Download the Full April 2017 Issue PDF
Are Grain-Free Foods Taking Over the Premium Dry Dog Food Market?
I was in a chain pet supply store the other day, looking for a higher-quality food for some foster dogs from my local shelter who are a little chubby. For this reason, I was looking for a product that was not too high in fat.
I was a bit surprised to realize that grain-free foods have sort of taken over the shelves in the section of the store where the higher-quality foods are stocked. Many of the companies whose products appear in the “natural/holistic” or “premium” section seem to offer only grain-free foods. I had to go through several aisles before I found a product from a company that I like offering a food that contained grain and had a lower fat content.
After I got home, I did more research; are these companies discontinuing their dry dog foods that contain grain? The answer was no; the companies I was thinking of still offered those products, but the chain store where I was shopping that day didn’t stock them. That said, some of the companies have far more grain-free options than foods that contain grain.

For example, one whole aisle was devoted to Merrick, and only Merrick’s grain-free foods were being sold. Most of these foods contain a minimum of 38 percent protein and 17 percent fat. At home, I saw that Merrick still offers a “Classic” line of foods that contain grains, and these contain slightly less fat (15 percent) but also less protein (25 percent in the case of the lamb variety, and 30 percent for the beef and chicken varieties).
The marketing of foods has also gotten very focused on grains, whether pro or con. Merrick highlights the Classic line as containing “ancient grains like quinoa.” Quinoa is a favored ingredient in dog food advertising, perhaps because no one has yet launched a campaign against it. Never mind that quinoa appears fairly low down on the ingredients lists of these foods. For example, in Merrick’s Chicken variety, it appears 10th on the ingredients list, well below peas (3rd), brown rice (5th), and barley (6th).
Some dogs do better on grain-free foods than on a diet that contains grains, but this isn’t true of all dogs. I wouldn’t give grain-free foods a blanket recommendation for all dogs; I don’t think they are a superior diet, except for dogs that have a specific problem digesting grains. Other dogs might have difficulty digesting the carbohydrate sources that are in the grain-free foods!
How about you? Are you feeding grain-free? If so, why? Have you seen any changes in your dog’s health or digestion since using these diets?
Note: We published a great article on the issue of grain-free foods in 2010. Check it out!
Why I’m Grateful for My Dogs – Again
Yesterday, I had a long list of things that I needed to do and had committed to doing – things for myself, my job, my husband, a friend, and the shelter where I volunteer. The list was so long that just contemplating it made me feel tired.
Not even on my list, but in the back of my mind, was the knowledge that the dogs haven’t been out for a good long run in days and days. Nine-year-old Otto can cope with that; while he loves going out for off-leash runs, his behavior doesn’t really change if he doesn’t have that opportunity.

But Otto’s counter-point is one-year-old Woody, whose behavior gets increasingly gravity-defying with each day that goes by without a run. The carpet runners in my hall start piling up at either end, as he finds he can no longer walk through the house; he has to dash down the hall and slide into the room at either end. He starts greeting guests with airs above the ground. Wooden things (like the redwood bench on my deck) start getting chewed anew.
My son’s three-year-old dog, Cole, who is staying with me for a couple weeks while my son travels, is somewhere between my two. He can maintain good behavior when he’s not getting daily runs, but his neuroses start increasing. (Like a lot of coonhounds, he’s a sensitive soul and inconsistently demonstrates weird behaviors, such as spinning before mealtime, trembling and panting while riding in the car, hiding if anyone raises his or her voice, especially if another dog is getting reprimanded).
So when I realized that the sun was going down on a rain-free day – and we haven’t had many of those lately – I gave up on the thought of ticking off a few more of the things on my to-do list in favor of taking the dogs out for a run in our favorite place.
This particular place will close to off-leash dogs in just a few days, and stay closed until the end of June, for the nesting season. It’s a “wildlife area” – not a “wildlife refuge,” as several of my friends have mistakenly called it – but an area that is nevertheless managed by the state fish and wildlife department for recreation and hunting. Migratory ducks and geese nest there, as do native pheasant, quail, doves, and countless other non-game species of birds. All the so-called “game birds” are hunted there in specific seasons, but from March 1 through June, the birds get a break from predatory humans and their off-leash dogs, to lay eggs and hatch their babies. So this run was probably the last one that my dogs will have in the tall, green, open fields until next year. (They can run there again when the grass is all California summer brown, and the birds are all back in the air.)


They needed it – the chance to stretch out and race each other across the fields.
All the dogs had a good time running, but none more than Woody. He runs and ducks and swerves and does these great kangaroo bounces, seemingly for the simple joy of doing them. It looks like he’s chasing a rabbit or running a race, but mostly, while Cole and Otto are munching on the tender spring grass or sniffing the small game trails, Woody is doing these great, looping laps of the field, all by himself, running for the joy of running.


As much as Woody and the others needed a chance to race around outdoors, what I remembered once we were out there, and I was laughing so hard I nearly peed myself at Woody’s antics (and couldn’t concentrate on making sure my camera was taking proper exposures), was that I totally needed it, too.
After the past week of pressure from the rain and the constant threat of another evacuation or flooding, and helping with evacuated shelter dogs who are being housed by half a dozen of my friends, on top of my own work and family obligations, I didn’t realize how tense I was, how shallowly and tightly I have been breathing all week. As I walked outside under a wide open sky, through the deep, wet, green grass, surrounded with birdsong and geese calling each other overhead, and led by three vibrantly healthy, exuberant, responsive dogs, I felt my tiredness float away. I felt my lungs start to work again; I breathed deeply, taking in all that color and oxygen and joy.
If it hadn’t been for the dogs – for trying to get the dogs tired – I’d still be exhausted! But that walk filled me up, and I’m happily plowing through my to-do list again, even as they sleep.
For the millionth time, thank you, dogs!

Canned Dog Food Recall Gives Rise to More Questions Than Answers
This article was originally published in early Feb. 2017. Updates are in bold below.
On February 3, 2017, the FDA announced that Evanger’s Dog & Cat Food had recalled five lots of its canned Hunk of Beef dog food, for a “potential contaminant,” pentobarbital. One dog has died after eating the food, and three others were sickened. All four dogs belong to the same family, and ate food from the same can of food. [Note that various media outlets, including the original television broadcast with the owner on camera, have reported that the family brought four dogs to the veterinarian and one died. The FDA has been reporting that the family brought FIVE dogs to the vet and one died.] The dog that died was necropsied, and some food from the open can of food was tested. The results: both the dead dog’s stomach contents and the open can contained pentobarbital, a drug commonly used to euthanize animals.

