide abundant water. “Make sure fresh water is always available,” suggests Straus, “even if excess drinking causes your dog to become incontinent. If your dog already drinks a lot of water, ask your vet about giving subcutaneous fluids to help the dog stay hydrated.” Hard water contains minerals that are best avoided, so use filtered or low-mineral bottled water.
Dogs with kidney disease can lose interest in food, so look for foods and flavors that can revitalize a flagging appetite. “It’s important for these dogs to eat something,” says Straus, “even if it’s not one of the recommended foods. Try offering your dog’s food at different temperatures, experiment with raw versus cooked, and offer multiple small meals rather than just one or two large ones. My Nattie wouldn’t eat raw eggs, but she loved eggs scrambled with a bit of cheese. The cheese wasn’t the best thing for her, but it got her to eat.”
Green tripe can be added to food as a flavor enhancer, as can Seacure, a very fishy-smelling powder sold as a protein supplement. “If you feed a commercial food like k/d and your dog won’t eat it, find something else, preferably a homemade diet that provides high-quality protein while controlling the amount of phosphorus,” she says.
Plus, she adds, most dogs love fresh food. “The higher moisture levels in fresh foods help protect their kidneys, and they feel better and enjoy life more.”
Coenzyme Q10. In a recent human study, kidney disease patients improved on a dose of 60 mg CoQ10 three times daily. Adjust this for your dog’s weight by using 15 mg per 25 pounds of body weight, three times daily.
Vitamin E, 50 IU daily per 25 pounds of body weight. Also give vitamin B-complex and moderate amounts of vitamin C, around 500 mg for a 50-pound dog. Avoid multivitamin/mineral products that contain phosphorus or vitamin D. Buffered or ascorbate forms of vitamin C may be easier on the stomach.
Glandular supplements that support the kidneys are often recommended by holistic veterinarians. Canine Renal Support from Standard Process is available from veterinarians, licensed health care practitioners, and some online sources.
Herbal supplements. Traditional kidney tonics include dandelion leaf and root, couch grass, and marshmallow. Look for teas and tinctures that contain these and other gentle, supportive ingredients, or consult Herbs for Pets, by Mary Wulff-Tilford and Gregory Tilford (BowTie Press).
Also With This Article Click here to view “Can Meat Cause Kidney Failure”
A Close Look at Dog Collars
by Nancy Kerns
Dogs have become very popular in the last decade or so, and with their increasingly higher-profile place in our society, there has been a boom in businesses that create unique and useful dog-care products. Collars might just be the most ubiquitous.
There’s an adage: “Build a better mousetrap and the world will beat a path to your door.” We think it ought to be dog collar. There are now hundreds of special-purpose collars on the market: products that purport to prevent pulling, safety collars that release under tension, light-up or reflective collars for walking in the dark, collars with built-in retractable leashes or poop-bag dispensers . . . the list is almost endless.
Equally endless is the selection of plain old “regular” collars, products that provide only the most basic services: offer a place to secure your dog’s ID and your leash. It’s astonishing how much variety can be brought to the most basic product. Even in the “regular” collar category, there are products that emphasize certain abilities: increased strength, for example, or comfort, light weight, smoothness on the coat, or ease of use. Or, of course, fashion. Collars that look cool while working well – what more can you ask for?
Selection Criteria
Sometimes when we do a review of a certain type of product, there are only a few to examine, so we can try them all and tell you which ones performed well and which ones you shouldn’t waste your money on. Since this category is so huge – even with specialty collars excluded – all of the products we are going to tell you about in this review qualify as “top picks,” earning our four-paw rating (see “Rating System and Product Details” sidebar). We won’t bother telling you about the many products that failed our in-store examination, or the catalog-sourced products that disappointed us. We’d rather use the space on products we really like.
What, exactly, do we like in a collar? To start, we look for top-quality materials – leather that is soft and supple, evenly dyed, neither greasy nor dry; nylon that feels smooth and pliable; and buckles and snaps that open and close easily and securely. Next, we examine the quality of the workmanship. We want to see tight, even stitching, and nylon ends that are smoothly heat-sealed to prevent fraying. The collar should be constructed in such a way that it lies nicely around the dog’s neck, without pressing or bending inward in a way that could rub or otherwise cause the dog to be uncomfortable.
Next, we look for products that are easy to use. Sometimes this is a result of good hardware – for example, when the maker utilizes a D-ring that is especially large, making it easy to clip a leash onto it. In other cases, the ease-of-use is a result of good workmanship, such as when the holes for a buckle are punched a little on the large side, to make it easier to align the tongue of the buckle with just the right hole.
Last, but not least, we look for products that offer a lot more than the usual amount of attractiveness. Hip? Elegant? Showy? Any and all qualify.
Okay, let’s get on with it. In no particular order, here are the collars currently on the market that we like best.
Hemp Collars
Wow! Hemp has to be the softest, most comfortable, but strong fabric we’ve ever felt. Planet Dog has put the material to great use in its flat collars, available in an unlined style or lined with a soft fleece material.
As we went to press, we learned that Planet Dog recently discontinued its models with the belt-type buckles (shown in center and left, above) in favor of metal side-release style buckles. (The smallest size has plastic buckles – lighter for little dogs.) We liked both types, but the side-release models are more adjustable, so it’s fine with us.
We were originally attracted to the fleece-lined collar for dogs we know with very thin coats; leather, nylon, and even cotton can rub bare spots on some of these dogs’ necks and throats. The fleece does a nice job of keeping the coat intact, but we found that the unlined hemp was easy on these dogs’ coats, too. We also liked the ample size of the D-rings for attaching leashes.
Planet Dog offers these collars in just a few groovy colors: apple-green, orange, and purple. Matching leashes are available.
The company literature claimed that hemp takes washing well, and just gets better with time. That’s been our experience so far.
Soft Web Collars
There are dozens of nylon collars on the market, but we don’t know any company besides White Pine that uses this very soft, silky nylon for its collars (and leashes, long lines, and harnesses). It’s an absolute pleasure in the hand, making the order of a matching leash a necessity! The material is colorfast and can be washed frequently without stiffening. The collars come in a variety of widths, from 3/8″ (which is very lightweight, for tiny dogs) to an attractive 1″ for big dogs. They are also available in a wide variety of bright, pretty colors.
The Soft Web collars are available in two styles: the “Soft Snap,” which has a plastic side-release buckle (shown in the center of the photo above), or the “Soft Slip” (the outer collar in the photo), which is a limited-slip collar. The latter type of collar tightens slightly with leash tension to prevent a dog from slipping out of it, but if properly fit, they cannot choke a dog). The D-rings on the collars are black stainless steel. Best of all is the reasonable price.
Tail Waggin’ Collars
These are the second-most expensive collars we’ve featured here, but also the most attractive, in our opinion – colorful, unique, well-made, and perfectly functional.
Wendel Wirth, proprietor of “a tail we could wag” (yes, it’s spelled with all small letters), made the first “Tail Waggin’ Collar” for her own dog out of an old leash and a worn Guatemalan sash. She and her dog received so many compliments about the collar, that she began sewing a limited number of the collars and selling them in a local bar and grill. A thriving business was born.
Wirth now offers collars (and matching leashes) in a number of gorgeous patterns, all of which are traditional Mayan designs, woven for the company by native Mayans in Guatemala. The woven cotton is then stitched to a strong, soft nylon backing. The hardware used includes large solid brass D-rings and plastic side-release buckles that are slightly curved, for the dog’s comfort. Little touches like these really improve the performance of a product, and we just love these collars.
Top Rope Collar
This flat collar has a couple of cool features that almost make it too “tricked out” to include in this “regular” collar review.
It gets its name by virtue of an elegantly simple (and probably soon-to-be-copied) feature: a plastic “keeper” that keeps a large D-ring conveniently positioned at the back of the dog’s neck, where you can quickly and easily snap the leash on and off. Plus, with the leash fastened at the back of the dog’s neck, he’s less likely to step over the leash when you’re not paying attention. Too cool! An extra-heavy side-release buckle also serves as “ballast,” helping to hold the collar in the “right” position. This might prove a bit too clunky for a very small dog, but then again, the smallest size can be adjusted down to only nine inches, so perhaps this is self-limiting.
Another innovative feature (shared by some of Ruff Wear’s other collars) is a separate plastic loop, sewn onto the nylon fabric, for your dog’s ID tags. No more accidently clipping the leash onto the flimsy little ring the ID tags hang on!
The Top Rope Collar is available in four solid colors and four cool patterns.
Knot-A-Collar
Here’s another basic collar from Ruff Wear with some neat “extra” features.
The Knot-a-Collar has a minimal appearance that some owners will like; it looks like just a bit of light, mountain-climbing-type rope tied around the dog’s neck. But as the name suggests, the knots that the collar is tied with are what makes it special. You slip the buckleless collar over the dog’s head; it takes two hands pulling on the collar a certain way to adjust its fit. When a leash is attached properly to the stainless steel ring on the collar, no amount of tension will make the collar tighten. But if the dog snags the collar on something, it will slide loose enough to free him.
Ruff Wear has again included a separate ring on which the dog’s ID tags can be hung, so you don’t accidently snap the leash onto the flimsy ID tag ring.
The Knot-a-Collar is available in three colors and two widely adjustable sizes.
Mrs. Bones Collars
Okay, we know: That’s a crazy price for a dog collar. These collars are for dogs who belong to completely dog-crazy people.
All of Mrs. Bones collars are made of washable fabric, and use solid brass hardware, or in some designs, plastic side-release buckles. That’s the only generalization we’ll make about these collars, because the company offers a head-spinning array of deluxe fabrics and patterns to choose from. The tiny ones start at 5/8″ wide; the giant collars are up to 2″ wide. The fabrics include velvet, brocade, tartan, and silk-lined models.
All of Mrs. Bones collars are available in three different basic forms. The first has a standard plastic side-release buckle (the nice, curved kind). The second is what Mrs. Bones calls a “sighthound” style – a “limited slip” design that slides over the dog’s head and then is adjusted to fit. The D-ring for leash attachment is sewn into a separate loop of fabric that tightens to a limited degree with tension on the leash.
The final style is a “single loop” design that also passes over a dog’s head and is adjusted with a slider to fit. The latter style is particularly well-suited for tiny dogs or dogs with delicate skin or coats, since there is no buckle to rub the coat or irritate the dog’s neck.
Simply put, Mrs. Bones has the biggest offering of really gorgeous and unique designs available; there are several hundred styles and sizes to choose from, and the collars are custom-made for your dog. If it’s important to you to have the only collar of a particular kind in your whole town, Mrs. Bones is the place to shop.
Presidio Collar
This is a very simple collar that makes our list by virtue of the unique material it is made of: BioThane, a patented material made of a polypropylene webbing that is coated with urethane.
Used increasingly in horse tack, BioThane is an incredibly strong, flexible material, and available in a wide variety of vivid colors (and even a glow-in-the-dark option for an extra $2, but we didn’t test that one). BioThane is also waterproof, if the material is heat-sealed at every spot where it is cut or punched. We couldn’t detect evidence of heat-sealing in the products we tested, but even if OllyDog doesn’t do it, it’s a simple thing to do yourself, with a fire-heated blade or screwdriver.
These collars are lightweight, smooth, and so flexible, they must be comfortable. They can be ordered in one of two widths: 3/4″ or 1″. The hardware appears to be high-quality stainless steel. Best of all, the material can be kept clean and odor-free with the wipe of a sponge.
Dog Crating Difficulties
The topic turned to crating on one of my trainer e-mail lists recently. I was horrified to read that some shelters and rescue groups refuse to adopt to prospective owners who intend to use a crate with their dogs. What madness is this?
