Download the Full June 2020 Issue PDF
Making Sure Your Dog is Comfortable with Alone Time
I’m incredibly fortunate to have had a career that has allowed me to work from my home for the past 25 years or so. If you are new to working from home while sheltering in place (and, perhaps, also caring for children), you may be one of the thousands of people who observed that your dog was thrilled to have you home all the time. And he or she probably got more walks, too!
But as this issue goes to press, and states are beginning to reduce the sheltering in place restrictions, you may be worrying about how your dog is going to respond when you get to (have to?) go back to work or school. If this is you, we’ve got your back. Our Training Editor, Pat Miller, explains how to make sure your dog adjusts smoothly to your absence.
Food-filled Kongs and other food-dispensing toys are frequently prescribed by trainers – and, indeed, by us, too! – for helping dogs pass the time they have to spend alone. The idea is to give them something enjoyable to do, so they are less tempted to be destructive or worried about when you might return. But you should be aware that these food-filled toys and tools are not a panacea! Eileen Anderson describes some potential hazards associated with using food dispensers as dog-sitters.
I’d like to add something to the discussion. Pandemic quarantines aside, it’s always a good time to teach your dog to be comfortable and content at home without you. This goes double for newly adopted dogs and foster dogs, and it goes triple for puppies. Teaching your dog that he can relax when you leave him is a valuable life skill, and, since most of us can’t be with our dogs all day, every day – not even me, and I always work at home! – it enhances the quality of his life. You want him to feel safe and secure when you’re gone, don’t you?
I’m aware that a lot of us feel better when we’re with our dogs than when we are without them – and that some people depend on their dogs as emotional support animals. But even those people – perhaps especially those people! – should be sensitive to the idea that cultivating a dog’s emotional dependence on being with people is unfair, maybe even cruel.
I have a number of friends whose dogs suffer from separation anxiety, and that’s exactly the correct word, “suffer.” These dogs are not just uncomfortable, they are in absolute, being-branded-by-hot-coals agony when their owners leave.Their owners have spent countless hours working through training protocols meant to s-l-o-w-l-y improve the dogs’ ability to be left home alone without tearing themselves or their homes apart. Every dog owner should strive to prevent this traumatic disorder from developing if they possibly can.
Helping Dogs Adjust to Being Home Alone Again
Though many people who have been sheltering in place for weeks report being confused as to the day of the week, I have been getting confused about the date every month during a certain time of the month for the past, oh, 30 years or so. For the past 23 years, the cause of this is the monthly publishing schedule of Whole Dog Journal, and prior to that, it was the monthly publishing schedule of a variety of other monthly magazines.
You see, in late April/early May, I have just sent the June issue to the printer. Shortly after I send the June issue files to the printer, they start processing the files, printing the magazine, sorting the mailing file, and ultimately mailing off the hard (printed) copies of the magazine to our subscribers. During the same time, the staff at our publishing headquarters is downloading my files and turning the pages and art I created into the online version of the magazine. In a few weeks, usually about a week before the start of the month named on the cover, all of the work at the printer and post office and publishing headquarters is done, and the subscribers get to enjoy the issue that I finished a month prior.

Again, back in that late April/early May zone, I’ve shipped the June issue and begun work on the July issue. It’s around this time that people start commenting on or asking me about articles that were in the May issue. Problem is, by this time, I have trouble recalling what was even in the June issue, much less the May issue! And if you ask me what month it is right now, I sometimes have trouble answering!
Returning to work? Prevent separation-related behaviors.
However, I wanted to let you know about a couple of articles that will appear in the June issue, even though it won’t be in your hands for another week or two. The articles address a concern that many people are worrying about right now, as many states are loosening shelter in place guidelines and many people are going back to work: helping dogs adjust to being home alone again. Our Training Editor, Pat Miller, has written an article that discusses how to recognize and prevent separation-related behaviors (SRBs) – including separation anxiety, which is one particularly serious type of SRB.