Given that the Hunk of Beef food – an incomplete diet meant for supplemental or intermittent feeding – contains nothing but beef chunks, Evanger’s is blaming its supplier of the beef used in the batch of contaminated food. The company has announced a voluntary recall of that batch of food, as well as four other batches of food produced the same week with beef from the same supplier. [UPDATE: Evanger’s also makes a food called “Against the Grain,” which is not overtly labeled as an Evanger’s product. The “Pulled Beef With Gravy” variety of Against the Grain has since been recalled by Evanger’s.]
The company says it has terminated its relationship with the meat supplier for both products, despite a 40-year history of doing business together.
No other reports of dogs being sickened by this or other Evanger’s products have emerged.
That’s the short, simple version.
But this is a weird tale, and I suspect it’s going to take a long time for all the details to come out – if they ever do.
Weird thing #1: The owner of the dead dog has exchanged only one brief communication with Evanger’s.
The dog that died and the others who were sickened belonged to a single owner in Washington State. They were all Pugs, who were fed a single can of Evanger’s Hunk of Beef food as a “topper” on their usual dry food on New Year’s Eve (Saturday, December 31, 2016), as a treat. The owner of the dogs claims that within 15 minutes of the meal, the dogs began acting strangely, acting dizzy or “drunk,” and falling over. She took all the dogs to an emergency veterinarian, where all of them were treated, but one dog died.
We have not yet contacted the dog’s owner to verify the exact chain of events, but it would seem that the owner published a post on Instagram some time on Sunday, January 1, blaming the Evanger’s food for her dog’s death.
At 3 am on Monday, January 2, someone forwarded the Instagram post to Evanger’s. The company immediately began trying to contact the owner.
It would appear that on Monday, the owner posted an account of her story on the crowd-funding site YouCaring, asking for help with her dog’s vet bills. Evanger’s, still trying to contact the owner, paid the full amount that the owner was asking for on the YouCaring post, and asked the owner to please contact them.
A local television news station, KATU, interviewed the distraught owner discussing the event and picking up one of the surviving dogs from the veterinarian on Monday morning. This report was broadcast on Monday evening, January 2.
To date, Evanger’s says it has had only one direct communication with the dogs’ owner, a single short email.
The YouCaring page has been taken down. The dog owner’s Instagram page is now private.
Weird thing #2: Meat supplier is as yet unidentified.
Neither the FDA nor Evanger’s has revealed the name of the company that supplied the meat in the recalled lots of food.
In the case of most food-based recalls, whether the product is meant for consumption by humans or pets, if a specific ingredient in the food is suspect, the ingredient is generally traced to its source. What if the adulterated ingredient was used in other food products, elsewhere?
We contacted the FDA and asked why the meat supplier involved in this case has not been named. FDA spokesperson Anne Norris responded: “FDA’s investigation is ongoing, and the agency is committed to providing additional information as it becomes available,” and promised that she would be in touch when she is able to provide us with additional information.”
UPDATE: On February 17, the FDA released the following statement:
In its recent press release announcing a limited product recall, Evanger’s Dog & Cat Food Company, Inc. stated that the beef for its Hunk of Beef product came from a “USDA approved” supplier. However, the FDA reviewed a bill of lading from Evanger’s supplier of “Inedible Hand Deboned Beef – For Pet Food Use Only. Not Fit For Human Consumption” and determined that the supplier’s facility does not have a grant of inspection from the United States Department of Agriculture’s Food Safety and Inspection Service. The meat products from this supplier do not bear the USDA inspection mark and would not be considered human grade. USDA-FSIS regulates slaughter of animals for human consumption only. Testing by USDA-FSIS of Evanger’s Hunk of Beef confirmed that the meat used in the product was bovine (beef).
The investigation by the FDA is ongoing and includes examination of the suppliers of beef to Evanger’s and Against the Grain to determine a possible cause for the presence of pentobarbital. The FDA is also coordinating with the USDA to address any possible areas of shared jurisdiction at the suppliers.
Weird thing #3: Dog owner has communicated with bloggers.
A site I would describe as a conspiracy theory pet-food blog seems to have been in contact with the dog owner, and has been publishing highly inflammatory posts about the case. The site also published the necropsy report for the deceased dog, thanking the dog owner for supplying the report and allowing her to publish it.
Further, the blogger published an “updated” (yet undated) post claiming to have received information from a fellow blogger that she “received confirmation from an [unnamed] FDA spokesperson” that FDA testing carried out in the agency’s Veterinary Laboratory Investigation Response Network (Vet-LIRN) detected pentobarbital in “closed cans of food collected from the dog’s owner and from the retail location where the food had been purchased.” There has not yet been what we would consider credible evidence that this is true, nor has the FDA confirmed this.
UPDATE: In the press release on February 17, the FDA stated for the first time publicly that “unopened cans of the product from the pet owner and retailer that sold the products (from the same production lot), were tested by FDA’s lab. All of the samples tested positive for pentobarbital.” We have to ask: Why, if this information had been released to a pet food blogger some time ago, could this not have been confirmed and made public sooner?
Most important weird thing (#4): The presence of pentobarbital in a pet food.
The conspiracy theory bloggers and the pet owners who believe them are convinced, despite any credible evidence to the contrary, that euthanized dogs and cats are used as ingredients in pet food, and that any pentobarbital found in pet food proves this.
Pentobarbital is, in fact, commonly used as a euthanasia agent in pets and horses; it is also sometimes used to euthanize livestock – not on commercial food animal production facilities, but on family farms. I, myself, had a veterinarian euthanize my family milk cow with pentobarbital when it was “her time.”
However, no animal euthanized with pentobarbital should wind up in any facility that makes any product that will end up in pet food. There are Federal food safety laws that do not permit dead pets to be rendered in facilities that produce fats, meat meals, or bone meals that will be sold to pet food makers.
Pentobarbital has been detected in dry pet food in the past. The FDA’s Center for Veterinary Medicine began looking into the issue in 1998, and conducted tests on pet foods that year and again in 2000. The FDA issued a “white paper” about its findings in 2002, concluding that euthanized cows and horses that had (illegally) found their way into pet food, but that the levels of pentobarbital found in some pet foods were so low, that they would not pose a risk to the health of dogs and cats that ate those foods. The FDA also stated that every food in which pentobarbital was detected was subjected to tests looking for dog or cat DNA, but none was found.
Off the record, old-timers in the pet food industry will admit that more than 20 years ago, euthanized pets probably were occasionally used by unscrupulous pet food producers as a source of “meat and bone meal.” However, every industry source we have interviewed claims that this could not happen with today’s food safety laws and oversight. Any company that risked such a thing would be setting themselves up for swift financial suicide.
Cows or other food animals (pigs, sheep, chickens, etc.) that die before they can be killed at a slaughtering facility are, by Federal law, not allowed to enter the slaughtering facility, but must be diverted to a rendering plant that makes ingredients for non-food products, such as fertilizer, biodiesel fuel, soap, and candles.
If an animal that was euthanized with pentobarbital was slaughtered and its meat sold for pet food, it would be a serious violation of Federal food safety laws.
We will be reporting further on current Federal laws governing the rendering industry, and explaining the differences between rendering plants that produce meat meals and fats that may be used in pet foods, and the rendering plants that utilize “4D” material (dead, dying, diseased, disabled).
Who is liable?
Pet food companies are technically liable for ill effects caused to an animal by their products, but in point of actual fact, any pet food company whose product harmed an animal will be trying to determine if someone else was at fault. Start the clock on the filing of lawsuits, counter-suits, and finger-pointing.
When a company’s food is actually made by a contract manufacturer, it’s likely that the company whose name is on the label will try to blame the co-packer, saying, “We did not authorize that ingredient/source to be used in our food…it was used without our knowledge.” And the co-packer will shoot back, “The company absolutely knows what we put in their food; here are the ‘run sheets’ that they signed off on, proving they know what was in the food…” They typically sue each other, and then settle out of court, with the case sealed so that the public never learns who was truly at fault, the company whose name is on the label, or the co-packer.
In this case, the food was made by the company whose name is on the label. Evanger’s makes its own food in its own plant – and the food (according to its label) contains nothing but beef. What could they do but blame their meat supplier?
We’ll continue reporting on this story as it develops.
Oroville Dam Case Study: How Evacuating People And Animals Early and Often Can Save Lives

In the winter of 1997, the town where I live now, Oroville, California, had a big flood. I didn’t live here then. But that year, the Feather River, which (usually) flows tamely right through my town, was threatening to massively flood the town. There is a dirt levee that separates the river from the main streets, and it seems like an historic artifact most of the time – a thing that was built by pioneers to try to keep the Feather from flooding the town again and again. It seems quaint now, because since 1968, the town has been more significantly protected by the Oroville Dam, with a huge reservoir (Lake Oroville) behind it – the combination that meters out the Feather at a safe and sane rate, protecting the town and much of the Sacramento Valley below from flooding. But with truly historic rainfall, like in 1997, the operators of the dam can’t help but let out so much water that the river swells to capacity, and suddenly our old historic levee is important once again, holding back the Feather from flooding Oroville.
In 1997, with the Oroville Dam letting out maximum quantities of water, and the Feather crazily high, the levee started seeping. County officials called for an immediate evacuation of Oroville. If the levee burst, they said, the town would be covered with 12 feet of water.
The local animal shelter lies about a mile and a half from the river, in the prehistoric flood plain of the Feather. Wild-eyed police officers gave the then-director of the shelter 15 minutes to get her staff and herself out of the shelter. Faced with the prospect of every animal in the shelter drowning, and with no way to evacuate 60-some animals that quickly, she made the horrible decision to euthanize every animal. Every staff member was pressed into helping. The animals were left dead in their enclosures, the doors locked, and the staff fled.
But the levee held, and the town didn’t flood.
It was a horrible, traumatic day for everyone involved. And the horror was burned into the memory of at least one of the kennel workers, who still has nightmares about it. Today, that former kennel worker is the director of the same shelter, now located in a newer facility about 300 yards from the old one. And today, on any given day, the shelter holds about three times as many animals as before.
This last week, as you may have heard, the town of Oroville was evacuated again. Northern California, on the heels of a long drought, is being inundated with rain. The mighty Feather is again roaring, and the Oroville Dam is holding it back. But the structure recently suffered catastrophic damage: A huge hole suddenly developed in the main spillway, where floodwaters can be dumped out of the lake when inflow exceeds outflow. Even with the lake filling fast, the dam operators had to shut off the outflow, to ascertain the extent of the damage. The lake neared the brim, the point at which the water of Lake Oroville would start to flow over the top of them never-once-used “emergency spillway” – basically, the engineered lowest spot on the downstream edge of the lake, positioned at what seemed like a safe distance from the dam itself.

The current director of the shelter, who still tears up and starts trembling at the thought of that horrible day 20 years ago, wasn’t going to sit still and wait for the police to give the staff 15 minutes or even 15 hours to evacuate. With the lake nearing full, and given the damage to the spillway, she pulled the trigger on a precautionary evacuation, days before any other official in the county thought it was necessary.
On Friday, February 10, as water started pouring over the “emergency spillway” on the dam, the director started reaching out to every animal rescue group the shelter has ever done business with, and asked if they could come take some animals. Hound rescue, Lab rescue, small dog rescue…you name it, they were called. She announced a “Dam Good Adoption Event” – every adoptable animal could be adopted for free. And she called on all people who foster animals, if they lived outside the evacuation zone, to come and take some animals.
I live three blocks from the levee, definitely in the potentially flooded zone. But I helped get dogs to friends’ homes. One friend took two dogs; another took six puppies, from several different litters. All the cat cages were loaded up into trailers, and taken to the homes of shelter employees who A) lived in a safe zone and B) had a warm barn or garage where they could care for the cats safely. (Fortunately, all of the cat kennels are mobile, and can be rolled about in sets of nine cages, making it super easy to move the cats with bowls and litter pans in place.)
Another friend hitched up her horse trailer, and late Friday evening, transported 10 large dogs in crates to my friend Sarah Richardson, who owns and operates The Canine Connection, a training, daycare, and boarding facility. After we got those 10 situated, Sarah asked how many dogs were left, and offered to take more. We took a second trip with six more, and the woman who was driving the shelter took six more to her home.

On Saturday, with only a handful of dogs in the shelter (the ones that the county animal control officers had picked up as stray in the past couple of days, and that the shelter did not have authority to move), the director directed the staff to start a deep cleaning of the shelter. May as well stay busy! In the meantime, up at the dam, workers were growing concerned about severe erosion being caused on the face of the hill next to the dam from all the water pouring over the emergency spillway.
On Sunday afternoon, the shelter was closed, with just a small number of dogs that county animal control would not let us move. And then came a mandatory order to evacuate the town of Oroville – immediately. The order said there were indications that erosion on the hill below the emergency spillway was undercutting the gates that control the flow of water over the main spillway. If the gates failed, the lake would begin to flow in an entirely uncontrolled fashion over the hill next to the dam, essentially carving a new river channel next to the dam. The dam operators estimated that the thing could collapse within an hour. And if it did, a 30-foot wall of water would be right behind it, leveling my town.
When the emergency evacuation order was broadcast, on radio, TV, and cell phones, I was helping my friend Sarah with the 15 evacuated shelter dogs in the next town over, completely safe. I had my dog Woody with me, but my husband, our dog Otto, and my son’s dog Cole (who is staying with us while my son is on a trip to New Zealand), were at home, right in the path of danger. My husband’s stated goal for the day was to mow the weeds (all that’s left of our lawns after several years of drought) and trim some trees. So he was outdoors, running loud equipment, and with his cell phone in the house. I called and texted him numerous times, getting more and more panicky by the second. I called and texted every friend I knew who was also in the danger zone; they were all packing and driving away.
I had started driving toward my town, scared stiff that at any second I was going to hear on the radio that the lake was headed to town, shaking and crying, and begging my husband to call. The traffic on the other side of the highway, headed out of town, was getting thicker and thicker. I didn’t want to drive into a wall of water, but I had to get my husband and dogs.
Thank goodness, my neighbor over my back fence heard my husband in our yard and yelled at him when the mower shut off. “THERE’S AN EVACUATION!” she told him. That’s when he finally picked up his cell phone and saw that I had sent him a half dozen texts and voice mail messages to “PLEASE GET THE DOGS AND GET OUT!” He grabbed a few things, and was tying the dogs in the back of his truck, even as police drove by twice, each time yelling over the megaphone at him to “LEAVE NOW!” Only when he was in the truck and driving out of town did he call me to say he was on his way out. When the call came, I was right at the last possible exit where I could turn around and also head back in the direction of safety. I waited there for him, and we shifted the dogs from the back of his truck into my car, and then we joined the traffic back to a nearby safe town.
The police wouldn’t allow the director of the shelter to go to the building and evacuate those last 15 or so dogs.
That night, we all watched the news, held our breath, and said prayers.
The next morning (Monday), the chief of police, likely feeling a little bad for pooh-poohing the shelter director days earlier, kept vigil while she oversaw the evacuation of the last few dogs from the shelter. At last ALL the animals, some 200 dogs, cats, birds, and a pig or two, were safe.
On Monday and Tuesday, the weather was sunny and warm and beautiful. My husband and I (and the three dogs) stayed with a friend in a nearby town. I had no computer, just my phone. I spent most of my time at my friend Sarah’s place, trying to help care for the evacuated dogs – and with Sarah promoting them on her Facebook page, adopting six of them out!!
Conditions at the dam improved, and midday on Tuesday, the Sheriff downgraded our evacuation to an “evacuation warning” – meaning, we could go home, but we should keep our cars packed, radios on (and mowers off, maybe!), be ready to evacuate again. The shelter director is keeping all the evacuated animals in foster care. Until the Sheriff moves the prisoners that he’s in charge of back into the county jail, also in the evacuation zone, we’re not moving animals back into our shelter, either.
As I write this, it’s Wednesday morning, and a storm is moving in. If the lake water rises rapidly again, and conditions deteriorate, another evacuation will be called. This time I will be more ready, with my computer and all my dogs with me, and I’ll duct-tape my husband’s cell phone to his to his body, I think. But no matter what happens, the shelter animals will be safe, thanks to the efforts of many local animal lovers AND, most significantly, to the hyper-vigilance and experience of my local shelter director, Lorraine “Rainy” Green. That’s really her name! She avoids the spotlight like the plague, but I hope she will take a bow when this is all over.
Why Dogs Bark and How to Stop Them