I first discovered crates some 30 years ago, when they were relatively new to the dog scene. I was skeptical about putting my new Australian Kelpie puppy in a “cage,” but since Keli was part of a Canine Field Agent program for the Marin Humane Society where I worked as a Humane Officer, I was determined to do everything perfectly right. I reluctantly decided to try crating.

On the third night, when I went to deposit Keli in her crate, I found Caper, my three-year-old Bull Terrier, happily curled up in the pup’s den. Caper smiled up at me and thumped her tail in the blankets, clearly saying, “This is wonderful! Can I have one of my own? Please, can I?”
I bought Caper a crate of her own the next day, and have been a total crate advocate ever since. How could they now be perceived as a bad thing?
As I followed the discussion, I realized that the negative crate perspective stemmed from concerns of “overcrating.” Apparently some owners crate their dogs all day while they’re at work, let them out for a couple of hours when they come home, and then crate the dogs all night while everyone is sleeping. This, some shelters fear, is too much time in a crate for a dog’s physical and mental health.
They’re right.
The crate is an invaluable management tool. Like any training tool, it can be misused. Even when used properly, it’s not necessarily the appropriate tool for every dog in every circumstance. The discussion that follows may help you decide when, and whether, it’s the right choice for you and your canine pal.
Overcrating Dogs
A properly used crate can be the answer to your housetraining prayers. I was astounded by the ease with which I was able to housetrain my Kelpie pup. I also, however, was in the enviable position of being able to take my baby dog to work with me, so I was never tempted – or compelled – to crate her for longer that she could “hold it.”
If you’re a normal person whose boss frowns on dogs at work, you simply can’t crate your pup all day while you’re gone. He’ll be forced to eliminate in his crate, breaking down his inhibitions against soiling his own den – the very inhibitions you rely on to be able to accomplish house-training.
A general rule of thumb is that puppies can “hold it” during the day for up to one hour longer than they are months old. In other words, your eight-week-old baby dog can be crated for perhaps up to three hours during the day. They can usually go somewhat longer at night because metabolism slows, but it’s a rare two-month-old who can go through the night without a potty break.
So, you can only crate your pup during an 8- to 10-hour workday if you can arrange for at least two bathroom breaks. One quick run home at lunch won’t be enough, at least not until he’s five to six months old.
In addition to performing necessary bodily functions, a growing pup needs to move around in order to develop properly. Some runaround time during the day helps him develop mentally and physically, practicing skills and learning lessons he can’t make up later in life.
Finally, a pup who spends his entire day in a crate stores up mental and physical energy. When an owner comes home exhausted after working all day, she’s rarely in a state of mind to cope with pent-up puppy frenzies, or to provide adequate exercise and mental stimulation to make up for a day of relative deprivation. The rela-tionship suffers, and the pup gets relegated to the backyard, alone, or worse – put back into the crate.
While adult dogs are more physically capable of “holding it” for extended periods than puppies, it’s still not appropriate for a dog to be routinely crated for 10 hours. Hence, the concerns of adoption agencies.
Solution for Overcrating Your Dog
Alternatives to crating include finding alternative confinement options, arranging for multiple bathroom breaks, or finding a daycare situation of some kind.
Some owners simply leave their dogs – including puppies – outside in a fenced yard during the day. This allows the dog total freedom to poop and pee at will. It also leaves him vulnerable to threats from the environment – theft, poisoning, accidental escape, snakes, raccoons, skunks, coyotes. I even met a pup once with a huge scar across his back – souvenir of a brief flight, fortunately aborted, in the talons of a Golden Eagle.
Outdoor confinement also leaves the dog free to practice inappropriate behaviors such as digging, escaping, and barking, and exposes him to the extremes of weather.
It might be safer to confine your pup indoors, either in a small puppy-proofed room such as a bathroom, or in a secure exercise pen. This requires newspapering the floor, and perhaps encouraging the dog to use one of the commercial pee pad products or a litter box, essentially giving him permission to eliminate in the house.
This solution has risks as well. Your pup can learn to rip up vinyl flooring and chew on cabinets if he’s loose in a bathroom. He may be able to knock over his exercise pen if it’s not well secured, climb out (some come with lids), or get a leg caught between the bars. If you plan to use an ex-pen, get him used to it while you’re home, to be sure none of these things are likely to happen.
Multiple bathroom breaks may be easier than you think. If there are two adults in the household, perhaps you can stagger your lunches – one at 11am, one at 1pm – to give him two breaks. If not, a commercial pet sitter can take a daily turn at potty breaks. Other options include friends, neighbors, or family members who live close enough to provide the service until the pup is older. You might even find a local teenage dog lover who would cherish the opportunity to earn some spending money.
Finally, Spot may just need to go somewhere else during the day. Commercial doggie daycare centers are increasingly popular and available.
If Your Dog Soils His Crate
If Spot eliminates in his crate even when not overcrated, your first course of action is to rule out medical problems. Loose stools, a urinary tract infection, or other incontinence problems make it impossible for a dog to hold it for normal periods of time.
Assuming all is well, there are several other possible causes of crate soiling:
• Your dog has been routinely overcrated in the past, and was forced to soil his crate. His inhibitions against soiling his den have been damaged. He now thinks the crate in an acceptable bathroom.
• Your dog isn’t eliminating outdoors before being crated.
• Your dog has separation anxiety (SA) and is voiding his bladder and bowels during his SA panic attack.
Solution for Crate-Soiling
Your approach to Spot’s crate-soiling behavior depends on the cause. If he has learned to soil his crate, it may help to change his bedding, or remove bedding altogether until he’s retrained. Bedding that absorbs fluids, such as a blanket, can make it more comfortable for your dog to be in his soiled crate. His current bedding also may have become his preferred substrate. Try newspaper instead, a square of heavy duty compressed foam rubber (the kind used for flooring), or no bedding. A tether may be a reasonable alternative to nighttime crating.
Make sure his crate is the correct size – big enough for him to stand up, turn around, and lie down comfortably. If it’s too large he can potty in one end and sleep in the other.
Perhaps you’re just not making sure Spot eliminates outside before you crate him. In your morning rush to get to work on time, you let him out in the backyard and assume he empties before he comes back in. That may be an incorrect assumption. If it’s cold or rainy, he may have huddled on the back porch, waiting to be let back in. Perhaps he was distracted digging for moles under a bush, or barking at the kids walking past the yard on their way to school. Maybe he gets a cookie for coming back into the house, so he’s skipping the step where he’s supposed to go pee on the grass first. It could be a substrate preference problem – he wants to pee on grass, and all he can find is snow!
Set your alarm to awaken you 15 minutes earlier than normal, so you can go out with Spot on leash before and after he eats his breakfast to make sure he’s empty when you crate him. If he’s reluctant to out in inclement weather, create a sheltered potty spot, so he doesn’t have to eliminate with rain or snow dumping on his head, or strong winds buffeting him. Would you be able to “do your business” under those conditions?
If he’s determined to go on grass, it’s the dead of winter and there’s no grass available, you may need to scrape snow away from the grass in his sheltered potty spot or provide indoor-grown grass until you can teach him a new substrate preference. Maybe Astroturf would work!
When Your Dog Refuses to Go Into the Crate

Dogs who refuse to enter their crates may have never been crate trained, or the crating process was somehow abused. Spot may have been overcrated and now resists entering a den he fears he’ll be forced to soil. Perhaps someone previously used his crate as punishment, or forcibly crated him. He may have had a bad experience in a crate that may have been improperly secured and rolled with him in it, or by having loud noises or other fear-inducing stimuli occur while he was crated.
Teach Your Dog to Love the Crate
Whatever the reason, you’ll need to embark on a program of counter-conditioning and desensitization to change Spot’s association from bad to good, and retrain his crating behavior.
Start by scattering yummy stuff around the outside of his crate, placing a couple of tidbits just inside the door so he can stick his head in to get them. Gradually toss more yummies inside the crate to entice him further in. When he’s going in easily, start handfeeding tidbits while he’s inside, to encourage him to stay in. If you use a clicker, you can now begin to click! and give him a treat for going into the crate.
When he’ll go in and stay calmly inside the crate while you feed treats, close the door gently, feed treats through the door, and then let him out. Gradually increase the length of time you keep the door closed, until he’s quite comfortable with this step. Then take a step away from the crate, click! and return to give him his treat. Continue this process until he is happy to enter and stay in his crate.
You can play another crating game to motivate your dog to “kennel.” Take something scrumptious, like a meaty knucklebone, and put it in the crate. Show it to your dog, then close the door with him outside the crate. Let him spend some time trying to get into the closed crate to get at the bone, then open the door allowing him to zoom in (and back out, if he wants) to claim his prize.
To keep crating fun for your dog, be sure to practice crating games often, not just when he’s going to be crated for extended periods. You can also give him food-stuffed Kongs and other interactive toys to keep him happy in his crate.
If your dog absolutely refuses to enter the crate, get one that comes apart. Take the top off, then start the counter-conditioning process.
Incessant Barking in the Crate
Sometimes barking happens because the dog really needs to go. While it’s critically important to heed your dog’s bathroom calls, it’s equally important not to succumb to crate barking when it’s simply his insistent plea to get out and play, or cuddle. The more often you let him out on demand, the more the behavior is reinforced, and the harder it will be to ever successfully train him to stay quietly in his crate.
Solution to Barking in the Crate
If you’re just starting your dog’s crating lessons, be sure he empties his bowels and bladder before you begin, so you know he doesn’t have to go. Ignore his barking, and let him out of the crate when he’s quiet. At first, he may be quiet for just a few seconds. Mark the quiet with a “Yes!” or a click! so he knows it’s the quiet behavior that gets him out of the crate. Gradually increase the length of quiet time before you let him out.
If your dog has already learned to demand-bark to gain freedom you’ll follow the same procedure as above. However it will take longer to extinguish the behavior because it’s been previously reinforced. Your dog is likely to go through an extinction burst – more and/or louder barking, as he tries to make this formerly successful behavior work again. Be strong; if you give in during an extinction burst you will reinforce your dog for an even more intense behavior, and it will be even harder to make it stop.
At first, listen for and reinforce even very brief pauses in barking. You have to show your dog what behavior will work – quiet – if you want him to offer more of it.
When Your Dog Panics in the Crate
This is very different from demand barking. Some dogs, particularly many of those with separation anxiety (SA), can’t tolerate the close confinement of a crate. They experience a full-blown panic attack, and frantically try to escape from their prison.
A panicked dog’s efforts to escape from his mental and emotional anguish may include hysterical, non-stop barking and howling – for hours and hours without pause; frantic attempts to bite and claw his way out – often breaking teeth and ripping out nails in the process; and stress-induced urination and defecation – which he proceeds to paint all over the walls of his crate as he thrashes around.
Solution to Panicking: Don’t Crate the Dog
You cannot subject a panicked dog to these conditions. You must address the SA problem through behavior modification, and may someday be able to use a crate with your dog, if you are successful in modifying the SA. In the meantime, look for doggie daycare-type management solutions.
When Your Dog Gets Aggressive in the Crate
Some dogs become ferocious in their crates, usually manifesting territorial aggression, fear aggression, or resource guarding. The behavior is alarming, especially to an unsuspecting passer-by – human, canine, feline, or other – who inadvertently walks too close to the crate and is greeted with a fierce roar and crash when the dog lunges into the side of his kennel.
Managing Dog Aggression in Crates
Management is your best approach to this behavior, followed by behavior modification.
Dogs who are aggressive in their crates shouldn’t be subjected to environments in which the behavior is constantly triggered. These dogs should not, for example, be left crated and unattended at canine sporting events. If children are in the household, they must not be allowed to approach Spot in his crate.
Some dogs will crate calmly if the crate is covered to reduce the stimuli that triggers their aggression. Others do well as long as there’s nothing of high-value to be guarded in the crate, such as a favorite toy or stuffed Kong.