Lots of owners rely on food-stuffed Kongs, slow-feeder bowls, snuffle mats, and other food-dispensing toys to occupy their dogs and help them fill the time when they are gone. Eileen Anderson, a more recent addition to our stable of contributors (she wrote the in-depth discussion of apps that are sold as tools for desensitizing sound-sensitive dogs which appeared in the March issue), discusses food-dispensing toys and tools in the June issue. She notes that some of these tools do more to frustrate some dogs than they do to help them fill their time in an enjoyable way. Anderson discusses ways to make sure that the tools or toys you use actually do help your dog reach the food in a way that helps them feel rewarded, not annoyed.
If you live in a state that is reopening NOW, I’m sorry you have to wait for another week or so to access these articles! We started preparing them the minute we thought of the idea.
New World Order, Puppy Edition
In a world where maintaining safe social distances is going to be the new normal for a while, there are a number of dog-related transactions between people that have been altered.
Covid-19 has changed things in the world of dogs
Veterinary hospitals are sending masked and gloved assistants out to parking lots to collect and return patients, and taking credit card payments over the phone from the parking lot; no clients enter the veterinary hospitals. I’m hearing about daycare providers and groomers who are building “airlock” entrances, where clients enter a small enclosure with their dogs, closing a gate behind them, take off their dogs’ collars or harnesses, open a gate and let the dog into another small enclosure; the dog is retrieved from the other side of the second enclosure by a staff member, who uses the facility’s own slip lead on the dog. In this way, the people never come into contact with each other.
Dog-training classes have moved to Zoom and other live-streaming platforms for the time being; when classes can take place in person again, the trainers I know plan to reduce their class sizes by half in order to maintain safer distances between students. This is a tough one, because it also effectively cuts the trainer’s income in half – but trainers I know who teach indoors say it’s going to be necessary in order to keep students farther apart.
Placing a litter of puppies while maintaining social distancing
My friend fostered a litter of 10 puppies for my local shelter recently (I played a backup role). When it came time for the puppies to meet prospective adopters, the shelter made appointments with interested people. My friend and I transported the pups to the back side of the shelter and placed them in an outdoor exercise area; the shelter staff met the prospective adopters outside. It took more than two weeks to get the whole litter placed – a lot longer than just allowing people to come to the shelter and meet the whole litter, but it controlled the interactions in a safe way.
After the litter of pups had spay/neuter surgery, I kept the three girls at my house and my friend kept the boys at hers; it’s too hard for the girls’ incisions to heal nicely when they are wrestling with that many siblings. And as it turned out, given the slow pace of the adoption appointments, I had one girl for more than two weeks. She quickly got dubbed “Woody Junior,” since she looked just like his Mini-Me. Her color and markings were so similar to Woody’s. I had to keep telling people that Woody has been neutered since he was her age! He’s not the dad!

A very special reunion with my favorite foster puppy ever
As it turned out, a very special family saw photos of this puppy, the last to be available for adoption, on the WDJ Instagram page (rather than on the shelter website). I was contacted by the family who adopted Odin, the foster puppy from the litter of “mange puppies” I fostered a year ago. Remember Odin? He was the one who injured his eye, and eventually, had to have it removed; I had him with me for about six or seven months. I was SO happy that they contacted me directly to ask if she was available. We set up a meeting date, and they drove from a good distance to meet her – again, outdoors, safe distances, etc.
When they arrived, I got to see Odin again! I thought I would cry like a baby when I saw him – my favorite foster ever, I very nearly kept him – but he was actually too busy with greeting his buddy Woody to bother very much with me. Woody was happy to see Odin – they greeted each other with excitement – but then Woody’s attention was almost immediately drawn away from Odin by Odin’s boy, Adam, who picked up Woody’s ball and threw it. Woody is a fetch addict; once started, he’s hard to stop. And boys seem to LOVE that. Soon, the three boys (Odin, Woody and Adam) were off playing fetch together, complete with Odin occasionally stealing the ball and needing to be chased down to get it back.

The rest of the family was able to meet and greet the pup while the boys romped, and after a fairly short visit, they loaded her in their car and took her home. Again, no tears; I was so happy to see them all together. They’ve done such a nice job with Odin, I know they will take good care of Woody’s little Mini-Me.