As I write this I can hear my Kelpie, Kai, in the backyard barking at . . . something. Kai barks a lot – at squirrels, cats, birds, horses – anything that moves! I can empathize with dog owners who live in closer quarters, where a barking dog can be the catalyst for neighbor feuds, animal control citations, and civil lawsuits. And I thank my lucky stars that our nearest neighbors are a half-mile away and not likely to complain about occasional bouts of canine cacophony.
Barking is a natural, normal canine behavior. If you have a dog, you need to understand and accept that sometimes dogs bark!
That said, some dogs bark a whole lot more than others. Dogs also bark for a variety of reasons. How you work to manage and modify your dog’s barking will depend, at least in part, on what motivates him to bark.
Step one of any good barking-modification program is minimizing your dog’s need and opportunity to bark. Exercise, an important element of many good behavior modification programs, is useful here as well. A tired dog has less energy, hence less need to bark, and a well-exercised dog tends to be emotionally healthier as well.
Meanwhile, good management minimizes barking opportunity. Close drapes or put up baby gates to deter out-the-window barkers. Use white noise or calming music to muffle sounds that set off your dog. The more your dog practices his unwanted barking behavior, the more often is it reinforced (barking makes the mail carrier go away!), and the harder it is to modify.
Finally, in order to successfully modify barking behavior, you have to understand why your dog is barking.
Reasons Dogs Bark and How to Modify It
Again, how you manage and modify your dog’s barking will depend on what’s motivating him to bark. You might successfully ignore a demand barker’s utterances and reinforce him for quiet, but ignoring a dog who is barking from anxiety can exacerbate the behavior.
Here are the most common reasons that dogs bark, and how to resolve them:
Alarm Barking
A dog who alarm-barks may save his family from a fire, inform you that Timmy’s in the well, scare off a rapist – or just go bonkers every time someone walks past your house on the sidewalk. This dog is doing his job: letting you know there’s something to be seriously concerned about. Alarm barkers can save lives, but sometimes their judgment about what constitutes an alarm-appropriate situation can be a little faulty.
To manage alarm-barking, reduce your dog’s exposure to stimuli that cause his arousal. Perhaps you can baby-gate him out of the front room, move the sofa away from the windows so he can’t jump up and see out, close drapes, or tape poster board over the windows. Outside, install a privacy fence, attach a solid barrier of some kind to your see-through chain-link fencing, or put up an interior fence to block his access to the more stimulating parts of the yard.
You can also use counter-conditioning and desensitization to modify barking at things he really doesn’t need to be alarmed about. Sit with him at the window. As soon as someone comes into view, let him look, feed him a high-value tidbit, let him look again, feed again, until the passerby is out of sight. When you’re not there to feed, prevent access to windows that look out on passersby.
Given that alarm barking will inevitably occur, it’s also useful to teach your dog a positive interrupt – a cue, friendlier than “Shut up!” that you can use to stop him in mid-bark. (See “The Positive Interrupt,” below.) However, your dog might be barking because something really is wrong. Before you use that positive interrupt, take a moment to see what your dog is barking at. Perhaps your house really is on fire.
Alert Barking
This is your dog’s less-aroused approach to letting you know that there’s something of interest afoot; a squirrel on the back fence, or Dad’s car pulling in the driveway at the end of the work day. It can be managed and modified in the same manner as alarm-barking, including use of the positive interrupt, but is usually easier to work with because the emotional level is much lower.
Anxiety Barking
Barking due to anxiety can be manifested as a number of behaviors, including hysterical barking and sometimes howling. This is a complex and challenging behavior to both modify and manage, because true anxiety is a real panic attack – the dog truly cannot control his behavior.
One of the most common presentations of this condition is separation anxiety – a very difficult behavior to live and work with. (See “Relieving a Dog’s Separation Anxiety,” WDJ July 2008.) Real anxiety usually requires the intervention of a good positive behavior consultant, and often, behavior modification drugs. If your dog’s barking is due to anxiety, consult with a professional behavior counselor, and manage his environment to minimize his exposure to anxiety-producing conditions while you help him learn how to cope. (Note: The use of shock collars, not something I would recommend in any case, is a horrifically poor choice here, almost guaranteed to increase your dog’s stress and anxiety.)
Boredom Barking
Dogs are social creatures, and the backyard dog is lonely and bored. Boredom barking is often continuous, with a monotonous quality: “Ho hum, nothing else to do, I may as well just bark.” This kind of barking is most annoying to neighbors, and likely to elicit a visit from a local animal control officer.

The answer here is obvious and relatively easy. Bring the dog inside. Many outdoor barkers are perfectly content to lie quietly around the house all day, waiting for you to come home, and sleep peacefully beside your bed at night. If your dog isn’t house-safe, use crates, exercise pens, dog walkers, lots of exercise, and even doggie daycare to keep him out of trouble until he earns house privileges. You can also enrich his environment by giving him interactive toys such as food-stuffed Kong toys to keep his brain engaged and his mouth busy. See “Must-Have Chew Toys,” (WDJ 2016) for some of Whole Dog Journal‘s favorites.
Demand Barking
This behavior is more likely to annoy you than your neighbors, but it’s annoying nonetheless. A demand barker learns that he can get what he wants (usually attention or treats) by making noise. It often starts as a gentle, adorable little grumble, and can quickly turn into insistent, loud barks – your dog’s way of saying, “I want it, now!” You can preempt the development of demand barking by remembering to randomly give your dog attention and treats for being quiet, before he starts barking.
Demand barking, once it starts to occur, is easiest to extinguish early. The longer a dog has been reinforced for demanding stuff, the more persistent he’ll be when you try to ignore him. However, ignoring him is the best answer to this behavior. No treats, no attention – not even eye contact. The instant the demand behavior starts, utter a cheerful “Oops!” and turn your back on your dog. When he’s quiet, say, “Quiet, yes!” and return your attention – and treat – to him.
Beware “extinction bursts” and “behavior chains.” When you’re trying to extinguish a behavior by ignoring it, your dog may actually increase the intensity of his “I WANT IT NOW!” behavior. This is an extinction burst, akin to you kicking the soda machine that doesn’t deliver after accepting your coins. If you succumb to your dog’s increasing intense barking, thinking extinction isn’t working, you have now reinforced the more intense barking, and your dog is likely to get more intense sooner next time. If you stick it out and wait for the barking to stop, you’re well on your way to making it go away. You have to be more persistent than your dog.
A behavior chain is a series of behaviors strung together. You dog may learn that if he barks once or twice, you will turn your back, say “Quiet,” and then feed him a treat. His short behavior chain is “bark . . . and then be quiet.” To avoid this, be sure to acknowledge and reward him frequently before he barks even once.
Frustration Barking
Often confused with anxiety barkers, dogs who have a low tolerance for frustration bark persistently when they can’t get what they want. Unlike anxiety barking, this is an “I WANT IT!” communication similar to demand barking, but with more emotion. It’s usually directed at the thing he wants, such as the dog he wants to go play with.
You can use the positive interrupt to redirect frustration barking. If you consistently offer high-value treats in the presence of frustration-causing stimuli, you can condition your dog to look to you for treats when the other dog is present (dog = yummy treats) rather than erupt into a barking fit.
Greeting/Excitement Barking
“Yay, Mom’s home! Mom’s home!” If your dog hails you with hellos when you return after a long (or short) absence, it’s time to shift into ignore mode. Stand outside your door and wait for the cacophony to subside, then enter calmly; no rousing hug-fests or “I missed you so much!” sessions. When your dog is calm and quiet, then greet him. If he starts to bark again, mark the barking with an “Oops!” and ignore some more.
If his loud greetings are directed toward arriving guests, you’ll still need to go into calm mode. If you use loud verbal reprimands you add to the chaos and arousal. Rather, use your positive interrupt to invite your dog to you, and calmly put him in another room or on a tether – then greet your visitors. Alternatively, you can use counter-conditioning to get your dog to look to you for treats rather than erupting with barks when visitors arrive. You may want to tape a note to your door advising guests that you are training your dog and it may take you a moment or two to answer the door, so they don’t give up and go away.
Play Barking
This is common behavior for herding dogs, the cheerleaders of the canine world. As other dogs – or humans – romp and play, the play-barker runs around barking (and sometimes nipping heels). If you’re in a location where neighbors won’t complain and the other dogs tolerate the behavior, you might just leave this one alone. With children, however, the behavior is not appropriate, and the dog should be managed by removing him from the play area, rather than risking bites to children.
If you do want to modify play-barking behavior, you can use negative punishment: The dog’s behavior makes the good stuff go away. When the barking starts, use a time-out marker such as “Oops!” and gently remove your dog from the playground for one to three minutes; a tab (a short, six- to 12-inch leash left attached to his collar) makes this maneuver easier. Then release him to play again.
Over time, as he realizes that barking ends his fun, he may get the idea. Or he may not – this is a pretty strong genetic behavior, especially with the herding breeds.
The Positive Interrupt
The positive interrupt is a well-programmed, highly reinforced behavior that allows you to redirect your dog’s attention back to you when he’s doing something inappropriate, like barking. Ideally, you want your dog’s response to the “Over here!” cue to be so automatic that he doesn’t stop to think, he just does it, the way your foot automatically hits the brake of your car when you see taillights flash in front of you on the highway.
Here’s how to teach a positive interrupt:
1. Install the cue in a low-distraction environment. Use a phrase such as “Over here!” or “Quiet please!” as your interrupt cue. Say the phrase in a cheerful tone of voice, then immediately feed your dog a morsel of a very high-value treat, such as a small shred of canned chicken. Repeat until you see his eyes light up and his ears perk when you say the phrase.
2. Practice with the cue in a low-distraction environment. Wait until your dog is engaged in a low-value activity – wandering around the room, sniffing something mildly interesting – then say your interrupt phrase in the same cheerful tone of voice. You should see an immediate interrupt in his low-value activity, and he should dash to you for his chicken. If he doesn’t, return to Step 1.
3. Add distractions to your practice. Still in the low-distraction environment so you can control the distraction level, add moderate distractions – one at a time – and practice the interrupt. Gradually move up to major distractions in the low-distraction environment. If you lose his automatic response at any step, return to the previous step.
4. Move your lessons to an environment with real-life distractions. Go for a walk around the block with your dog on leash. Use the interrupt when he’s sniffing a bush, or eyeing a fast-food bag on the sidewalk. Start with mild to moderate real-life distractions if possible, but if a major distraction presents itself, including a stimulus that causes him to bark, give it a try!
5. Use the positive cue to interrupt barking. When your dog automatically turns his attention to you in response to your cue when confronted with major real-life distractions, you have a valuable tool for interrupting his barking. Be sure you practice occasionally with mild distractions to keep the cue “tuned up.” And remember to thank him and tell him what a wonderful dog he is when he stops barking on your request.
Barky Breeds
Some breeds of dogs are notorious for being vocal, and even within breeds there are some lines that are known to bark more than others. There is a genetic component to a dog’s vocal behavior (as behavior is always a combination of genetics and environment – nature and nurture.) Note that when we say a behavior is “genetic,” what we really mean is that the dog has a strong inherited propensity to be reinforced by the opportunity to engage in that behavior. By definition, behaviors that are reinforced increase; a dog who finds barking reinforcing and has opportunities to bark will bark more.