If Spot is fearful, taking refuge in his crate out of fear, be sure to do nothing to intimidate him while he’s crated. No reaching in, for example, to remove bowls, toys, or dog from crate. You may do better to refrain from crating a fearful dog until he’s become more confident with you, to avoid setting him up for crate aggression.
To modify crate aggression, return to your old friends, counter-conditioning and desensitization. If your dog is aggressive to passers-by, arm yourself with a large supply of high-value treats (canned chicken, rinsed and drained, works well), and sit next to the crate. When your dog alerts to a member of the trigger species (whether it is dog or human) passing at a noticeable but low-arousal distance, begin feeding him treats, non-stop, until that someone is gone. Each time the trigger appears, wait for your dog to notice, then start feeding him tiny tidbits of chicken, non-stop, until the trigger is gone.
Keep watching your dog’s reaction. You’re looking for his response to the appearance of the trigger to change from wary or alert to “Yay! Where’s my chicken!” When you get the latter reaction consistently, move the trigger closer and repeat the lessons, until the trigger can pass next to the crate.

If your approach triggers an aggression response, do lots of practice sessions where you walk up to the crate and drop chicken into it, so your dog learns to associate your approach with good stuff. Never punish your dog for being aggressive in his crate – you’re likely to make the behavior worse!
The Best Kinds of Crates
Some dogs crate best in wire crates, others seem to prefer the plastic airline-style kennels. Portable, collapsible soft crates have become hugely popular. Some owners only crate through the puppy stage, others use crates throughout their dogs’ entire lives. Both are acceptable.
Despite the potential for crating woes with some dogs, I remain a staunch fan of this invaluable management tool. We can educate owners about proper crate use to avoid overcrating and other abuses. The crate is so useful, it distresses me to hear that some well-meaning shelter folks have such a low opinion of it. Let’s not throw the puppy out with the bath water!
Pat Miller, CPDT, is WDJ’s Training Editor. She is also author of The Power of Positive Dog Training, and Positive Perspectives: Love Your Dog, Train Your Dog.
The Male Dog’s Reproductive System
by Randy Kidd, DVM, PhD The reproductive system has what seems to be a relatively simple task: to provide the mechanisms necessary to maintain survival of the species. However, the mechanisms involved are complex, and maintaining a functional balance of the hormonal, mechanical, and physiological requirements for reproductive success can be difficult at best. What’s more, while dogs (and for that matter, all animals) are hard-wired to maintain reproductive viability at all costs, very small alterations in the balance of any one of the functions involved with reproduction can produce profound results throughout the body. This month, we’ll examine the male reproductive anatomy and physiology, and deal with the female next month. Anatomy The scrotum is the pouch of lightly haired skin that contains the paired testes and their attached epididymides. The testes are the functional units that generate the production of sperm; they also contain cells that produce a variety of hormones. The reproductive “plumbing” begins with the seminiferous tubules, which coil throughout the interstitial tissues of the testes. Each seminiferous tubule empties into an epididymis, which, in turn, empties into a vas deferens, which in turn opens into the urethra. The primary function of the testes is to produce the male gametes or sperma-tozoa; this process is termed spermatogenesis and takes from 55 to 70 days in the dog. The exact timing of testicular descent into the scrotum has not been established, likely due to the small size of neonates, the softness of immature testes, and the tendency of the cremaster muscle to hold immature gonads in the inguinal region. In one study of Beagles and mixed-breed dogs, the testicles were in their final scrotal position at seven weeks of age. In another study (of German Short-Haired Pointers) there was a correlation between the time of passage of testes through the inguinal canal and completion of deciduous dentition – they both occurred at about 30 to 35 days of age. Unilateral or bilateral cryptorchidism results if one or both testes remain within the abdomen after closure of the inguinal canal. The penis develops from the same embryologic tissue as does the female’s clitoris, and the testes are derived from the embryologic tissue that produces the female ovaries. Development into male or female depends on the presence of the Y chromosome, which fosters the production of testosterone, thus promoting the development of the male sexual characteristics. In the male canine embryo, the mesenchymal tissue inside the glans penis ossifies to form a bony os penis. The penis of the adult dog is composed of the proximal body and the distal glans penis, which includes the bulbus glandis and the pars longa glandis. The bulbus glandis is a cavernous expansion of the corpus cavernosum urethrae. It surrounds the proximal portion of the os penis, and when it fills with blood during erection, it expands into a bulb-like structure that is held within the female’s vagina during copulation. Disorders of the male canine reproductive system There are several disorders of the canine male reproductive tract that deserve mention. They can be categorized into congenital defects, acquired disorders, neoplasias, and functional disorders. Congenital defects of the penis are relatively rare, but include the following: • Penile hypoplasia (incomplete or underdevelopment), usually due to aberrations of the XY chromosomes. • Hypospadia, a defect that results in an abnormal location of the urethral orifice. • Persistent penile frenulum. Normal separation of the glans penis from preputial epithelial cells occurs before birth. If it doesn’t, a tag of skin that restricts movement may cause the penis to deviate. • Congenital preputial stenosis (a narrowing of a duct or canal) often occurs with concurrent phimosis (entrapment of the penis within the prepuce). Cryptorchidism is a congenital condition in which the testes fail to descend into the scrotum. The condition may be bilateral or unilateral (75 percent of the cases are unilateral). It is considered the most common reproductive disorder in dogs, affecting between 1 to 15 percent of dogs, and it is inherited as a sex-limited autosomal recessive trait. Since cryptorchid testes have a much greater risk (6- to 13-fold) for developing Sertoli cell tumors compared to normal testes, and since the trait is inherited, bilateral castration is recommended, even in cases of unilateral cryptorchidism. Acquired disorders include: • Injury/contusion to either the penis or testicles, perhaps as a result of fighting or failure to jump cleanly over a fence. • Fracture of the os penis, again from trauma or as a result of a breeding accident. • Balanoposthitis, inflammation of the glans penis and prepuce, generally from a bacterial infection. • Paraphimosis, a failure of the glans penis to retract normally into the prepuce. • Inflammation or infection of the testes is termed orchitis; epididymitis or inflammation of the epididymis may also occur. Either of these can be caused by any number of bacteria. Of particular interest is brucellosis, an infection that causes resorption of the fetuses early in gestation or sudden abortion during the last trimester of pregnancy. Caused by the Brucella canis organism (or occasionally by B. abortus, B. suis, or B. melitensis), it is a highly contagious disease that can spread rapidly through a kennel by contact with infected fetuses, vaginal discharge, or occasionally by venereal means. Infected male dogs may develop generalized swellings of the lymph nodes, and they frequently show signs of a painful orchitis, epididymitis, or prostatitis. Neoplasias of the penis run the gamut of common types of tumors seen at other body sites, and, except for transmissible venereal tumors (TVTs), they usually occur in older dogs, beginning at around 10 years of age or older. TVTs generally occur in younger dogs since they are transmitted at coitus. TVTs grow, invade, and metastasize most widely in an immune-compromised individual, so immune-supportive therapy is indicated as a part of any holistic protocol for treating them. Tumors of the canine testes are the second most common neoplasm affecting the male dog, representing about 5 to 15 percent of diagnosed tumors. Tumors may develop in any of the tissue types that occur in the testes, but the most common tumors involve the germ cells (seminomas) and tumors of the Leydig and Sertoli cells. Dogs with undescended testicles (cryptorchid) are much more likely to develop testicular tumors, specifically Sertoli cell tumors and seminomas, than are normal dogs. Testicular tumors may be asymptomatic; many occur as a difficult-to-palpate, discrete mass within the testis. Most do not grow rapidly nor metastasize to other body sites. Some (slightly more than half of all) Sertoli cell tumors result in a feminization syndrome as a result of the production of estrogenic steroids by the tumor tissue. The feminization syndrome may cause significant dermatologic changes such as hair loss without itching and hyperpigmentation; behavior changes may also be noted. Seminomas may be associated with other clinical problems such as prostate disease, alopecia, perineal hernia, and other tumors (especially perianal gland adenomas). Prostatic tumors include adenomas, which are generally benign, and adenocarcinomas, which can be quite difficult to treat since they tend to metastasize to other tissues rapidly and because complete surgical excision is rarely possible. Tumors are treated via Western medicine by the usual means: surgical excision, and/or some form of chemo- or radiation-therapy. Alternative therapies for tumors of any type include homeopathy or acupuncture; nutritional supplements and herbal remedies may be included to support the primary therapy of choice. Functional disorders Failure to achieve an erection is a fairly common functional disorder of the male dog. Reasons for this condition include: • The female is not at the receptive stage of heat (this is the most common cause). • Pain (from prostatitis, for example, or arthritis or other conditions of the hips, legs, or lower back), which prevents mounting of the female. • Fear/anxiety about the female or the breeding environment. • Drugs that have anti-androgen activity – for example, ketaconazole, a commonly used drug for treating fungal infections. • Priapism, which is a persistent erection in the absence of sexual stimulus, is occasionally seen in dogs with spinal lesions. Rarely, it occurs due to thrombo-embolism of penile vasculature. This condition differs from the frequent erections seen in young excitable small breed dogs, which respond to behavioral modification, castration, and/or progestin therapy. Prostate problems The prostate, an accessory sex gland in the male dog, is located just caudal to the bladder in the area of the bladder neck and proximal urethra. It encircles the urethra and has several ducts that enter the urethra throughout its circumference. It produces prostatic fluid, which acts as a transport and support medium for sperm during ejaculation. The prostate increases in weight with age until it reaches its normal size; it then stabilizes through adulthood until it begins to grow again in aged animals. However, if the dog is castrated before sexual maturity, normal growth of the prostate is completely inhibited. If the dog is castrated as an adult, the gland will decrease in size to about 20 percent of its normal adult size. Some practitioners refer to age-related prostatic weight increase as benign prostatic hyperplasia (BPH), a condition commonly seen in aged humans. In contrast to human males, however, the uncastrated dog’s prostatic enlargement usually does not cause dysuria (difficulty in urination) due to urethral obstruction; the dog’s prostrate tends to enlarge outward, away from the urethra. Treatment may be required only if the enlarged prostate causes abnormal signs such as dysuria or straining when defecating. Other diseases of the prostate are fairly common, especially in the older dog, and may lead to fertility problems. In the aging dog, fluid cysts may develop in association with age-related hyperplasia. Urinary incontinence True incontinence (involuntary urine leakage) must be differentiated from behavioral urinary issues such as lack of housetraining, submissive urination, territorial marking, or senile loss of housetraining due to canine cognitive dysfunction. There are several causes of incontinence, including excessive water consumption; infection of the urinary tract or bladder stones (either of which can cause irritation and stimulate the “need to pee” feeling); spinal cord irritation; weak bladder sphincter; and several diseases, including diabetes mellitus and diabetes insipidus, Cushings syndrome, and kidney failure. Western medicine treatments have included hormone therapy, alpha-adrenergic agonists, anticholinergics, and surgery. All of these except the anticholinergics work by attempting to restore neuromuscular control and tone to the bladder sphincter. The anticholinergics work by relaxing the bladder’s muscle fibers, thus facilitating urine storage. All of these treatments (with the excep-tion of surgery, which has not been very successful without additional medications) have proven to be fairly effective. The problem is, all the medications listed above may cause severe side effects, and some have been removed from the market. Both phenylpropanolamine, the popular alpha-adrenergic agent, and diethylstilbestrol (an estrogen), are now available from special pharmacy compounding outlets. My choice for treating urinary incontinence is to first of all perform a chiropractic evaluation and adjustment if indicated. Many patients respond to this initial treatment, and periodic adjustments seem to keep their spinal cord fit enough to allow for urine retention. If indicated, I also add acupuncture treatments for their ability to help enhance the balance of hormones throughout the body, as well as for their ability to treat spinal or other inflammatory conditions that might exist. There are also several herbal remedies that have been especially developed to help with treatment of this