Guide Dogs of America’s drive-through puppy pick up experience
Given the slow pace of these 10 puppy placements, I laughed and laughed when I heard that one of WDJ’s contributors, Stephanie Colman, distributed 13 – THIRTEEN! – puppies to their new homes in a single afternoon. Stephanie is the puppy program coordinator for Guide Dogs of America (GDA), based in Sylmar, California.
GDA breeds, raises, and trains guide dogs for people who are blind and visually impaired, as well as PTSD dogs for military veterans, children with autism, and facility dogs. The dogs are trained through its service dog branch, Tender Loving Canines Assistance Dogs, a prison training program where carefully chosen inmates are taught how to successfully raise a puppy and teach more than 30 service dog behaviors. GDA places about 60 guide dogs per year. It costs more than $48,000 to breed, raise, and train each dog, and dogs are matched to clients throughout the U.S. and Canada at no cost to the clients.

An important part of Stephanie’s job is to recruit and “train” families who want to be puppy raisers for GDA’s guide dog program. The families receive their pups when they are about 8 weeks old, and they keep them until the pups are about 15 to 18 months old. Scheduling all those families to pick up their pups from GDA’s Sylmar campus is also part of Stephanie’s job, and it was made a little more challenging this year, given the need to maintain safe social distancing. So Stephanie conceived a “drive through puppy pick up” experience, successfully scheduling 13 different families to come to the GDA campus, where they were handed their foster puppy through the car window by a masked and gloved puppy technician. Three different local television news stations covered the event! Here is a link to one station’s coverage.
I’ll have to remember this next time I am involved with placing a large litter!

If you live in Southern California and are interested in being a puppy raising family, GDA is hosting a free, online information session on Saturday, May 16. To learn more, visit www.guidedogsofamerica.org or call the puppy department at 818-833-6447.
How to Teach Your Dog to Wait
Old-fashioned training (the kind I grew up with) was mostly “don’t do stuff” – as in “Sit, Stay, Behave!” – where “Behave” meant “Don’t do anything.” As a force free trainer, I love that now we focus on training dogs to do rather than don’t-do. Today, for our dogs, “Behave” means “Do a behavior.” Ironic, then, that one of my most-used, and most useful cues, is “Wait!”
In my dogs’ world, “Stay” means “Stay in the exact position I left you in until I release you,” while “Wait” means “Pause for a bit.” I do still sometimes give a release with Wait, but it’s far less formal than a Stay.
I use Wait multiple times a day. It’s literally a life-saver. “Wait” when I open the car door so you don’t jump out into traffic. “Wait” at the door while I walk out – you’re not coming this time. “Wait” at the top of the stairs while I go first so you don’t trip me, causing me to fall. “Wait” while we’re hiking and you spot a deer or rabbit, so you pause and I can call you back to me and you don’t get lost chasing prey off into the woods.
Related: The 10 Most Important Things to Teach A Puppy
It’s easy to teach your dog to wait. Here’s how:
How to Teach Your Dog to Wait for the Food Bowl
- With your dog sitting, facing you, hold her bowl at chest level (with food in it, topped with tasty treats!) and say “Wait.”
- Lower the food bowl toward the floor two inches. If your dog stays sitting, click your clicker (or use a verbal marker) raise the bowl back up again, and feed her a treat from the bowl. If she gets up, say “Oops” and ask her to sit again. If she remains in place, lower the bowl two inches again, mark (click), raise the bowl, and treat.
- Repeat this step several times until she consistently remains sitting as you lower the bowl. Mark and treat each time.
- Gradually move the bowl closer to the floor with succeeding repetitions until you can place it on the floor two feet away from her and pick it back up without her getting up or trying to eat it.
- Finally, place the bowl on the floor and say a release cue like “Free!” to tell her to eat.
A really helpful thing about teaching this behavior is that you have at least one built-in daily training session (possibly two, since many of us feed our dogs twice a day).