Most of the herding breeds have strong opinions about things and aren’t afraid to express them. Think Shetland Sheepdog, Collie, Border Collie, Australian Shepherd, Australian Kelpie . . . . Barking is part of the constellation of behaviors that were selected for over the years as these dogs were expected to be “large and in charge” when directing the movement of sheep and cows – animals many times their weight and size.
Scenthounds (such as Beagles, Bassets, Bloodhounds, etc.) have also been bred for their “voice.” As they chase game, their excited baying tells their humans where they are, and enables hunters to find them when their quarry is treed or goes to ground.

Many small breeds of dogs (Chihuahua, Yorkshire Terrier, Miniature Pinscher) are known to be quite vocal. They have earned a reputation as “yappers” – making up for their diminutive size by making a lot of noise.
Then there are the dog breeds known to be at the quiet end of the canine vocalization continuum. Many of the Giant breeds – Danes and Newfoundlands, for example – are generally less vocal.
There are also many smaller breed dogs, including the French Bulldog, Cavalier King Charles Spaniel, and Shiba Inu, that have reputations for being non-talkative. And then there is the Basenji, which doesn’t bark, but is capable of making a number of other alarming and annoying vocalizations. Rather than bark, these dogs can scream, growl, even yodel in a canine sort of way.
Whether you are looking for a quiet dog for townhouse living, or a vocal one to ward off trespassers from your rural home, knowing which breeds bark less is a good place to start. That said, it’s also important to remember that, despite breed tendencies, every dog is an individual. You can find a Great Dane who will rattle your apartment walls, and a Sheltie who wouldn’t speak if the safety of your farm depended on it. If voice, or lack thereof, is important to you, make sure you look beyond simple breed stereotypes to actual behavior when selecting your next canine family member.
Be Proactive with Dog Barking Modification
Uncontrolled barking can be frustrating to the human. I know this all too well, with two vocal herding dogs currently in my own family. However, our dogs sometimes have important and interesting things to say. There was the time I was engrossed in writing an article and our dogs were alarm barking ferociously in the backyard. Resisting the urge just to tell them to stop, I reluctantly got up to investigate. No, the house wasn’t on fire, but I did find a sick groundhog in the yard.
You do want to be able to have some control over your dog’s voice, but don’t lose sight of the value of his vocal communications – he may be trying to tell you something important. If you ignore him, your dog might do combat with a rabid skunk in the yard, a burglar might make off with all the bikes and tools in the garage, or Timmy might drown in the well!
Letters from Readers: March 2017
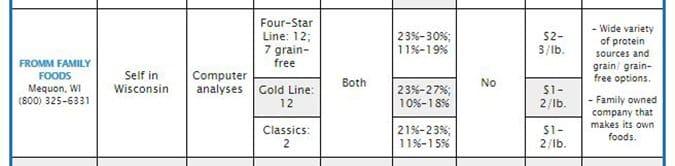
I have been a subscriber for years to Whole Dog Journal. I am always particularly interested in the approved dry (and canned) food lists. This year’s “approved dry foods” list is a little weird. It says it’s the 2015 approved dog foods instead of 2017. My other concern is that Fromm, the dog food I’ve been feeding my babies, is not on the list this year. Please be kind enough to let me know why Fromm is not on your list this year. I am very concerned!
Sharon DiDomenico
via email
The “2015” was the sort of typo that will recur in our nightmares for a decade. What appeared in the February 2017 issue really is the 2017 list.
Also, we’re very sorry about the accidental omission of Fromm Family Foods. The company did provide us with the information we asked for; their response got lost in (considerable) shuffle of information. They were added to the online version of the magazine. Had it appeared in the print version, their entry would have looked like the following. We regret the errors.
I read with interest Cynthia Foley’s article on honey (“Raw Honey for Dogs,” WDJ January 2017). Manuka honey is expensive, depending on the strength you purchase. But the healing power is worth the cost.
I used Manuka honey on my 14- year-old Lab/Shar Pei-mix. She had ripped open one of her pads and was having a very difficult time getting it to heal. I used a veterinary-prescribed ointment with fresh bandages as required, while using a boot to provide protection. Two weeks later, with the wound getting worse, I did some research and read reviews of Manuka honey and its healing power. I spoke with my vet and decided to give it a try.
I purchased some that day (strength: MGO 400+) and used it in place of the ointment. I kept the injury wrapped, changing the bandage and refreshing the honey daily, with a boot to protect it. In a week, any skepticism I had disappeared. The results were impressive.
Internally or externally there are huge benefits with its use in both dogs and humans.
Rich Dolphin
via email
I especially appreciate the yearly issue regarding your dog food recommendations. I have noticed that Avoderm is one of the approved products. I once read that avocados shouldn’t be fed to dogs due to the presence of “persin,” causing diarrhea and vomiting. Is this information incorrect?
Marilee Ager
via email
Avocado pits and skin can cause digestive upset in dogs. But the flesh of the avocado can be quite beneficial.
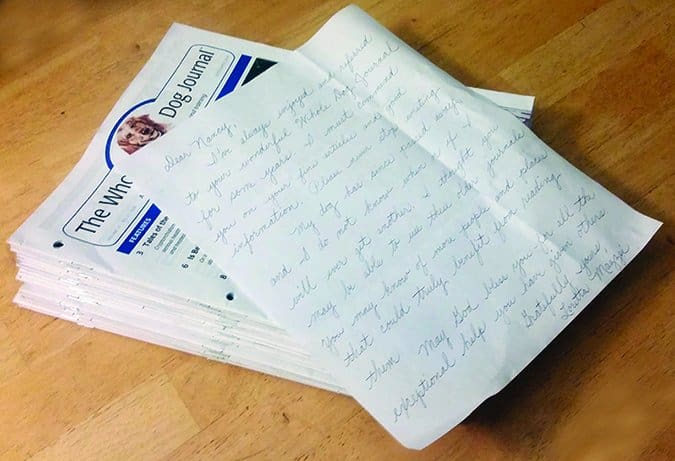
I’ve always enjoyed and have referred to the wonderful WDJ for some years. I must commend you on your fine articles and good information. But my dog has passed away, and I don’t know when or if I’ll get another. I thought you may be able to use these older journals. You may know of more people that could truly benefit from reading them. God bless you for the exceptional help you’ve given others.
Loretta Mazzei
Pittsburgh, PA
That’s so sweet! We’ll ask whether one of the prison-based dog training programs we profiled in “Prison Dog Training Programs” (May 2016) can use them. But we hope you have an opportunity to share your home and heart with another dog.
Raising a Well-Adjusted Puppy
I used to pride myself on the fact that I had never been a so-called “foster failure.” As most of you probably know, that’s what they call you if you take on a foster dog or puppy and, though you had no intention of doing so when you accepted the fostering commitment, you decided to keep the dog for your very own. I took pride in not keeping any of my foster dogs, because the more you keep, inevitably, the fewer you will be likely to foster in the future. After all, not very many of us have unlimited resources of time and money to spend on our dogs.
But a little bit more than year ago, I failed; I fell hard for a pudgy pit-mix puppy I had been fostering, along with eight of his brothers and sisters. Why? Why did I fall for that puppy? For that matter, why would I fall for any puppy? After all, as cute as they are, no one knows as well as someone who fosters a lot how much work puppies and adolescent dogs can be! And prior to taking on that litter, I had absolutely no desire for another dog. At the time, I was already fostering an adolescent American Black and Tan Coonhound named Maebe, and she was annoying Otto, my “heart dog,” to no end. What on earth, I’ve been asking myself for the past year, made me decide to keep this puppy? And what have been the costs to our formerly copacetic canine/human family?