condition, and in my mind the idea of treating all castrated individuals with herbs that contain steroidal precursors warrants further study. In any event, only after I’ve tried all the alternatives am I tempted to resort to Western medicine drugs. Fertility evaluation There are several ways to evaluate the functional capacity or breeding soundness of the male dog, including observation of sexual behavior (libido), general health, soundness of rear quarters, spermatogenic capacity, and functional evaluations of other, associated organ systems. Daily spermatozoa production is highly correlated with testicular weight and this latter highly correlated with scrotal width. Scrotal widths are measured with calipers. The ejaculate should be evaluated for sperm count, motility, and morphology. Frequency of ejaculate does not affect daily sperm production, but it depletes the sperm reserves contained in the epididymis. Thus, when high sperm concentrations are desired (for example, when sperm are being collected for preservation), the number of sperm is maximized by having the dog ejaculate only at four- to five-day intervals. Healthy animals have a high percentage of sperm that are actively and rapidly swimming in a freshly collected sample. Sperm morphology is evaluated by staining the cells and observing them under a microscope. Stained slides may also reveal the abnormal presence of high numbers of bacteria, white blood cells, or red blood cells. At least 75 percent of the sperm cells should be morphologically normal. Sometimes, fertility evaluations include an examination of the bacteria that resides in the prepuce and distal penile urethra of the male. However, even perfectly healthy and fertile dogs have a normal population of bacteria in those locations. There are often at least three or four different species of bacteria found. On the other hand, some studies indicate that a high bacterial count, especially if there are high numbers of gram negative bacteria along with large numbers of white blood cells, indicates infection. If total numbers of bacteria are high, rule out infection as a potential cause of infertility. Outside factors Poor thyroid function is known to adversely affect libido and breeding soundness in animals, and other organ systems will likely be shown in the future to have intimate connections to the reproductive system. A complete breeding soundness exam will certainly include an evaluation of thyroid function, and an evaluation of other organ systems may also be indicated. Recently, there has been much to-do about estrogenic factors in the environment – airborne “sexual toxins” such as pesticides, herbicides, and manufacturing by-products of plastic production. This news is worth following. Some final breeding hints: • Be certain the dog has reached puberty. • The dog’s libido and efficiency will increase with age and experience – at least, until the onset of old age problems. • Be certain that the female is truly in standing heat. To be sure, use a combination of hormonal, cytological, endoscopic, and behavioral evaluations for the female. • Wherever possible, stay out of the way and let nature take its course. The second most common cause of breeding failure is well-meaning folks who feel the need to interfere and thus disrupt the “ambiance” necessary for good reproductive contact. • Realize that sometimes the mating was simply not meant to be. Sometimes, for whatever the reason, the couple may not be attracted to each other, and they may never be able to “hit it off.” Alternative treatments I think acupuncture and chiropractic are essential when treating at least two conditions of the reproductive system: incontinence and breeding soundness. I’ve had very good results in some (but certainly not all) cases of urinary incontinence using chiropractic adjustments alone or in combination with acupuncture. The typical animal who will benefit from chiropractic adjustments will have a palpable subluxation somewhere between T-12 and L-3. Acupuncture and chiropractic have also cured many an animal from “infertility” that was caused by pain in their hindquarters. Acupuncture has been shown to enhance sperm production, libido, and overall vitality. Herbal remedies offer a good alternative way to treat bacterial infections. Antibiotic herbs such as goldenseal (Hydrastis canadensis) and Oregon grape root (Berberis aquifolium), and immune-stimulating herbs such as echinacea (Echinacea spp.) apply here. In addition, I think it is healthy to support male hormone production after an animal is castrated, even though I realize this is controversial. The major controversy seems to be that the phyto-hormones are not actually hormones, but rather, precursors to hormones. Those stuck on a biochemical paradigm say that only preordained amounts of the biochemical will be effective. I happen to like the herbal remedies because they are precursors of the steroidal hormones; I like the idea that the animal’s body can select the precursor it needs along with the amount it needs. To my way of thinking, this way of supplying a hormone has the best chance for being applied in a healthy manner by the dog’s own systems, and it has the least chance to interfere with the intricate feedback methods already in place in the body. Some plants that provide anabolic steroidal precursors include wild yam (Dioscorea villosa), sarsaparilla (Smilax officinalis), licorice root (Glycyrrhiza glabra), damiana (Turnera aphrodisiaca), and saw palmetto (Serenoa serrulata). Check with an herbalist experienced with using herbs for treating animals for proper dosages and delivery methods. Also With This Article Click here to view “To Neuter or Not to Neuter Your Dog, That Is the Question” Click here to view “New Reasons to Spay, Neuter” -Dr. Randy Kidd earned his DVM degree from Ohio State University and his PhD in Pathology/Clinical Pathology from Kansas State University. A past president of the American Holistic Veterinary Medical Association, he’s author of “Dr. Kidd’s Guide to Herbal Dog Care” and “Dr. Kidd’s Guide to Herbal Cat Care”.
Assistance Dogs
Have you ever watched an assistance dog work? On the campus of the Virginia university where I attended graduate school, I often crossed paths with a student who used a wheelchair, accompanied by her assistance dog, a lovely Golden Retriever. They went to classes, visited the snack bars and cafeteria, hung out in the student lounges, and hoofed it all around campus together.
The assistance dog opened doors, picked up dropped items, pressed elevator buttons, and accompanied her owner everywhere. When you approached her owner, the dog looked confidently and calmly right into your eyes. She was the kind of take-anywhere canine companion that any dog lover would be proud to call her own.

What, I wondered, could this assistance dog and her trainers, teach family dogs and their owners about the secrets of her success? How did she become such a solid, confident, and reliable companion? Can ordinary people obtain a go-anywhere canine companion with the steadiness and confident demeanor of an assistance dog? Assistance dog trainers were happy to help me find the answers.
According to Brian Jennings, staff trainer for the Massachusetts-based National Education for Assistance Dog Services (NEADS), creating a great dog takes lots of time and planning.
A compatible candidate
Bringing home the right dog, assistance dog trainers say, makes the task of developing a friendly and reliable canine companion a lot easier. The goal is to seek a type of dog that tends to be constitutionally suited to the sort of environment in which it will be expected to live and work, and to find an individual dog who seems to exhibit the temperament and personality of a dog who will likely enjoy his new home and job.
For assistance dog work, Jennings and NEADS executive director Sheila O’Brien define what kind of dog they look for in each type of assistance dog:
• Service dogs help people with impaired mobility, including those in wheelchairs. Labs and Golden Retrievers whose calm and confident temperaments fit their job requirements often fill this role.
• Guide dogs assist the sight-impaired. More assertive Labs, Goldens, and German Shepherds excel in this mission, where more independent decision-making is required of the dog, who may have to refuse an owner’s command for safety reasons.
• Hearing dogs help the hearing-impaired by recognizing specific sounds, investigating and locating the source of sounds, and alerting their owners to the presence of the sounds. NEADS selects feisty, inquisitive, and persistent mixed-breed dogs, many with terrier or herding breeds in their heritage, for this high-energy work. O’Brien refers to these dogs as “self-made men and women . . . who need a job,” and often selects these dogs as adults from shelters. These dogs take initiative.
• Therapy or social dogs are often released from specific assistance dog programs, but go to live in nursing homes or with families with emotionally disturbed children, acting as facilitators for social interaction and therapy. The best candidates are exceedingly friendly dogs who thrive on lots of physical contact and affection from people, and are temperamentally “sturdy” enough to disregard a bit of strange behavior from the people they meet. These dogs can be from any sort of background – purebred or mutts.
Choosing your family dog
Imagine that you are an assistance dog trainer looking for a dog who will be as perfectly suited as possible to live with a certain family – your family. Think about what your family is like, and what traits a dog should have to succeed in his new job as your family’s dog.
For example, if you’re looking for a dog whose primary “job” will be to provide company for your elderly and not-very-mobile mother, you’ll want to consider types of dogs that don’t require a lot of exercise to be happy or calm, and who thrive on a close relationship with a person. There are a number of breeds, small and large, that excel as affectionate lap-dogs.
If your household is chaotic, with rowdy, active kids running in and out, you should look for a confident, gregarious dog who will cheerfully accept any and all visitors to your home and handle spontaneous eruptions of activity with aplomb. In contrast, dogs who tend to be nervous, sound-sensitive, or shy will have an uphill struggle to simply survive in your home.
In addition to understanding what traits you want in your new dog, you need to know what characteristics you definitely don’t want. If you have cats, birds, rabbits, or other small pets in your home, you definitely don’t want a breed whose predatory (or hunting) instincts are legendary. If your heart’s desire is a dog who will hike with you in the woods unleashed, steer away from scenthounds or sighthounds, whose talents may propel them toward new adventures, but not always with you.
If you are not familiar with the traits commonly associated with certain breeds or breed-mixes, do some homework. Attend a breed show and talk to as many breeders as you can about their dogs’ common personality traits. Tell them about your family and ask if they’d recommend one of their dogs for your household. Responsible breeders won’t hesitate to warn you away from a breed that is unsuited to your life-style; puppy mill-type breeders, of course, will place their puppies in any paying home.
Check out a breed book at your local library and pay attention to the part about the breed profiles that discuss the dogs’ activity levels, propensity for barking or predation, and reputation for trainability. Cross-breeds and mixed-breeds may display traits from all the contributors to their ancestry.
Once you decide on a breed – or if you prefer a mixed-breed dog from a shelter (and good for you!) – look for an individual who has a temperament that suits your family, too. Not all representatives of a certain breed will have equal doses of the breed’s hallmark temperament.
Lydia Wade-Driver, executive director and founder of Virginia’s Blue Ridge Assistance Dogs, says that a few simple interactions with a puppy or adult dog can provide clues about his temperament and personality. Does the dog approach you willingly? Does he enjoy being touched? Does he startle easily? Does he recover quickly after a scary moment? Does he respond to treats and toys? Watch for confidence without aggression, then, “It’s the whole package and a gut feeling,” says Wade-Driver, “That’s what I go by.”
Socialization is critical
Selecting for certain characteristics is only the first step to improving the odds of raising a great family dog. Developing that great dog’s potential after it has joined your family is where the rubber meets the road.
Assistance dog trainers often disagree about the best techniques for training, but the one thing most dog trainers do agree on is this: intense, well-managed socialization is the most important factor in developing a great dog, whether it’s a family pet or an assistance dog.
“Socialization definitely outweighs obedience,” states Kali Kosch, director of training for Assistance Dogs of America in Swanton, Ohio. “I’d rather have a dog who’s very well socialized than one who’s very well obedience-trained. You can do all of the obedience training in the world but, if you have a dog who’s afraid, you’re at a loss,” she says.

Even though the term “socialization” generally implies some interactions with other individuals, a big part of socializing the dog actually has to do with exposing him to inanimate objects and various environments. Assistance dogs are exposed to every mode of transportation imaginable, including cars, buses, airplanes, trains, moving sidewalks, elevators, and escalators. They are taken to noisy stadiums, quiet libraries, busy fairgrounds, deserted parks, industrial areas, and farms. The idea is to expose them to every sort of environment they might ever find themselves in – in a calm, safe manner.
It’s a big job, though, getting your dog out and exposed to a wide variety of people, places, and things. “I try to present the enormity of it to dog owners in a way that doesn’t feel that enormous,” says Elsa Larsen, president of My Wonderful Dog, a service dog training center in Portland, Maine. Larsen utilizes short, daily socialization and training sessions of two to three minutes each, a program most families can emulate.
“You can get a lot into two to three minutes,” says Larsen. Adding up the small increments of training time over the weeks and months makes the job appear larger than life, so she focuses on “eating the elephant” one piece at a time.