A Puppy Who Is Focused and Connected
In the interest of full disclosure, I usually do develop a preference for one puppy in each litter I foster – but I have never, ever, considered keeping one until this particular favorite pup came along. I noticed early on that the big brindle male pup had extraordinary powers of concentration at the precocious age of four weeks, and boy, do I like that in a puppy or adult dog. I teach all of my foster pups that I will pop treats into their mouths if they sit and pay attention to me, and this pup was the first to retain and actively use this information. When I would work with the group, the big brindle male was always the first to sit down and fix his eyes on my face. The pups with shorter attention spans (and/or less interest in food) would continue to play, sometimes even jumping on the big pup in an effort to get him to return to their games, but the big guy would literally shrug them off, never taking his eyes off of mine. It was as if he were saying, “Get lost, kids; I’m working here!”
He was also the first pup to learn how to follow me down the seven stairs off the back porch into the backyard, and the first to follow me back up the stairs, too. I found that almost every time I tripped over a puppy, it was because that one big guy was on or right next to my foot.
Surgery day arrived, when I took the pups back to the shelter to get altered and then go up for adoption. I kissed their puppy heads, as I always do on the day they “graduate” from foster care, and I said a special goodbye to the brindle boy. Unlike always, I started crying when I said goodbye to that pup, and the shelter workers laughed – kindly – as I walked out of the shelter with tears running down my face, unable to talk. It’s hard, sending those sweet little faces off to uncertain futures! But in most cases, I cheer up over the course of the day, and by day’s end, I’m super happy to be done with puppy pee and poop for a while, and eager to see the puppies’ adoption photos, taken with their new owners, popping up on the shelter’s Facebook page.
In this particular case, however, I stayed weepy all day – so much so that I developed a really bad headache. That’s why I was prone on the sofa, a pillow over my head, when the shelter’s vet tech called me to say that they hadn’t been able to finish all the surgeries for the day, and would I want to take the two males home for another week of fostering? My pillow flew through the air as I flew out the door to go pick up the brindle boy and his only brother, a gorgeous gray pup with pretty pale blue eyes.
When Other Puppies Pale in Comparison

Every time I laid eyes on that handsome gray pup I’d think, “He’s going to go fast! Someone is going to LOVE that puppy.” But that someone was not me; I still was just oddly crazy about the chunky brindle boy. He had the most fantastic eye contact, and even when I wasn’t looking at him, I would often discover that he was looking at me.
One day I watched a video online about “platform training,” wherein a trainer used a little box to help a dog “station” – to help him understand exactly where he should sit, down, or stand (as cued). Just for fun, I got some treats, and started teaching Maebe, my foster hound, to step up onto a little plastic step stool; I thought I might try the platform training with her. The two male puppies were in my office, playing on a dog bed, but when the brindle pup smelled treats, as usual, he came over and joined in the training session; as usual the gray pup did not volunteer. I worked with the hound and the pudgy pup for about five minutes, rewarding them for putting their front paws on the stool, and then I went back to work on my computer.
About an hour later, I rolled my chair back, stretching, and glanced around to see where all my canine charges were. Otto was asleep on a couch in the living room. Maebe was asleep on the couch in my office. The gray pup was asleep on the dog bed next to my desk. And the brindle pup? He was sitting on that little plastic step stool in the next room, looking at me through the doorway. Had he been sitting there for the past hour? I have no way of knowing, but he was just so dogged, he very well might have been.
I didn’t make the decision to keep the puppy that day, but, looking back, that was the moment that clinched it. When I took both male puppies back to the shelter the following week for their surgeries, I filled out an adoption form.
New Puppy Duties
My husband is in charge of naming our pets, and usually I leave the task completely in his hands. This time, though, I asked him to consider one criterion: I wanted him to pick an especially friendly name. Given that the pup was clearly going to have a “bully breed” look, I wanted a name that would counter any tough-guy baggage that can come with those looks; despite the promise of his size, I didn’t want a Thor or Bruiser.
My husband proposed the name Woody, after the beautiful wood-grain look of the puppy’s coat, and I loved it. It evoked the sweet cowboy in the “Toy Story” movies – “I’d like to join your posse, boys, but first I’m gonna sing a little song!”
Of course, it’s just a coincidence, but it’s a funny/sometimes not funny coincidence that Woody has developed a strong predilection for chewing things made of wood, such as chair legs, parts of our deck, rosebushes, apple trees, dog houses, and more. If it’s wooden, it’s been given a speculative chew. I’ve gone through quarts of Bitter Apple (a chewing-deterrent spray for dogs that tastes terrible), which actually does deter the teething adolescent, but usually just makes him go search for something that hasn’t been sprayed yet.
Even with the usual amount of puppy-wrought destruction, though, Woody somehow hasn’t managed to aggravate my husband, who usually likes dogs only provisionally – when they are quiet and well behaved. Oddly enough, Brian likes Woody even though he is not always well-behaved; he’s so full of athletic energy, enthusiasm, and curiosity, he’s always bounding around, into, and through us. But it’s hard to hold a grudge against him, even when you get a fat lip from getting hit by his head when he does a random hop up (a kissing bandit sort of move), because he’s turned into such a genial, goofy guy.
Woody’s “happy dog” demeanor didn’t just happen, however; I’ve been cultivating it like a prize rosebush.
Raising a Pit-Mix Puppy
Again, given the fact that it was clear that Woody was going to grow up into a big, powerful dog with one of those blocky, bully-breed heads, I felt like it was incumbent on me – as it should be on the owners of all similarly big, strong dogs – to take extraordinary measures to make sure that he is well socialized, well trained, and well managed. In July 2016, WDJ published “The 10 Most Important Things to Teach Your Puppy,” by Pat Miller – check those out for a complete puppy checklist. The following are all the measures I’ve personally and deliberately taken over the past year to meet my goal of building a solid canine citizen:
1. Immersed Woody in every puppy fostering opportunity I’ve had over the past year. He’s played “big brother” to four other large litters of puppies that I’ve fostered since he was adopted. This has given him extraordinary social skill, especially with smaller, more fragile dogs. He also finessed his way into the heart of the protective Great Dane mother who stayed with us for months with her litter of 11 puppies. She didn’t like him near the puppies at first, but by the time she got adopted, not only had he earned her approval for puppy-playmate privileges, she liked to wrestle and play with him, too.
2. Enrolled him in puppy kindergarten classes with a positive-reinforcement based trainer, and took him to additional “puppy socials” at the same well-managed facility.
3. Exposed Woody to many other types of animals in controlled settings, taking special care to prevent him from having any opportunity to practice an unwanted behavior even once. For example, I made sure that the first times he saw poultry and livestock, he was on leash, so he never had a chance to see an animal run away from him “by accident.”
4. I sought out opportunities for Woody to meet and hang out with humans of all kinds, and especially babies and children. This is no small feat when you have a dog who looks scary to some people! But I made sure that every interaction he’s had with kids has been enormously rewarding, full of extra-special treats and toys. And it’s worked so far! When he sees a kid, he wriggles with joy and anticipation.

5. I’ve taken Woody into every store in my area that welcomes dogs, and every sort of vehicle I have access to. And I always – always – have treats on hand, so I can reinforce his good behavior, and do a little counter-conditioning if I see signs that he’s getting at all nervous.
The Puppy Adolescent Fear Period
All of this super-socializing might seen excessive to some, but something happened to Woody at about seven months of age that prompted me to put my socializing efforts into overdrive, rather than cruise control. One day, out of the blue, with no precipitating event that I could recall, Woody started raising his hackles and emitting a soft growl when he saw certain people or other dogs. It wasn’t every time, just sometimes, but there was no pattern to it that I could discern. Overnight, he went from happy to meet everyone, to happy to meet most people, and scared to meet some.
I’ve edited enough articles about canine fear-based aggression to know that what Woody was expressing was anxiety, and that the best way to ease a dog’s anxiety was to:
– Increase the distance between the dog and whatever is scaring him, until he can observe the scary thing or person calmly; and
– Counter-condition generously, by feeding him tons of super-delicious treats, in an effort to make him feel better about the situation, without pressuring him for any particular behavior.
I also asked every dog trainer I know personally (and every dog training contributor to WDJ!) about this behavior, and they all said the same thing: “It’s the adolescent fear period. Not all dogs go through it, but any dog can. Keep doing what you are doing.”
We’ve been doing that, and it’s working. Woody has mostly come out the other side of this tunnel of fear, and rarely growls or raises his hackles upon seeing people he doesn’t recognize. I’ll tell you more about our continuing efforts to work through this unexpected challenge in a future issue. If you are seeking more info on puppy socialization now, read Denise Flaim’s article, “Properly Socializing Your Puppy“.
Nancy Kerns is editor of WDJ.
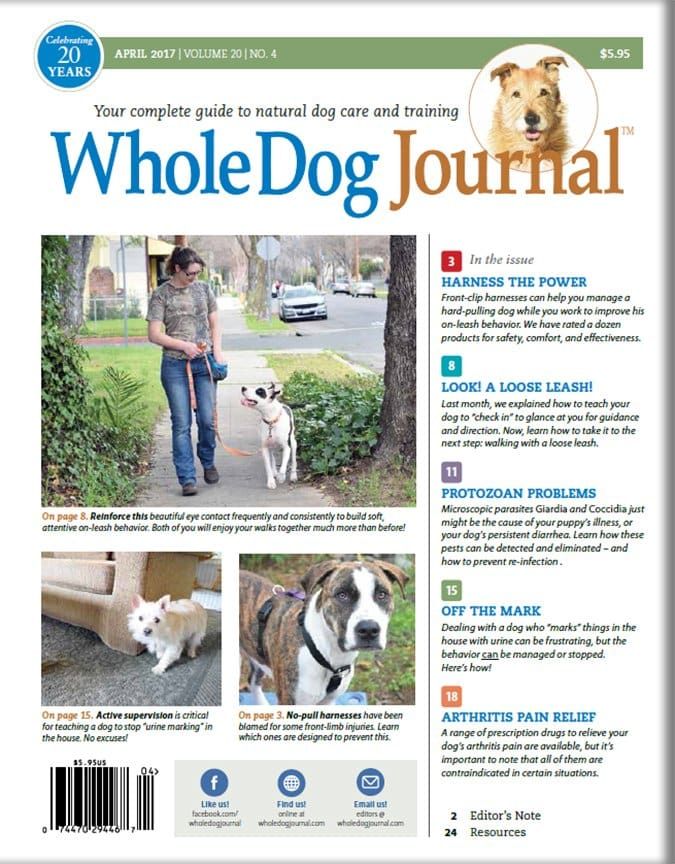
Whole Dog Journal’s New Look

I couldn’t be more excited about the changes you will see in this month’s issue of WDJ, not least of which is the new illustration of a dog on the cover, which was based on a photograph of my nine-year-old mixed-breed dog, Otto! Nepotism may have gotten Otto the spot, but I honestly think he serves as a perfect representative of what WDJ is about: a vibrantly fit, happy, intelligent, confident “everydog.”
I shouldn’t sound critical of a dog who has been such a hard-working member of the WDJ family for so long, but I never really gave my heart to the Golden Retriever who used to appear in the Journal’s logo. I always wanted him to lose some weight, and show a little more enthusiasm for the job.
We’ve also added a little more color and a little more air to the pages, modernizing the entire look a bit. It’s time! With this exact issue, WDJis 20 years old, after all!