Larsen encourages owners to get their dogs out in public regularly, but to carefully manage the process. Proper socialization is not a free-for-all, she says.
Careful management
Jennings starts taking young puppies and adult shelter dogs to “easy places” to meet “easy people.” She defines easy places as quiet locations without crowds, such as banks, libraries, and malls in the morning. Easy people are sympathetic individuals who resemble the assistance dog trainers, or, for pet dogs, people who resemble family members.
The important part is to carefully observe the dog’s reaction to her experiences and environment, and adjust the process accordingly. Watch her body language for signs of stress such as tucking her tail, licking her lips, shaking, withdrawing, yawning, or losing focus. A little dog may respond with a fast heart rate – easy to detect if you are holding her. Start with short visits of no more than two to three minutes each.
Stop when the dog shows any indication of “too much too soon,” but don’t go home yet. Just return to a place where the dog felt comfortable, and allow the dog to regain her composure. Ask for one more “easy” interaction. Then go home. Jennings refers to this process as “habituating” a dog to different environments slowly and carefully, a critical step that family dog owners often neglect.
For instance, if your dog was fine when meeting adults outside the bank, but became agitated when children approached her, give her a quiet moment to rest, then encourage her to meet with a friendly adult or two, then stop for the day. This approach teaches the dog that exhibiting fearful or avoidance behaviors will not release her from a situation completely, but that she will have the opportunity to collect herself before continuing. Of course, lots of treats to reinforce steadiness are the order of the day.
Solid socialization arises from positive exposures to people, places, and other animals. “Negative socialization can do more damage than good,” claims Kosch. The dogs learn to feel safe in lots of places, but planning and constantly adjusting the pace of the program to fit the dog are the keys.
After a couple of weeks, the trainers graduate their dogs to “hard places” and “hard people.” Hard places include supermarket parking lots, city streets, and pet supply shops. Hard people are unlike any the dog has ever met before, and can include boisterous, active children; large, gruff men; heavily perfumed women; or the elderly. Repeat the process. Watch for signs of stress, and back up to the last point of success, if necessary. End on a positive note, with lots of treats. In about 15 trips, Jennings’ dogs show confidence, even in moderately hard places and for more than a few moments.
Most family dogs don’t receive this amount of managed socialization, with a concentration on positive-only experiences at a pace adjusted for the dog. Kosch reminds dog owners that it’s the quality of the socialization, not just the socialization, that’s important. Jennings adds, “Doing it right is a whole lot more important than doing it a lot.”
Focus on you
One of the most noticeable qualities of good assistance dogs is their focus on their handlers, even in strange places. Family trainers can get the same attention from their dogs by using a few simple training techniques.
For instance, Ann Hogg, staff trainer at the St. Francis of Assisi Service Dog Foundation in southwestern Virginia, teaches dogs to make eye contact and sit as a way of asking for permission to interact with a stranger or to get his dinner bowl. All good things originate from an interaction with the handler.
Fully integrated in the family
Another reason that assistance dogs seem to be so bonded with their handlers is because they spend literally their entire days and nights with their handlers. Completely integrating the assistance dog into the daily life of his adoptive handler allows the person to incorporate training into almost every hour of the dog’s daily life.
Both Hogg and St. Francis training director Karen Hough agree that the effectiveness of the training, however, relies on consistency among all members of the dog’s household. Hogg prepares a “vocabulary list” of training words to use with an assistance puppy, which she tapes on her refrigerator door. All of her family members use this specific vocabulary when they interact with the dog.
Hough is never without a treat in the presence of her assistance dog trainees and doesn’t worry about fading out the treats over time. According to Larsen, treats are the one constant in an assistance dog’s life, as he moves from breeder to puppy raiser to skills trainer to owner.
Time commitment
How much time does it take to perform all of this managed socialization and consistent training? Well, it depends how you look at it. At 3 to 5 minutes, a couple of times a day during early training, then adding 15 to 20 minutes a day when obedience and skills training begins, the commitment sounds reasonable, even for busy families.
However, Kosch warns against underestimating the time involved in raising a well-socialized dog, not only for teaching lessons, but also for planning the training program and monitoring its status. According to Larsen, it takes about 20 months to socialize and train an assistance dog. After the dog is placed with his new owner, it takes another year of work to develop into a close-knit, working team – a sizeable investment, to be sure, starting from day one.
Trainers encourage owners to watch their dogs throughout the day. If you do this, your time with your dog will be filled with on-the-spot training opportunities.
Lorie Long is a freelance writer and agility competitor from Virginia.
The Anatomy of the Canine Kidney
by Randy Kidd, DVM, PhD Put simply, the function of the kidneys is to make urine, a “waste” product of body metabolism. Of course, there is much more to the kidneys. They are powerful chemical factories that: • Remove waste products, toxins, and drugs from the body • Balance the body’s fluids and help maintain a constant body pH • Release hormones that regulate blood pressure and control the production of red blood cells • Produce an activated form of vitamin D that promotes strong, healthy bones Anatomy and physiology The two kidneys lie against the back abdominal wall, lateral to the spine, in the lumbar region. They are encapsulated organs, shaped somewhat like a kidney bean, and their size varies with the size of the dog. The functional unit of the kidney is the nephron. There are perhaps a million nephrons in each kidney, each one comprised of a glomerulus and a long tubule that eventually empties into the ureter.
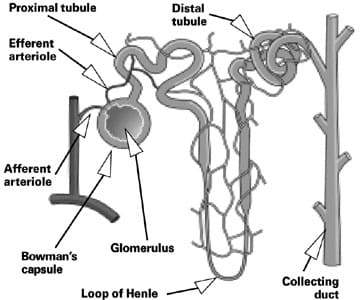
The glomerulus is a congregation of blood vessels contained within Bowman’s capsule, and the glomeruli are located in the outer portion of each kidney (cortex). Blood is filtered as it passes through the kidney’s collection of glomeruli. After filtration in the glomeruli, the resulting protein-free fluid is passed into a thin tubule. The proximal tubule descends into the med-ulla of the kidney and then makes a sharp U-turn (at the loop of Henle) to return into the cortex, where it empties into a collecting duct, even-tually exiting via the ureter. The tubules are responsible for secretion of some substances (such as drugs and their by-products, uric acid, fatty acids, and bile salts) and reabsorption of a variety of other permeable solutes, among them glucose, amino acids, vitamins, minerals, urea, and some salts, notably sodium, chloride, and potassium. Urine passes into the bladder where it’s stored until it’s excreted via the urethra. Blood pressure is controlled by a complex interplay of hormones. In response to decreased blood pressure (as a consequence of chronic congestive heart failure or CHF, for example) the kidneys release renin. This is a proteolytic enzyme that acts on liver-produced angiotensinogen, which is converted to angiotensin I and then to angiotensin II. Angiotensin II causes retention of sodium and water, in part through stimulation of the synthesis and release of aldosterone by the adrenal cortex. Angiotensin II also causes vasoconstriction, thus increasing vascular resistance. Vasoconstriction and water retention place further stress on the already compromised heart muscles, and ultimately these conditions may also damage the kidney’s nephrons. Thus, angiotensin-converting enzyme (ACE) inhibitors are widely used in treating CHF in dogs, and many practitioners include them for the treatment of kidney disease. The maintenance of the body’s overall acid/base balance also relies on a complex mechanism that depends on adequate respiratory and digestive function as well as kidney mechanisms. The kidney’s role in keeping the body’s pH within a healthy range is related to balancing the potassium and hydrogen ion retention and depletion and is especially important during hypoxia (when the animal is not receiving enough oxygen, either from poor respiratory function and/or a diminished supply of red blood cells). The kidney is both the sensor organ and the major site for the production of erythropoietin, the hormone that regulates production of red blood cells. Chronic renal failure is thus typically accompanied with a mild to moderate anemia. Bone health is reliant upon healthy kidneys in at least two ways. First, vitamin D is necessary for the utilization of calcium, and the activated form of vitamin D is produced in the kidney. Second, normal kidneys excrete phosphorous; chronic renal failure may lead to excessive retention of phosphorous, which in turn causes an imbalance between calcium and phosphorous. Vitamin D must be metabolically activated (via hydroxylation in the liver and kidney) before it can function physiologically; the conversion in the kidneys is the rate-limiting step in vitamin D metabolism. Occasionally the imbalance of calcium to phosphorous seen with increased retention of phosphorous may create a decreased amount of circulating calcium. Parathyroid gland hyperplasia occurs (to maintain serum calcium in normal ranges), and the resultant high parathyroid hormone (PTH) concentrations result in increased bone resorption, which ultimately creates thinning of the bone. Note here that the major contributor to the softening of the bones is an imbalance between calcium and phosphorous levels in the body. Rarely, the opposite of the above condition (hypercalcemia) occurs with renal disease, but the pathogenesis of this condition is unknown. Note also that calcium metabolism is involved with bladder and kidney stone formation, which often makes for complicated therapeutic decisions whenever we need to treat kidney disease. Notes about renal disease Renal disease refers to the presence of morphologic or functional lesions in one or both kidneys, regardless of extent. Renal failure refers to the retention of nitrogenous waste products of protein metabolism, regardless of the cause. Renal insufficiency is a term that has been used to describe a state of reduced renal function that has not yet resulted in retention of nitrogenous waste products. Azotemia (from the Greek azote, meaning “nitrogen”) is defined as an excess of urea or other nitrogenous compounds in the blood. You may also hear the term “uremia” used to replace azotemia, but uremia has now come to refer to the entire constellation of signs and symptoms of chronic renal failure: nausea, vomiting, anorexia, uremic odor of breath, pruritus (itchy skin), neuromuscular disorders, pain and twitching of muscles, hypertension, edema, mental confusion, and acid-base and electrolyte imbalances. Typical causes of azotemia are classified by their location: prerenal, from diminished blood flow into the kidneys; post-renal, usually due to a blockage of the “outflow vessels” (ureters or urethra); and renal disease that can be caused by a lack of proper function of any of the components of the nephron (the glomerulus or tubules), or it can be caused by conditions affecting the tissues between nephrons. Finally, to help determine treatment, practitioners also like to know if the disease is acute or chronic, and if it appears to be progressive or nonprogressive. Diagnosis of urinary disease Noticeable symptoms and signs of urinary system disease will, of course, vary with the disease and its severity, but the following general symptoms should make you suspicious of urinary system disease. Dysuria, that is, any abnormality of urination, including polyuria (passage of large amounts of urine in a given period), may be the animal’s attempt to compensate for diminished functional capacity of the kidneys, and it is often associated with polydipsia or chronic excessive thirst. Hematuria indicates the presence of blood in the urine and may be due to renal calculi, trauma, or destruction of the red blood cells within the body (this latter condition is more correctly referred to as hemoglobinuria). Oliguria (from the Greek oligos, meaning little or few) describes the secretion of a diminished amount of urine in relation to the fluid intake, and stranguria (from the Greek stranx, meaning “drop”) describes slow and painful discharge of urine, due to spasms of the urethra and bladder. Anuria is defined as the complete suppression of urinary secretion by the kidneys. It is an emergency condition whenever urine flow has ceased, whether due to kidney shut down (shock, for example) or blockage of the outflow vessels of the urinary tract (stones). See your veterinarian immediately. If renal disease proceeds to chronic renal failure, uremia results, and (as mentioned above) uremia produces an entire constellation of signs and symptoms. Other symptoms, seemingly unrelated to the kidneys, may occur with chronic renal failure: pulmonary edema and coughing, bone conditions related to softening of the boney mass, heart conditions related to improper control of blood pressure, and symptoms related to anemia such as difficulty breathing, exercise intolerance, restlessness, etc. Symptoms, even those that become evident when specific diagnostic aids such as urinalysis and blood chemistries are employed, may not occur until a very high percentage of the nephrons are not functioning properly. Perhaps as many as 70 percent or more may need to be dysfunctional before specific symptoms are detected. Urinalysis The primary diagnostic aid for kidney disease, a typical urinalysis includes the urine’s specific gravity, its pH, and the presence of abnormal amounts of substances such as protein, glucose, and creatinine. Important findings in the urinary sediment include red or white blood cells, crystals, bacteria, or other organisms such as yeasts. A functional kidney is able to concentrate (or dilute) urine to a specific gravity that is different from that of the blood plasma (circulating blood plasma has a specific gravity of 1.010 + 2); kidney disease is diagnosed when the urine specific gravity remains at 1.010 + 2, regardless of the dog’s state of hydration. Normal pH of the carnivorous animal’s urine is acid (below pH of 7), and it typically becomes more basic with bacterial infections. The consistent presence of glucose in the urine (glucosuria) indicates the likelihood of diabetes mellitus. The presence of cells or microorganisms in the sediment are indicators of infection or inflammation. Moderate amounts of protein in the urine signify that there is a “leak” in the glomerular filtration system, that the kidneys are unable to retain proteins in the bloodstream. See “Urine Luck” (February 2004) for more information on urinalysis. Blood tests Blood chemistry tests can also help diagnose some urine system dysfunctions. Renal excretion of urea is accomplished by glomerular filtration. Urea is also reabsorbed passively in the renal tubules, which means that its blood levels will increase whenever there are slower tubular flow rates – during dehydration or blood volume depletion, for example. So, one important result of the blood chemistry test examines the blood urea nitrogen (BUN) levels. Creatinine, a product of the normal metabolism of muscles, is excreted by the kidneys by glomerular filtration. Non-renal variables, such as excessive muscular activity, muscle necrosis, and possibly ingestion of a meal of cooked meats, may have a small and transient effect on the blood creatinine level, but it is still considered a good indicator for glomerular function. Creatinine and BUN assays offer an indirect measurement of the glomerular filtration rate (GFR), which in turn is a good assessment for the overall functional capacity of the glomeruli. Phosphorous retention results from declining function of the glomerulus, and blood phosphorous levels may be extremely high with chronic renal disease. Blood albumin levels may also be low due to inadequate retention of proteins, and the decreased levels of protein may lead to edema and/or malnourishment. A mild anemia often occurs with severe kidney disease (due to improper production of erythropoietin). Elevated white cell counts may point to infections in the urinary tract. A complete blood count (CBC) can help detect these conditions. Other diagnostic tests include abdominal X-rays, contrast studies of the urinary tract, ultrasonic exams of the kidneys and bladder, and renal biopsy. Some diseases (diabetes and CHF in particular) may predispose the dog to renal failure, so tests to rule these out may be needed. See “Passing the Blood Test” (November 2003) for more information on blood chemistry analysis. Prerenal conditions These conditions result from reduced blood flow to the kidneys due to such causes as dehydration, congestive heart failure, or shock. They usually resolve completely with appropriate treatment, but they may also progress to renal disease and renal failure. Renal conditions