It’s hard for me to believe this is our 20th year. For me, time has just flown by; this has been such an exciting time to be involved with dogs. In the two decades since the first issue of WDJ was published, training dogs with positive reinforcement has gone from being a novelty to the mainstream training method of the most committed, educated dog owners and trainers. Today, there are entire generations of trainers and dog owners who have grown up training with only flat collars and classical conditioning, variable schedules of reinforcement, and other humane, effective training tools.
Canine nutrition and holistic healthcare, too, have been revolutionized during WDJ‘s time in print. There are hundreds of good dog foods to choose from today; when we started the Journal, there were fewer than 10 that met our existing selection criteria. I could go on and on – and I hope to! – for years to come. I hope you’ll come along; there is still much more to learn!
Recall Notice for Evanger’s Canned Beef Dog Food Variety
On February 3, 2017, the FDA announced that Evanger’s Dog & Cat Food had recalled five lots of its canned Hunk of Beef dog food, for a “potential contaminant,” pentobarbital. One dog has died as a result of eating the contaminated food. Evanger’s canned food appeared on WDJ‘s “approved canned dog foods” in our October 2016 issue. Evanger’s makes its own canned foods, and is blaming its meat supplier for the problem.
Evanger’s dry foods, which appear on our “approved dry dog foods” list in the February 2017 issue, are produced by a contract manufacturer and are not involved in the current recall. For breaking news on pet food recalls, see the U.S. Food & Drug Administration website.
For active coverage from Whole Dog Journal, see my blog post about the recall, and check back for weekly updates.
Make Vet Visits Less Scary
[Updated August 24, 2018]
Vet visits can be stressful for the beings on both ends of the leash! As my dog sits in the waiting room, awash in trepidation, I, too, am often worried about what decisions I’ll need to make regarding diagnostic testing, what it’s all going to cost, and the pros and cons of every possible scenario – all while battling an overall concern for my dog’s physical and emotional health.
Veterinary care is a necessary part of responsible dog ownership, and, fortunately, a little pro-active planning and thoughtful training can help reduce vet-related anxiety for both dogs and their owners. The following tips will help prepare you and your dog for your next trip to the vet’s office.
1. Research your ideal veterinary care for your dog.
Do you have strong opinions about certain facets of animal care? Do you believe in feeding a raw diet or waiting until a certain age to spay or neuter? Do you prefer exploring holistic heathcare modalities in place of more conventional Western medicine approaches? Where do you stand on vaccinations? How do you feel about chemical flea and tick preventatives?
While the ability to use Google does not make you an expert, it’s perfectly fine to have strong preferences for how you want to address your dog’s healthcare needs. There’s space in this world for many opinions! That said, it’s wise to work with a vet who shares (or at the very least respects) yours.
Stephanie Colman

When looking for a veterinarian, ask local dog-owning friends which veterinarian they use and how well they like both the vet and the practice in general. If you’re new to the area and can’t rely on personal referrals, consider using the American Animal Hospital Association’s accredited hospital locator search tool to begin your search.
When considering a certain veterinary hospital, calling the office or viewing the practice’s website can answer questions such as where the staff refers its critical care or after-hours cases, whether or not the office is staffed overnight, or if the doctors are available on call. These are all good things to know early on when developing a relationship with your vet.
Office staff likely won’t be able to speak in detail about an individual doctor’s philosophies and approaches to care, nor will the doctor have time to field a lengthy interview call, but you can schedule a basic exam visit to serve as your chance to get your general questions answered, while allowing you the opportunity to experience the vet’s bedside manner.
AAHA Veterinary Accreditation
The American Animal Hospital Association is the only accrediting body for companion animal hospitals in the United States and Canada.
“Accreditation is voluntary. The hospitals are inviting AAHA in to evaluate how they practice,” says Heather Loenser, DVM, veterinary advisor of professional and public affairs for the American Animal Hospital Association. “Vets don’t have to do this. That’s why accreditation is a big deal, because you know you’re going to a practice where the staff wants to be excellent and wants external feedback from leaders in the field.”
When a veterinary practice applies for accreditation, the practice is evaluated on approximately 900 standards of veterinary care, ranging from pain management, infectious disease protocols and anesthesia safety to customer service procedures and how medical records are maintained. Facilities are re-evaluated every three years and must pass each time in order to maintain accreditation. The AAHA estimates that about 12 to 15 percent of veterinary practices throughout the United States and Canada are accredited.
“You can still practice excellent medicine and not be accredited, but I think pet owners will notice a difference in team work, pride and high morale of the staff in an accredited hospital,” Dr. Loenser says. “The veterinary teams who want to go through accreditation tend to hold themselves to a higher standard – they’re often the Type A of the Type A kind of people.”
For more information, visit www.aaha.org.
2. Plan for the cost of your dog’s veterinary care.
Nobody likes to be hit with an unexpected vet bill, but accidents and illnesses happen, and it’s important to be prepared. Pet insurance can be a great way to ease the financial sting of costly vet bills. Today’s pet insurance market is broad enough to offer a variety of coverage levels, ranging from plans designed to cover major emergencies with relatively high deductibles and lower monthly premiums, to more comprehensive plans including wellness coverage and lower deductibles, but with higher monthly premiums. Like any insurance, pet insurance can feel like a gamble. We hope we never need to use it, and when we don’t, we might grumble a little when paying the premium. At the same time, it’s a relatively inexpensive way to secure the peace of mind that comes with knowing you are better prepared, financially, to provide for your pet’s medical needs.
If insurance doesn’t feel like the right choice for your family, consider establishing and funding a separate savings account specifically for your pet’s unexpected medical issues. There’s also CareCredit, a credit card designed specifically for heath care financing, which offers 0 percent interest for 6-24 months on an initial medical charge of at least $200. (Even with pet insurance, I’ve personally used CareCredit several times.) Be warned: If you exceed the promotional period, CareCredit carries a whopping 26.99 percent interest rate.
3. Don’t wait until your dog’s minor illness or injury becomes a major one.
To go or not to go to the vet can be a stressful decision. The stress rate skyrockets after normal business hours when your regular vet is closed and you’re considering the nearest emergency facility.
It can be tempting to take a wait-and-see approach to seemingly minor medical issues. This isn’t always a bad choice, especially when you’re familiar with what’s normal for your dog, and in a position to closely monitor him for changes. Generally speaking, I don’t rush my dog to the vet the first time he vomits, has an episode of diarrhea, or seems somewhat lethargic; I’ll keep an eye on him and watch for other potential problems.
However, not all vomiting, diarrhea, and lethargy are created equal; it’s important to pay attention to the big picture. Vomiting and lack of appetite in an otherwise alert, bright-spirited dog could indicate nothing more than his body attempting to rid itself of a dietary indiscretion. Vomiting along with drooling, panting, and general restlessness is a classic sign of bloat, which is an immediate veterinary emergency.
It’s one thing to feel confident in your ability to manage minor issues that crop up after hours in an effort to avoid the higher cost of emergency care. Good old-fashioned pragmatism definitely has its merits. But the truth is, waiting often makes things worse; for example, taking a “wait and see” approach with a dog’s limp, thinking it is due to a soft-tissue injury, when the limp actually resulted from a slipped disc, can result in a drastically worsened injury. By the time you realize it’s not getting better, a dog in this situation could be facing paralysis and you’d be facing a much higher vet bill.
4. Familiarize your dog with the veterinarian’s office before your next appointment.
If your dog visits the vet’s office only when he has an appointment, there’s a much stronger chance he’ll log the experience in the “Bad Stuff!” category, even if you’re lucky enough to mostly only need routine wellness visits. (I mean, have you seen where they often put the thermometer?)
The floor is slippery, everything smells different, and you sometimes hear distressed animals vocalizing in exam rooms or crating areas. Plus, the “strangers” in the vet’s office don’t want to just to pet your dog – they often need to physically restrain or hold her in position during an exam or procedure. This can be frighteningly invasive for even the most easygoing dog during the best-case scenario. Factor in not feeling well or being in pain, and it’s no wonder why many dogs hit the brakes in reluctance as you attempt to walk into the office. Unfortunately, this fear often builds on itself over time, causing some dogs to progress from being mildly concerned to extremely anxious, or even completely panicked during a visit.
A simple way to help prevent or reduce vet-related anxiety is to visit the office when your dog doesn’t have a medical reason to be there.
Pay attention to where the visit first starts to seem scary for your dog and start there. If his nerves flare up during the walk from the car to the front door, hang out in the parking lot, offer delicious treats, play a game of tug if your dog likes toys and then hop back in the car without ever going into the office.
If he’s fine until you reach the doorway, plan your party for the area just outside of the office, being careful to stay out of the way of clients coming in and out. After a short fun-fest, return to the car, where you can either wait a few minutes and go play again, or simply drive home, depending on your schedule.
Veterinarian waiting room jitters
If your dog’s behavior tells you it’s the waiting room and beyond that trigger his nervous tendencies, happily engage your dog as you walk from the parking lot to the reception area. Offer “freebie treats” in support of your dog’s positive attitude (to further strengthen your dog’s association with the parking lot as a safe place) and ask for simple behaviors along the way.
I typically ask for (and reward) several “sits,” a hand-touch or two, and a few “spins” just on the short walk from the car to the front door as I head into the office with my dog, Saber. The more I can keep him using his thinking brain, the less likely he is to succumb to the overwhelming feelings of his emotional brain.
Once inside the waiting room, allow your dog to investigate, so long as his activity doesn’t interfere with other clients. I like to alternate between allowing my dog to look around and asking for simple behaviors, as his ability to focus on my requests tells me a lot about his emotional state. If he’s unable to focus on my requested task, he’s telling me he needs more time to acclimate. The same applies to dogs who generally enjoy treats, but who might refuse them in the waiting room.
Note: If your dog refuses food for more than a few minutes, he’s likely too far over threshold, and you should start at an easier level – just outside of the office or in the parking lot.
Invite your dog to hop on the scale to be weighed. It’s important that your dog cooperate with being weighed, since medication dosages are calculated by weight. When getting weighed requires physical restraint, the greater the risk of an inaccurate reading.
Have a seat and simulate waiting to be called for your appointment. Offer treats, calm petting and praise throughout the experience. If your dog is at all hesitant, it’s wise to end the visit here, and repeat the experience on another day. If he’s handling the waiting room in stride, and the staff isn’t super busy, ask a vet tech or member of the office staff to offer your dog treats (only if your dog is comfortable with strangers). They might even be willing to escort you to an exam room where you can continue your “just for fun” visit against the backdrop of a more formal appointment. Feed a few more treats, ask for a simple behavior or two, present a favorite toy, then cheerfully exit, remembering to thank the staff for their help.
When planning your social visits, it’s helpful to call ahead so the staff knows what to expect when you arrive, and to make sure you don’t walk into an exceptionally crowded office.
Social visits are a wonderful way to help a puppy or young dog create a positive association with the vet’s office as well as help counter any negative emotional baggage following an especially unpleasant vet visit. Taking the time to plan emotional training sessions away from necessary visits can help reduce stress levels in adult dogs, too.
Admittedly, this isn’t always the most convenient training session, since it requires travelling to the vet’s office, but as responsible, compassionate dog owners, we owe it to our canine friends to look after not just their physical health, but their emotional health and well being, too.
5. Teach your dog calm acceptance of being handled and restrained.
So much of what goes into a vet examination or medical procedure can be made easier for your dog when he’s familiar and comfortable being handled in myriad ways. Make it a habit to touch your dog all over his body as part of your everyday affection and relaxation routine. Rub his belly. Massage his leg muscles. Gently play with the inner and outer part of his ears. Massage his feet. Run your hand from atop his head toward his muzzle.
Handling your dog in this way helps normalize the experience of being touched, which can help make handling in other circumstances, like at the vet or groomer, less concerning. It’s also a great way to familiarize yourself with your dog’s topography so you’re more likely to notice a change, such as the development of or change in a lump or the sudden appearance of a rash or other skin irritation.
Pair certain types of handling with treats to help your dog build a positive association with those experiences. This is helpful for dogs who have an demonstrable aversion to being touched certain ways, as well as dogs who appear fine with the handling when at home with their owners. Taking the time to pair handling with treats, even with cooperative dogs, helps ensure against the normally “fine” behavior degrading and becoming an issue when the dog is distressed. It’s one thing to be “fine” with having your feet handled by your owners, in the safety and security of your own home. It’s a whole different story when you’re being held by strangers, in an unfamiliar place, and are in pain from an injury.
When using food to create a positive association with different types of handling, ideally you present the handling in a way that prevents the dog from feeling uncomfortable and then present the treat, rather than feeding treats simultaneous with the handling. For example, if a dog is uncomfortable with having his feet held, you might start by touching the top of one foot with two fingers, for one second, and then feed the treat. This helps make sure the dog is associating the act of being touched with earning the cookie. When feeding simultaneously, it’s easy for the presence of the food to override the handling you’re teaching the dog to enjoy. (That said, choosing to feed treats throughout an event your dog might find unpleasant is a perfectly valid way to manage the situation, in hopes of minimizing the potential for negative emotional baggage.) Slowly build toward the finished behavior, increasing your effort only when the dog can calmly tolerate the easier step.
When it comes to paw handling, it’s well worth taking the time to teach your dog to comfortably cooperate, as many vet experiences include needing to hold a dog’s feet – from the obvious such as nail trimming and foot injuries, to the less obvious, but common need to hold a dog’s paw during blood draws and when inserting IV catheters.
It’s also important to teach your dog to enjoy handling by other people. If he’s already comfortable being handled, or once you’ve desensitized him to being touched in any tricky spots, instruct your friends on where and how to handle him as you supply treats at the correct time. This will help generalize the behavior to other people.
In-office handling also often requires restraint. Teach your dog to be comfortable when you lean slightly over and into him, holding him tight to your body. Practice securing your dog’s head. When training, always start with super-short trials of just a few seconds, at a level that doesn’t appear to cause concern, followed by the delivery of a treat.
Even if your dog lets you do all of these things, there’s still value in taking time to build strong, positive associations through further training to ensure against behavior degradation during difficult times. Think of the training time as a way to help inoculate your dog against future stress!
If your dog has handling issues, or if you want to be extra prepared, teach your dog to wear a comfortable muzzle. Even the most accepting dog is apt to struggle if a foreign object is suddenly thrust upon him.
Strengthen your dog’s basic cues.
Finally, don’t underestimate the value of basic skills such as a solid “sit,” “down,” and “stand,” and the ability to relax on his side (whether you call it “chill” or “play dead”) as ways to control your dog’s body. A nose-bump hand target or duration target behavior is another great way to cooperatively guide your dog into position during an exam. The better your dog is at responding to basic cues in the vet’s office, the less he will need to be physically manipulated throughout the visit.
When working on vet-related issues, it’s important to remember behavior is fluid. It’s not uncommon to take three steps forward, then two steps backward, especially following a challenging vet visit. The good news is, once initial progress has been made, that foundation work often makes it easier to recoup benefits via additional training, even following a setback.
SUCCESSFUL VET VISITS: OVERVIEW
1. Find a veterinarian with whom you agree on issues that are important to you regarding your dog’s care.
2. Have a financial plan for unexpected veterinary expenses.
3. Protect your dog from unnecessary added stress by teaching him to comfortably accept handling common to vet visits.
Stephanie Colman is a writer and dog trainer in Southern California.
Train Your Dog to “Check In”
“CHECK-IN” TRAINING OVERVIEW
– Help your dog develop a habit of checking in with you. Start where he won’t easily be distracted.
– Reward your dog each time he spontaneously glances at you throughout the day.
– Prepare some small yummy treats in advance and put your dog on leash. Stand quietly and mark and treat every glance toward you until your dog is focused on you.
– Take the game outside in a low-distraction area. Mark and treat any effort your dog makes to pay even the slightest attention to you. Be patient.
– Practice stepping outside with your dog so he learns to look at you and wait while you lock the door.
– Make it easy for your dog to choose to pay attention to you, so he gets as many opportunities for reinforcement as possible!
Recently, while out walking with a friend and my dog, Chili, my friend noted that Chili often turned to glance toward me and she asked, “Why is she doing that? Is she afraid to lose us?” I chuckled and answered “Not at all. She’s just learned to check in with me now and then.”
Chili is walked on a leash, but she is free to follow her nose, and interesting odors often lead her to a position that is several steps in front of me or farther off to my side. I don’t mind at all, and in fact, I encourage lots of sniffing during our walks. My only requirement is that she keeps the leash nice and slack, and that she checks in with me frequently.
Checking in is one of those behaviors I like to place in the “habit” category; I want my dog to offer it easily and without really thinking about it.
The purpose of the “check in” behavior (why or when a dog may do it) varies, but it always looks like this: The dog momentarily connects with her human through eye contact. Chili and I have gotten so good at it that we often find ourselves turning toward each other simultaneously! I absolutely cherish those moments of instant, genuine connection with my dog.