Every practitioner will tell you that kidney disease is one of the most common entities seen in vet practices daily. Acute renal failure usually occurs following a major insult to the kidneys. Potential causes include vascular conditions (such as disseminated intravascular coagulation or DIC), immune mediated conditions (such as lupus), renal infections, and ingestion of toxins (such as heavy metals, aminoglycoside antibiotics, painkillers, and ethylene glycol or antifreeze). Once the instigating factor(s) is removed with specific therapy, and supportive therapy is instituted (for example, fluids to enhance flow through the nephrons), the kidney typically returns to its normal function. If the disease process is allowed to proceed for a few days to a few weeks, chronic renal disease may ensue. Chronic renal failure (CRF) presents a far more complex and ever-evolving picture. Therapy often must be adapted to the individual case and its progress over time. Basic principles of therapy include: • Determination of the cause of the disease, if at all possible. • Removal of potential toxins – including drugs that are known to be harmful to the kidneys. • Restoration of blood flow through the glomeruli. Fluids, given sub-Q, IV, or orally if possible, can be life-saving. Some dogs with CRF can manage a fairly good quality of life so long as fluids are administered on a routine basis – daily or several times a week. • Dietary changes to help bring the body and the urinary system back into balance (see nutrition, below). • Specific treatments to help counter the cause of the disease. Infections, for example, can be treated with antibiotics, herbs, acupuncture, or immune system-enhancing methods. Primary glomerulopathies are uncommon in dogs. They are often due to an immune-mediated disease that ultimately creates the formation of immune complexes in the glomerular capillary wall. These immune complexes prevent normal glomerular functioning, and the dog is unable to retain protein. The primary symptoms are frequently due to the protein loss: weight loss, edema or ascites, dyspnea (difficulty breathing, due to pleural effusions or pulmonary edema), coagulation disorders, and proteinuria. Severe cases can result in renal failure and uremia. Drugs are a prevalent cause of renal disease, and there are many that have been implicated. Aminoglycoside antibiotics are the second most common cause of acute renal disease in dogs (behind only antifreeze toxicity), and the frequency of toxicities seems to be increasing every year. Although their spectrum of toxic severity varies, all antibiotics in the aminoglycoside classification are nephrotoxic. Aminoglycoside antibiotics include neomycin, kanamycin, gentamicin, amikacin, and streptomycin. Many painkillers (including nonsteroidal anti-inflammatory drugs or NSAIDs), chemotherapy agents, and many other drugs have been reported to be nephrotoxic. Some herbs have also been cited as potentially nephrotoxic, including wormwood (Artemisia absinthium); sassafras (Sassafras albidium); horse chestnut (Aesculus hippocastanum); chaparral (Larrea spp.); and periwinkle (Vinca minor). Bottom line: Ask about the potential renal toxicities for any drug or therapy your practitioner recommends. Postrenal conditions There are several potential causes of partial or complete obstruction of the outflow vessels of the urinary tract, including tumors, enlarged prostate in the male dog, trauma that causes blood clots or eventual scarring, and uroliths or stones. Of these, stones are the most common. Generalized symptoms of constriction of the urinary tract include nonproductive straining to urinate, increased frequency of urination (without an increased volume), and blood in the urine. Symptoms may be present for a period, followed by periods of apparently normal function. Uroliths (also known as urinary calculi or stones) are crystalline concretions, found in the urinary tract, that contain mostly inorganic crystalloids, along with a small amount of organic matrix. Almost any mineral substance that passes through the kidneys could form one of these precipitates, and under favorable conditions, a hardened concretion could develop. Stones are named according to the predominate crystal found within. The most common stones found in dogs are struvite and calcium oxalate. Typically, when a dog has uroliths, crystals are seen in urine sediment. Depending on the stone’s size and mineral composition, X-rays can be used for detection; however, some uroliths don’t show up well on X-ray films. Laboratory analysis of the stones is needed to positive identify the minerals they contain. Some breeds are predisposed to forming uroliths, and some breeds are especially prone to forming a specific type of urolith. For example, due to a genetic defect in uric acid metabolism, Dalmatians are predisposed to urate calculi formation. With each type of urolith, there are predisposing factors that tend to precipitate the problem, and each of these factors is specific for the type of urolith formed. For example, oxalate crystals form in acidic urine, struvite crystals tend to form in alkaline urine. Check with your vet for these specifics, to help formulate a plan for treatment and prevention. Symptoms vary with the location and the size of the urolith. They include frequent attempts to urinate, straining or inability to urinate, hematuria, overdistended bladder, or signs of uremia. Uroliths may also be totally or periodically asymptomatic. They often cause secondary irritation and result in infections. Struvite is composed of magnesium ammonium phosphate, in varying ratios and degrees of purity. Struvite uroliths form in alkaline, concentrated urine, and there is a genetic predisposition for their formation. Medical management may be helpful and may even dissolve the stones. A medical protocol would include enhancing urine flow (diuresis along with plenty of water intake), production of acidic urine, and dietary means to reduce magnesium and phosphorous and (perhaps) to reduce protein. (For more on protein, see nutrition section, below.) Calcium oxalate uroliths, in contrast, must be removed surgically, since attempts to dislodge them by nutritional means alone have not proven successful. An acute urinary obstruction is an emergency condition that requires immediate care. Urine backup creates a toxic level of urea in the body which may, within hours, cause neurological signs and eventually lead to death. Your veterinarian may need to use anesthesia to pass a catheter to dislodge the stone(s) for immediate relief. Other urinary tract diseases Infections of the urinary tract include cystitis (infection of the bladder), pyelonephritis (kidney infection), and urethral infections. Infections can be caused by a variety of microorganisms, and they are conventionally treated with antibiotics or alternatively with herbs or other methods. Clinical symptoms include the list of urinary dysfunctions: hematuria, difficulty and increased frequency of urination, etc. Infections are usually easily diagnosed by examining the urine sediment for the presence of bacteria and/or blood cells. Culture and sensitivity can also be performed to determine the antibiotic of choice; herbal remedies typically have a broad range of activity, although their potency may not be quite as strong. While symptoms of urinary infections or obstruction may wax and wane, depending on the degree of obstruction and/or the amount of irritation to the urinary tract, you can often predict an event by observing precursor symptoms such increased attempts to urinate (with poor results), straining to urinate, or blood-stained urine. At the onset of these symptoms, I’ve had excellent results with dandelion root (Taraxacum officinale) and Oregon grape root (Berberis aquifolium), perhaps along with echinacea (Echinacea spp.) to enhance the immune system. Of course, make sure the dog drinks plenty of water and continues to be able to urinate freely. Dandelion acts as a diuretic and Oregon grape root has antibiotic activity; the combination is often enough to ward off further development of disease while we try to correct the problem nutritionally or with other medications. There are two problems of the urinary tract – urinary incontinence and conditions of the prostate – that deserve more discussion, but since they are more related to the reproductive tract, I’ll cover them in the next installation of the Tour of the Dog. The urinary system is also affected with a long list of physical anomalies, many of which have a familial tendency. Included in this list are renal dysplasia and hypoplasia, renal agenesis, polycystic kidneys, renal cysts, and some of the glomerulopathies. Neoplastic diseases also occur along the length of the urinary tract, and their diagnosis and treatment are the same as for neoplasias affecting other sites. Western and other therapies Western medical therapies for treating urinary system diseases are aimed at the following: removing or discontinuing instigating factors (infections, for example, or nephrotoxic drugs); improving hydration so that urine flow through the tract is optimal; providing nutritional support that minimizes stress to the kidney while it helps return the body back to balance; and using specific medications that apply to the ongoing condition of the patient. Alternative medicines can be helpful for treating many of the common conditions that affect the urinary system. Alternative medicines may prove even more beneficial for maintaining a balance of the “extra” functions of the kidney – the functions that help the animal maintain homeostasis. “Alternative” or “holistic” practitioners will try to create the same benefits that their Western colleagues expect, typically by using a more natural approach – with home-prepared foods rather than commercial “prescription” diets, as one example. A holistic practitioner will also likely employ one of the alternative methods to try to re-establish homeostasis. Nutrition will likely be the mainstay for the holistic practitioner treating renal disease. Holistic treatments will vary according to individual patient needs and will likely change as the healing process progresses. Nutrition Nutritional approaches to treating urinary tract diseases are fairly common now, especially since the dog food companies have seen the potential for increased sales. It’s important to remember that each type of urinary tract disease requires an individualized nutritional approach. With this in mind, there are some basics that may help you when you devise a diet for your dog. It is important to maintain fluid flow through the kidney, so the dog’s diet should either be moist or should encourage drinking lots of water. Some diets include salt to enhance thirst, but salt encourages fluid retention, which is not good for the heart. Excess phosphorous may speed the progression of renal conditions. Low-phosphorus diets are difficult to formulate, so most commercial foods contain “phosphorous binders” – substances that contain ingredients that remove phos-phorous from the blood. Some diets or therapeutic regimes use potassium citrate, an alkalizing agent that helps maintain potassium levels in the body and helps with the management of calcium oxalate uroliths. Antioxidants (such as Omega-3 and -6 fatty acids) can speed the repair of renal damage from disease. Vitamins A, C, and E can be used for their antioxidant effects, but these vitamins can affect the pH of the dog’s urine. If your dog has a history of or predisposition to stones, work with your vet to monitor the pH of the dog’s urine when you feed these supplements. B vitamin supplements can be beneficial, especially if diuretics are used to enhance urine flow. One of the most controversial topics in canine nutrition has to do with proteins in the diet of kidney-compromised dogs. Studies have produced conflicting results. In years past, we thought that we helped compromised kidney function by providing a low-protein diet. Not all current research supports this, however. Recent studies indicate that a low-protein diet (less than about 10 percent) may actually be detrimental when treating kidney disease. What seems to be the consensus now is that a diet moderately high in protein (30 to 35 percent), provided in high quality, readily assimilated proteins, is most supportive for long-term care of the kidney-compromised dog. What none of the studies shows is what most interests a holistic practitioner: How much “vitality” is contained in the food. Processed foods have almost no healthy “energy.” Raw, home-prepared foods have the dietary vitality that dogs evolved with, foods that retain their natural capacity to provide overall health and vigor. I have no scientific data to support this, but my guess is that an unprocessed diet that approximates the high protein diet of the wild canine will ultimately prove to be the best one for preventing renal disease. (Editor’s note: WDJ will publish an article on diets for kidney-compromised dogs in a few months.) Herbal therapies The list of herbs that may be helpful for aiding urinary problems is extensive. For starters, many herbs are diuretic, with a range of activity varying from slight to profound. Most conditions of the urinary tract benefit from an increased flow of urine, so almost any herb will be helpful in this regard. Further herbal selection depends on the specific condition – for example, one herb that has been used to treat kidney stones is bearberry or uva-ursi (Arcto-staphylos uva-ursi). My favorite herbal combination for non-specific urinary tract conditions, especially the recurring types that may be related to low grade infections, are dandelion root and Oregon grape root. Go, team! As I consider the various and sundry functions of the urinary system and how to best keep all its aspects healthy and functioning and in accord with other body systems, I can’t help but think that this is a prime example where a team approach may be the most beneficial. To be most effective, we need the diagnostic acumen of Western medicine, the services of a good, holistic dietitian (to help us provide the best balance by using whole foods), and an herbalist who is well informed on potential kidney toxicities as well as the benefits of the herbs. Finally, to provide the most beneficial treatment for a specific kidney disease, there will be occasions when Western medicine is simply more prudent and better than any of the alternatives available. Also With This Article Click here to view “Can Meat Cause Kidney Failure?” Click here to view “A Low-Protein ‘Kidney Diet’ is Not Always The Answer” Click here to view “Chronic Kidney Disease in Dogs” -Dr. Randy Kidd earned his DVM degree from Ohio State University and his PhD in Pathology/Clinical Pathology from Kansas State University. A past president of the American Holistic Veterinary Medical Association, he’s author of Dr. Kidd’s Guide to Herbal Dog Care and Dr. Kidd’s Guide to Herbal Cat Care.
Download the Full April 2005 Issue PDF
Join Whole Dog Journal
Already a member?
Click Here to Sign In | Forgot your password? | Activate Web AccessPets and PETA
by Nancy Kerns
Criticizing an organization that accomplishes good things on behalf of beings with no resources with which to help themselves – why would I want to do that? Actually, I hadn’t meant to – yet.
In the February issue, I mentioned that it had come to my attention that someone in the pet food industry was spreading a rumor that WDJ and People for the Ethical Treatment of Animals (PETA) were somehow in alliance. I have a good hunch that the rumor was being spread maliciously, to try to undermine WDJ’s standing as an independent and reputable voice. I addressed the rumor directly because I wanted to nip it in the bud, fast.
I mentioned that I didn’t know much about PETA, but was aware that the animal rights organization had a poor reputation among dog owners. I offer my sincere apologies; that was a sloppily written statement, and I knew better. I should have said, “among some dog owners.” Because the little bit that I do know about PETA is that there are a number of dog owners who can’t stand the high-profile group.
I know this because I’ve seen many anti-PETA statements posted on dog-related bulletin boards, and heard many critical comments about the PETA at dog-related venues. The criticisms I’ve heard suggested that PETA is anti-pet – that the group is opposed to the practice of owning dogs and every other type of animal. I’ve also seen a number of quotes to this effect attributed to Ingrid Newkirk, PETA’s founder and president.
Since being taken to task for my inaccurate statement by a number of readers who are fans of PETA, I belatedly educated myself about the group’s stance on dog ownership and use of dogs. I found no evidence to support the accusation that PETA is against dog ownership in the organization’s literature on its Web site (www.peta.org).
PETA does, however, disapprove of any and all dog breeding. One of its factsheets (“Companion Animals: Doing What’s Best for Them”) cites a number of sad statistics quantifying the numbers of dogs and cats put to death in U.S. animal shelters each year, and comments, “In light of these tragic statistics, no breeding can be considered ‘responsible.’ ”
It follows that the group is not crazy about conformation dog shows, which promote dogs based on appearance, because breeding has created health problems in many breeds. It is opposed to all tail-docking and ear-cropping.
I’ve heard it alleged that PETA is opposed to all dog training, dog sports, and use of service or working dogs. That’s not currently reflected in its literature, either, although the factsheet referenced above does mention the group’s opposition to dog sports and the use of working dogs when the dogs are treated inhumanely, pushed beyond their natural limits, sent into dangerous situations, and deprived of opportunities to socialize with other dogs.
PETA is opposed to all laboratory testing on animals – which is one place where the group and I disagree. My personal opinion – which is not that of WDJ or its contributors – is that it’s possible for labs to keep and use animals in a humane fashion, and that some lab tests involving animals are valuable and necessary. I would include feeding trials, which I discuss at length in “On Trial” (in this issue), in this category.
PETA has been a part of a movement that has improved living conditions for many animals. I think that’s commendable. Even so, I admit I’m not a fan of the techniques it uses to forward its mission of “establishing and protecting the rights of all animals.”
How about you? Do you think that any means justify the potential end of poor living conditions for lab dogs?
———-
Correction
In the March 2005 issue, we listed an incorrect phone number for Dr. John Symes, who advocates a gluten-free diet for dogs. The correct number is (251) 343-7110. We regret the error and apologize for any inconvenience it may have caused.
Pet Food Company On Trial
[Updated March 4, 2016]
In 2003, People for the Ethical Treatment of Animals (PETA) launched a media campaign aimed at exposing what it characterized as the cruelty, pain, and suffering experienced by dogs and cats that are used in laboratory research studies conducted by pet food companies.
One of the more unfortunate results of this campaign, as far as we’re concerned, is that consumers may have become convinced by PETA’s campaign that two important lab tests – feeding trials and metabolic studies – are inherently cruel. In fact, there is nothing innately cruel about the tests themselves; neither imposes anything more invasive than the removal of a blood sample on the canine test subjects. Also, we believe the tests do benefit the canine population at large. In our opinion, it’s how (and how long) the dogs are kept by the labs that could stand major improvement.

There are all sorts of other laboratory research studies conducted by the larger pet food manufacturers that push the envelope of “humaneness.” Some companies perform (or order a “contract lab” to perform) studies that call for a disease or health problem to be induced in a population of test dogs, such as a damaged kidney or cardiac problem. Then various nutritional approaches to improving the condition are tried. Some of these tests also require euthanasia and postmortem studies of the dogs; feeding trials and metabolic studies do not.
Research conducted to formulate foods that improve health problems has the most potential for inflicting pain and suffering on the test dogs. But it shouldn’t mistaken for what happens in a feeding trial to confirm the nutritional adequacy of a food – which is what this article is about. We’ll save for another day a discussion about the ethics and practice of conducting research that requires the induction of disease and euthanasia of the test subjects.
Definition of a Feeding Trial
It should not come as a surprise that pet food makers use dogs and cats to develop and test their products, and not just in a “He likes it! Hey Mikey!” kind of way. The most common test ordered by dog food makers is the “feeding trial,” a formal test where dogs are fed a certain food and nothing but that food for about six months. Feeding trials are conducted to test and – it is hoped – establish the ability of a food to keep dogs alive and reasonably well. When a food “passes” a feeding trial, its maker earns the legal right to include a statement on the product label assuring consumers that a feeding trial has established the nutritional adequacy of the food.
The “metabolic study” is another increasingly common test used by pet food makers. It requires that a dog spend at least five days in a relatively uncomfortable cage with a slatted metal floor, which allows technicians to collect every bit of the subject’s urine and feces. We’ll describe it in more detail below, but suffice to say it’s a common test, not invasive, but not particularly fun for the dog, either.
Sound like a case for PETA? The high-profile animal rights organization opposes all laboratory testing on animals, so it was perhaps just a matter of time before it trained its sights on the laboratory testing conducted by pet food makers.
However, PETA’s metaphorical weapon isn’t sharpshooter-precise; it tends to be more like a shotgun splatter of allegations of animal cruelty. PETA has taken the pet food industry (with a special concentration on one unlucky company in particular) to task for the all the research it conducts to develop and establish foods. (For more on the PETA campaign, see “Truth Is the First Casualty of War” sidebar.) But again, we’re going to limit our discussion to just two pet food tests that we feel are useful.
“Complete and Balanced”
Go grab a can or bag of your dog’s food, and look for a little bit of fine print that mentions AAFCO – the Association of American Feed Control Officials. The statement tells you what sort of proof the manufacturer used to establish the nutritional adequacy of that product. Pet food makers cannot claim a food is “complete and balanced” unless they can prove this in one of three ways:
• A feeding trial confirms that the food was able to maintain a population of test subjects for a determined period.
• A laboratory analysis confirms the food contains nutrients in amounts established by AAFCO as necessary for either “maintenance,” “growth,” or “gestation and lactation.” If the label claims it meets the AAFCO nutrient profiles for “all life stages,” the food must meet or exceed the requirements of the AAFCO nutrient levels for growth and gestation/lactation.
• A dog food in the same “product family” as a similar, “lead” product that passed a feeding trial may make the same nutritional adequacy statement as the lead product. To qualify as a “family member,” the family and the lead product must be of the same processing type (both are extruded kibble, for example) and contain the same approximate amount of moisture, a similar amount of metabolizable energy (as determined by a metabolic study), and similar amounts and ratios for crude protein, calcium, phosphorus, zinc, lysine, and thiamine (as determined by laboratory analysis).
There are three ways a product can earn its AAFCO statement, but only two different statements found on dog food labels: a “nutrient levels” or a “feeding trial” statement. That’s because AAFCO allows a product that meets the family requirements to use the lead product’s feeding trial claim, even though the family members didn’t pass a feeding trial. To complicate matters, pet food companies don’t (and don’t have to) disclose to consumers which food is the lead product that passed a feeding trial and which foods are the family members.
Feeding trials are considered by most veterinary nutrition experts to be the “gold standard” for proving nutritional adequacy claims – superior to the “nutrient levels” method of proof. That’s because it’s quite possible for a laboratory analysis to confirm that a food contains the amounts of various nutrients judged to be necessary for maintaining a dog, but for the product, in practice, to fail at that very job.
This is possible because not all nutrients may be in a digestible (“bioavailable”) form. Most nutritionists agree that feeding trials offer the most reliable confirmation of a food’s ability to deliver nutrients in a form that will benefit the target species.