4 Good Reasons to Encourage Your Dog to Look at You
The utility of having a dog who regularly checks in with you is undeniable. Communication is a two-way street, and checking in facilitates communication between your dog and you. Take, for example, the following circumstances in which Chili has learned to check in with me:
1 If she is unsure what to do in a given situation, Chili will check in with me by glancing my way and seeking eye contact for guidance. For example, faced with the unexpected rapid approach of a stranger, she might look to me for instructions on how she should respond. “Friend or foe? Should I worry? What’s your take on this situation?” I might ask her to come closer to me, or I might let her know it’s okay to go and say, “Hi.”
2. If she needs my help with something, she’ll check in by looking at me. If I’m not near her, she’ll seek me out. For example, if a toy has rolled under the couch and she can’t reach it, or if she wants the door to the backyard opened, Chili will capture my attention with eye contact in order to seek my assistance, rather than sitting and staring intently at the toy or the door, or whining or barking at the toy or the door.
3. If she wants to eat something. For example, if an item that looks like it might be edible unexpectedly falls to the ground – she’ll check in with me before diving in to gobble it up. That has proved especially useful on many occasions!
4. Before crossing a road or turning in a new direction. If I haven’t already let her know what I intend to do (by asking her to “Stop here,” “Keep going,” or turn “This way”), she’ll look toward me for clarification.
Reinforce Your Dog’s Check-In Early
In the early days when I first adopted Chili, I reinforced any eye contact she offered me as a way to start building a bond between us. I would simply say, “Yes!” whenever she looked at me and I’d follow up immediately with a small treat. It didn’t matter what else she might have been doing at the time – whether she was sitting, lying down, standing, walking, or even barking! My only goal at that time was to make it very clear to her that if she paid attention to me, good stuff would happen for her.
More importantly, I wasn’t soliciting this attention by calling her name or attracting her with sounds or movement. Instead, I made a point of reinforcing as many spontaneous gifts of attention that I could capture – and I do consider attention from my dog a gift!
It wasn’t long before Chili developed a beautiful habit of seeking eye contact with me for a reward. Once we’d established that simple rapport, it was easier to start training the behaviors I wanted Chili to learn. Checking in was especially useful when teaching her to walk nicely on leash. It also played an important role in teaching a solid recall.
But before tackling advanced behaviors like loose-leash walking, it’s much more useful to start with the basics.
How to Teach Your Dog to “Check In” With You
Whereas at first I would reward Chili for just glancing my way without any solicitation on my part, I soon started adding some distractions and accessories in order to start teaching her some more complex behaviors.
Whenever you decide to teach a behavior that you’ll need your dog to know while in high-distraction areas (like outside on the street or at a park), the first step is always to start training in a low-distraction area in order to build the foundation skills. As your dog becomes accomplished in the low-distraction areas, you’ll be able to gradually make the learning sessions a bit more challenging by adding distractions. This is how your dog will acquire the skills needed to succeed: Start easy, and gradually make your way toward the more advanced levels.
I wouldn’t expect a dog with little or no loose-leash walking skills – and with only beginner check-in habits – to be able to remember to connect with his human while out walking. Who could blame him? There are just too many things vying for his attention out there!
Here’s how you can use the check-in behavior to improve your dog’s leash-walking skills:
1. While inside your home, prepare some small yummy treats in advance and put your dog on leash. Simply attaching the leash is often enough to excite some dogs, and he might start pulling toward the door, anticipating a walk. Stand still, remain calm and wait him out.
2. Watch your dog carefully and mark the slightest glance in your direction with a clicker or with a verbal signal, such as the word “Yes!” and give your dog a treat.
Try to deliver the treat close to your own body rather than reaching forward toward your dog. I personally prefer to drop the treat on the floor right next to me, but later on, when we take the exercise outside, that might not be possible because of the surface of the ground (there might be snow, mud, rocks, etc., making it more difficult for my dog to find the treat or to successfully pick it up). In that case, I’ll deliver the treat directly to my dog’s mouth, but close enough to my body to encourage her to stay near me.
3. Keep marking and giving a treat for every glance, until your dog is focused solidly on you. For most dogs, this won’t take long! The realization that there is a steady source of treats available is often a very powerful motivator for dogs to focus happily on their human.
4. Take the exercise outside, in an area with few distractions (more distractions than indoors, but not as many as walking on a street or in a park). A backyard, porch, balcony, or deck will do nicely.
Let your dog listen to the sounds around him, let him look around, let him sniff the air. Just as you did indoors, stand still and quiet, keep your eye on him, and mark and treat every glance he throws your way. Let him return to listening, seeing, and sniffing the air around him (while staying in one place).
Keep practicing this exercise until he’s offering you attention on a regular basis – not necessarily staring at you, but checking in with you frequently. Now you’re ready to add some distractions.
5. Go back inside and this time, take your dog out through the door you would normally use to go for a walk. Close the door behind you. (If you live in an apartment or condo, you’ll do this step twice – once outside your unit door, and once outside the main door to the building.)
Stay put next to the door. Chances are, your dog will already have begun pulling toward the street. Hang on, remain calm, and wait him out. Immediately mark and treat the slightest glance your way, and continue marking and treating any attention your dog offers you.
If you find it’s taking rather long for your dog to glance your way, encourage him by making a sound (like a kissy sound) the first couple of times just to get the ball rolling. After that, see if you can wait him out again.
Remember to mark and treat any effort to pay even the slightest attention to you. You want your dog to have as many opportunities for reinforcement as possible.
6. When your dog appears to be calmer and better able to offer you some attention just outside the door, go back inside. Keep your dog on leash and play the attention game just inside the door for a few seconds, then go back outside and repeat exercise #5.
You can play this in-and-out game a few times. Your goal is to be able to step outside and have your dog looking to you in anticipation of a treat, rather than bolting for the street.
Imagine how useful this real-life behavior will be when you need a free hand to lock the door behind you as you leave!
During the learning process, mark and treat every single time. Later, when your dog is offering this behavior reliably, you’ll be able to taper the treats and the reward will be to move forward. But for now, reinforce heavily with food.
Nancy Tucker, CPDT-KA, is a full-time trainer, behavior consultant, and seminar presenter in Quebec, Canada.
Dog Parkour: Canine Urban Athletes
[Updated February 7, 2019]
BEGINNING DOG PARKOUR OVERVIEW
1. Visit the International Dog Parkour Association’s website to learn more about this fun sport.
2. Explore new areas with your dog. Be creative! Encourage your dog to interact with the environment while practicing basic obedience and parkour skills.
3. Once your dog understands what to do with a certain obstacle – whether that’s jumping over, running under, or jumping up on it – see if you can “send” him to perform the same exercise from a distance.
4. Ask for more challenging behaviors only as your dog tells you he’s ready. Be patient while working on new behaviors – and remember to always keep it fun!
The tiny terrier confidently ascends the park bench at her handler’s request while the sun shines down on a warm Southern California day. There she sits, clearly enjoying the interaction with her human, and happily cooperating with the task at hand. The treat she’ll earn after hearing her release word isn’t bad, either.
For Delilah and Elisa Becker of Simi Valley, California, and countless teams like them, this type of activity transcends being a creative way to add pizzazz to a daily walk – they’re working toward a title in a fun new sport: dog parkour.
Parkour for Dogs: Fairly New, Very Fun
Dog parkour is the Fido-friendly version of parkour, sometimes called “free running,” a type of outdoor gymnastics. In the human version, enthusiasts (called “traceurs”) run, climb, leap, and swing their way through an improvised course of obstacles in the environment. Success in parkour is about discipline, not just daredevil tendencies; safety is of the utmost importance, and participants take great care to develop proper cardiovascular conditioning, strength, and body awareness.
Stephanie Colman

The sport “went to the dogs” in 2014, when established traceurs and dog trainers Karin Coyne and Abigail Curtis, DVM, of Reynoldsburg, Ohio, noticed how many unique obstacles in their everyday environment were accessible to dogs. They started experimenting with their own canine companions and quickly added parkour-themed classes to their training offerings. From there, the International Dog Parkour Association, (abbreviated IDPKA, since traditional parkour is often referred to as “PK”), and a new titling sport was born.
Coyne says dog parkour is a great way to get any dog-handler team out of the house, but it’s an especially nice option for owners whose dogs struggle with reactivity in a traditional group setting, or in areas where group classes are few and far between.
“For us, one of the best things about dog parkour is how it helps improve a dog’s confidence and focus as they explore new things,” Coyne says. “For the people, it gets them out, too. A lot of owners wouldn’t investigate a neighborhood park on their own, but once they start parkour, they’re looking for new areas to explore.”
Dog Parkour Rules and Requirements
Dog parkour involves a variety of skills, which must be executed in increasingly difficult ways in order to earn progressive titles.
Conceptually, the most common behaviors require putting four feet on an object, four feet in an object, jumping over an object, passing through a gap in or between objects, balancing on narrow objects, and moving away from the handler to go around an object.
It may sound easy, but Becker says even the seemingly simple concepts helped uncover some “holes” in her training.
“I took for granted that, because Delilah is constantly jumping up on things on her own, she’d know what I meant when I asked her to ‘jump up,'” Becker says. “I also discovered she didn’t like jumping into things. The ‘four feet in’ behavior was initially the hardest for us. I wasn’t expecting that.”
The IDPKA currently offers five titling options ranging from a training-level title (PKD-T) to a championship title (CH-PKD), all awarded based on a thorough review of handler-submitted videos and an accompanying submission fee of $20 to $40.
“I love being able to video our work and submit for a title,” Becker says. “It makes me less nervous, and gives us a chance to practice first and submit the best version of the performance. The only challenge with video is making sure we both stay in frame and I’m not blocking the camera.”
Traditional dog sports such as obedience, rally, and agility specify exactly how required elements must be executed, but dog parkour requires creativity and an eye for the environment, wherever you are – whether in a city or rural landscape. Park benches, utility boxes, playground equipment, tree stumps, decorative railroad ties, and more can easily become part of the parkour experience. How exactly your dog executes a “four feet on” behavior is limited only by your imagination, safety considerations, and your dog’s willingness to perform as requested.
“It’s creative and completely adjustable,” Coyne explains. “A young dog or older dog might put his feet on a six-inch obstacle; other dogs train for more of a challenge. Every dog can participate in some way.” Required elements can even be modified to allow for the safe and confident participation of dogs with disabilities.
To date, IDPKA has awarded nearly 250 titles to teams, mostly at the novice level. While the majority of title-holders hail from the U.S., teams from Canada, Denmark, United Kingdom, Sweden, and Australia have also completed title requirements.
Safety Comes First in Canine Parkour
Safety and choice – on the part of the dog – are at the heart of IDPKA’s program.
“If you try to force or lure or do anything to make the dog feel like he has to perform a behavior, it can become dangerous, because the dog isn’t freely choosing to participate,” Coyne says.
“It’s important to emphasize choice, start small, and work your way up. At the novice level, things are small – ground level. The dogs build strength and coordination, and the handler learns to properly ‘spot’ the dog to make sure he remains safe throughout the exercise.”
That’s not to say training lures are completely discouraged in all aspects of dog parkour. Coyne acknowledges how, in a team’s early training, lures can be helpful in establishing a dog’s understanding of conceptual behaviors such as “jump up” or “go under.”
“It’s one thing to lure a new dog up onto a low rock when first training,” she says. “But by the time a handler is ready to ask her dog to jump atop a tall wall, the dog should understand the cue and feel confident in his ability.” To that end, once working on a title submission, food or toys can be used only as rewards following the successful completion of a behavior, not to initiate or guide behavior.
In promoting the safe execution of urban obstacles, dogs must wear well-fitting back-clip harnesses, and handlers must make responsible decisions regarding the choice to work on- or off-leash, depending on the environment.
Dogs are never allowed to jump down onto a hard surface from higher than shoulder height. Instead, they must be carried, lowered, or shown an alternate exit strategy. Submission videos must clearly show the dog ascending and descending each obstacle. Handlers must demonstrate an understanding of proper spotting in order to assist their dogs as necessary. Most importantly, dogs must perform all obstacles independently, of their own free will, and with confidence.
“We like to see dogs who are confident, who understand where their feet are, and who are in a situation where, if something happened, the handler could immediately help,” says Coyne.
When a submission fails to pass, it’s usually for safety reasons – either the handler allowed a dog to jump down from a height exceeding safety guidelines, the handler wasn’t in a position to properly spot the dog, or the dog looks uncomfortable while performing the obstacle.
Expanding Your Dog’s Horizons with Sport
As a trainer, I’ve always been a fan of incorporating elements found in the environment into my daily dog walks. Random objects are great for helping dogs generalize behaviors while adding novelty to otherwise routine outings. For many people, the opportunity to work toward a title provides the motivation they need to brainstorm new things to train. Of course, time spent training strengthens the dog-human relationship, while helping to create and maintain a well-trained dog who is a joy to have around.
With the growing popularity of dog parkour, a little creativity, a video camera, and the Internet can help turn any dog into a titled urban athlete! Best of all, Elisa says, “It’s fun. That’s exactly how I feel all training should be – fun. If the dog isn’t having fun, there’s no reason to do it.”
Our thoughts exactly.
Things Whole Dog Journal Loves About Parkour for Dogs:
- If it seems that coercion or force was used to get the dog to perform an exercise, the performance will not be awarded with a title.
- Safety is stressed at every level. Strength and coordination are built slowly. The handler has to know how to and be able to support and catch the dog, preventing falls.
- Dogs who look confident and in control of their movements do well; wild attempts at exercises will not earn titles.
- Handlers don’t have to travel to events to earn titles; video submissions are judged instead.
Stephanie Colman is a writer and dog trainer in Southern California.