AAFCO Feeding Trial Protocols
Of course, to be of comparative value, a feeding trial needs to be standardized, so all products that “passed” a trial can be considered equally adequate. That’s where AAFCO comes in.
Contrary to its official-sounding name, AAFCO is not a regulatory power; it’s an advisory body comprised of state feed control officials (the voting members) as well as representatives from the pet food industry, the Food and Drug Administration (FDA), the United States Department of Agriculture (USDA), and other interested groups.
AAFCO researches and discusses policies that affect the feed industry, and drafts model regulations that feed control officials can bring home to their states for modification and/or adoption. Committees are appointed to study specific topics, such as ingredient definitions, labeling, manufacture, inspection, and enforcement; the committees then bring their analyses to the entire body for review and action. All of the individual American states enact and/or codify most or all of AAFCO’s suggested regulations for the manufacture and sale of animal feeds within their borders.
AAFCO designed the standardized protocols used by pet food makers to test the nutritional adequacy of their products through feeding trials. There are slightly different rules for different trials, depending on the claim the manufacturer wants to make for its product. The possible categories for dogs are:
• Adult maintenance
• Growth (puppy food)
• Gestation/lactation
• All life stages
We’ll examine each of these in detail.
Tried as Adults
For an adult maintenance claim, a minimum of eight healthy adult dogs (at least one year of age) and of optimal body weight are required to start the test. Eight control dogs meeting the same description are required for a control group and are fed a different food. While eight is the minimum number for each group, a minimum of 30 dogs must be monitored to establish values for “colony averages” of weight and blood test results before and after the trial.
Because a minimum of 30 dogs are required to establish the colony averages, the number of dogs used for both the control and the tested food groups are generally more than the minimum of eight. The distribution of different breeds in the two groups should be the same.
The adult maintenance test runs for a minimum of 26 weeks. The test diet is the sole source of nutrition (besides water, which must be provided at all times) for the dogs in the test diet group; the control group is fed a different food, one that has already passed a feeding trial for the same claim.
All the dogs are weighed at the beginning of the test, weekly, and at the end of the test. They also receive a complete physical inspection by a veterinarian before and after the test, and are evaluated as to general health, body, and hair coat condition. After the test, blood is taken from each animal and the results for hemoglobin, packed cell volume, serum alkaline phosphatase, and serum albumin are recorded.
Some dogs, not more than 25 percent of those starting the test, may be removed from the trial for “non-nutritional reasons” (say, one develops cancer or somehow breaks a leg) or for poor food intake (meaning the dog is not eating enough). Dogs can be removed for the latter reason only in the first two weeks of the test. A necropsy must be performed on any dogs that die for any reason during the test and the findings must be recorded.
The test food will fail the trial if any dog on the test diet shows clinical or pathological signs of nutritional deficiency or excess, or if any dog on the test diet loses more than 15 percent of its initial body weight.
The average weight of the entire test group is also taken into account; the food fails if the entire group’s average body weight change (from the start of the test to the end) is more than -10 percent or if it is less than the average of the control group’s body weight (minus an allowance for normal variation).
The average values from the dogs’ blood tests can also cause a food to fail. The test group must have adequate values for hemoglobin, packed cell volume, and albumin and must not exceed specific values for serum alkaline phosphatase.
A pet food manufacturer can employ the protocol for either a growth or a gestation/lactation study – both are considered more rigorous than the adult maintenance protocol – and still make the “adult maintenance” claim if the food passes the trial.
Finally, in case it wasn’t absolutely clear, feeding trials are not terminal; they do not require the euthanasia of any dogs.
Puppies on Trial
The protocols are similar for the growth and gestation/lactation trials. The major differences are as follows:
In order to make a growth claim, a minimum of eight puppies from three different mothers are required to start the test, with a control group of eight puppies from three different mothers. The distribution of pups of different breeds and sex in the two groups should be the same. A total of 30 puppies are required to establish colony averages. The puppies must be weaned, but no older than eight weeks, when the test is started. The test runs for a minimum of 10 weeks.
The post-trial blood test measures the same blood values as the older dogs, except for serum alkaline phosphatase, which is not measured.
The average body weight gain in the pups fed the test diet must be no less than either 75 percent of the colony average, with averages for males and females determined separately, or the colony average minus 2.33 times the standard error.
For gestation/lactation trials, enough females must be used to ensure that a minimum of eight pregnant females start the trial. The females must be in at least their second heat period and be at least one year of age.
There is no size or breed requirement, but the females must have been bred to dogs of the same breed. Breed distribution must be the same in both the test and the control group. A minimum of 30 pregnant females must be used to develop colony averages.
The test begins at or before estrus, and ends when the puppies are four weeks of age. The females are weighed at breeding, weekly during gestation, within 24 hours after whelping, weekly during lactation, and at the end of the test. The puppies’ body weights are measured within 24 hours of birth, weekly, and at the end of the test.
The litter size is recorded at birth, one day of age, and at the end of the test. Stillbirths and congenital abnormalities are recorded. Both the mothers and puppies are given a physical examination by a veterinarian at the end of the test and general health, body, and hair coat condition are recorded.
As with the other trials, the diet fails if any female or puppy shows clinical or pathological signs of nutritional deficiency or excess. Additionally, 80 percent of all the puppies that survived past the age of one day must survive and successfully finish the test.
Also, the females must gain weight during their pregnancies, and the average percent body weight change of the females – from breeding to the end of the test – can’t be too great. The litter size of the puppies in the test group must be at least 80 percent of the colony average, and they must have an adequate average weight (with respect to the colony averages) at the end of the test.
The required blood test results are similar to those required for the growth trial.
All the World’s a Stage
To earn the right to make the claim that a food provides adequate nutrition for all life stages, the product must pass the gestation/lactation trial and then be fed to the puppies produced from the litters whose mothers ate the test product in a growth trial. This is the most stringent test used to confirm a dog food’s nutritional adequacy.
However, while the term “all life stages” suggests a dog can eat the food from puppyhood to grave, this probably shouldn’t be taken quite that literally, since the inclusion of senior dogs is not required in any AAFCO feeding trial protocol.
A consumer might also mistakenly conclude that an all life stages food is guaranteed to benefit dogs with various health problems – dogs with poor kidney function, cardiac conditions, diabetes, etc. Not so. In fact, there are no AAFCO feeding trial protocols that prove a “medical benefits” claim.
Good, Not Perfect
The most significant criticism of the feeding trials method of providing nutritional adequacy – aside from the alleged cruelty of the tests, which we’ll discuss below – is that foods are tested for just six months. Many people feed their dogs the same food for years on end, unaware that there may be no scientific proof that dogs can thrive on the formula for years on end. Six months may not be enough time for the effects of any nutritional excess, deficiency, or imbalance to express itself to the point of detectable health problems in the test dogs.
AAFCO is cognizant of this concern. The serum alkaline phosphatase assay was added to the adult maintenance trial protocol in recent years, in an effort to detect calcium deficiencies that may not otherwise be detectable in a physical examination at the end of the six month trial.
As another example, there have been reports of foods found to contain levels of taurine that proved too low to prevent the development of cardiomyopathy in consumers’ dogs – after passing feeding trials. And the protocols don’t address the unique nutritional needs of breeds that are prone to genetic disorders that require specific nutritional therapy, such as Bedlington Terriers (which require a diet especially low in copper and high in zinc).
Another criticism has to do with the relatively small number of dogs required in the tests. As we detailed above, 16 is the minimum number of dogs needed to pass a feeding trial to prove an adult maintenance claim; this includes the dogs eating the tested food and the “control” group that eats another food. Theoretically, just eight dogs could “prove” the nutritional adequacy of a food that becomes the sole source of nutrition for millions of dogs. In actuality, the studies are generally more populous than the bare minimum required, but the more dogs that are used, the higher the cost of the tests, so it follows that no formula is likely to be tested on thousands of dogs.
It’s also potentially problematic that the lives – and therefore, the nutritional needs – of dogs in labs aren’t terribly similar to most of our dogs. Of course, as you’ll see below, we’d like to see the living conditions of test dogs come to more closely resemble those of our dogs.
Metabolic Studies
These studies have become far more common since AAFCO established a third way (the “family” protocol) for a product to earn its proof of nutritional adequacy; this method requires a metabolic study of each prospective family member.
Metabolic studies require a dog to be kept, for a minimum of five days, in a cage with a slatted metal floor. This floor allows the lab staff to collect every bit of the dogs’ urine and feces for analysis. The total amount of metabolizable energy in the food can then be determined by tracking the dog’s food intake to calculate the gross energy consumed and subtracting the energy in the waste products.
Life in a Lab
Now for the bad news. PETA is right about one thing: Life in a cage sucks for any animal. This is not quite the same thing as saying life in a cage is inherently cruel. But dogs are pack animals, and a solitary existence, devoid of physical contact with other dogs or other enrichment or socialization does not meet what we would consider a required minimum mental health standard.
And, while any individual feeding trial is just six months, and metabolic studies are just five days in duration, the “time served” by most lab dogs is at least several times those numbers. This is because labs tend to use the same animals over and over again in back-to-back trials. Lab directors defend this recycling, saying it’s surely better to reuse a small population of dogs for a lifetime of trials than to subject a larger number of dogs to just one or a few of the tests.
The good news is that dogs in feeding trials don’t have to live in cages. They can be kept in runs that have access to fresh air and time outdoors, in compatible groups or pairs, and have opportunities to participate in social playtime. Of course, as any kennel operator knows, this sort of facility is far more expensive to staff and maintain. Only pet food makers that really care about its test subjects (or at least, the opinions of consumers) will allocate the extra money for their test dogs to live in an adequately enriched and pleasant environment.
Under pressure from consumers – which can be at least partly attributed to PETA’s media campaign – both the pet food companies and the contract labs they sometimes use are beginning to discuss and consider improving the living conditions for the dogs in their feeding trials.
There have been a number of articles in Pet Food Industry about the industry’s need to improve the welfare of its test subjects. Several pet food industry conventions have presented speakers who made recommendations for lab animal socialization and enrichment programs. And most major pet food makers have published (or made available upon request) a description of their test animal welfare programs and goals.
Reform Still Needed
Unfortunately, this is not to suggest that everything is fine, now. Even the companies that advertise that they provide the very best living quarters, enrichment programs, and provisions for retirement or adoption of their old test dogs don’t invite confirmation of their claims.
For example, one contract lab, Summit Ridge Farms in Pennsylvania, has taken out ads and sent press releases to pet food industry publications, announcing the construction of a huge “puppy playground” and other innovations constituting “the beginning of a long-term environmental enrichment expansion” at its facility. A press release published in Pet Food Industry quoted Mike Panasevich, president of the company, as saying, “We are extremely happy and proud of our facility and the enrichment programs currently in place.”
However, this same executive wouldn’t return our repeated calls or e-mail messages to discuss these positive developments with us – not what you’d expect from someone who had genuine innovations to show off.
This opaqueness makes it appear that the industry still has a lot to hide. And, unfortunately, PETA’s infiltration of a contract lab has now afforded the entire industry with a convenient excuse to hide its work, citing security risks.
Throwing Down a Gauntlet
It seems to us that it would be in the best interests of pet food companies and contract labs to keep their test subjects as happy and comfortable as possible. We imagine this would help the foods produce and maintain health in the test dogs, so the products pass with flying colors.
But the companies would also be wise to do the right thing by their test animals as a marketing technique. For our part, we’d be thrilled to promote a pet food made by a company that could and would prove that its labs provide the best possible living conditions for its test subjects, with comfortable living quarters, plenty of socialization and exercise, and attentive veterinary and behavioral care.
One would think that a policy of openness and full disclosure at a facility that was truly doing everything right for the test dogs and cats would be a fantastic selling point for a pet food maker. But we haven’t found a company that’s willing (or able?) to take that challenge.
-Nancy Kerns is WDJ’s editor.