How to Teach Your Dog to Wait at the Door
When your dog is solid with Wait at her bowl, you’re ready to generalize the behavior. The next easy place to practice Wait is at the door. Start with your dog sitting or standing – whichever you prefer. (I prefer Sit.)
- Say “Wait” in a cheerful tone of voice. Begin to open the door just slightly. If your dog starts to go out, say, “Oops!” and close the door (be sure she won’t get caught by the door!). Say “Wait” and try opening the door again. If she stays in place, close the door mark and release. Repeat several times.
- When your dog consistently doesn’t move for a tiny crack-in-the-door opening, gradually open it wider with each trial, a little bit at a time. Mark and treat each time, but sometimes repeat another Wait without releasing.
- Practice cueing your dog to Wait, and opening the door until you can open it completely and she stays in place. Once she’s able to Wait consistently with the door wide open, take one step out. Return, close the door, mark and release.
- Gradually increase the time the door is open while your dog is still waiting. Sometimes step out and return, sometimes walk out and invite her to come with you, sometimes walk out and close the door leaving her inside (this will be an auto-release cue).
- Practice Wait every time you head out, even if she’s going to come with you. Consistency is the key to helping your dog learn quickly!
How to Teach Your Dog to Wait on a Walk
To generalize further, practice with your dog on leash. As you’re walking, say, “Wait,” take a few more slow steps and stop. If your dog stops, mark and treat, and continue walking. If your dog continues moving after you stop, let her walk on. When she stops at the end of the leash, mark and treat, and walk on. She should quickly learn to stop when you say “Wait.”
Now, don’t wait – go train your dog!
Read Next: How to Train a Dog to Stay
Watching Your Dog Age Is Hard
Barbara Dobbins, my friend and frequent contributor to WDJ, once wrote a post for this space that described how her senior Border Collie, Daisy, had earned a “permanent hall pass” for jumping up on the counter to help herself to any food that had been left out. Two years into cancer treatment, Dobbins was happy that Daisy had an appetite! She also described other dogs she knew whose owners had decided to look the other way when the dogs did naughty things.
Otto is definitely showing some signs of aging
At 12 ½ years, my senior dog, Otto, has seemingly decided he should get a pass, too. My husband and I are not sure whether he’s getting a little senile, or simply emboldened by the plethora of as-yet uneducated foster puppies that have been trampling the landscaping and chewing drip-irrigation lines (or, alternatively, whining in a crate), or some combination of these things. Whatever the cause, the fact is that his behavior has begun to deteriorate just a bit.
Don’t get me wrong; he’s still a very, very good dog! But, adolescent misadventures aside, he’s always been near perfect – like the kid who sits in the front row and always – ALWAYS – has his hand up in class. If he hears me telling any other dog to “sit” or “down” or “come here,” he’ll pop up out of a dead sleep and run over to prove that he can perform those behaviors better and faster than the other dog can. So it’s a bit of a shock to have him completely blow me off when I call him after hearing him roar his terrible roar at the FedEx truck that’s passing by our house, and see him go tearing down the fence line, determined to chase the truck to the very edge of our property. How do I know he actually heard me and decided not to leave the chase? Because I could see him look over his shoulder and hesitate just a moment, and then decide, “Oh forget it, she’s too far away.”
Otto’s sudden interest in playing fetch
He’s also apparently decided that enough is enough when it comes to the relentless fetching of our younger dog, Woody – one of those dogs who would likely fetch until his feet turn bloody or until he passes out from heat exhaustion. If Otto is by himself, he will fetch a time or two, and then, chase the ball or other fetch item a third time, but just as he’s about to reach the fetch item, seemingly catch a whiff of some mystery aroma he just HAS to check out! “Excuse me, Mom, I think there was a raccoon on our lawn four nights ago, I should investigate.” In other words, he’s never been all that into fetching. But suddenly, he’s started to get very competitive when Woody is fetching.
He’s not nearly as fast or as coordinated as Woody, but he’s started to insert himself into any session of fetch, trying to beat Woody to any throw where that seems likely – which, because Woody never watches the ball, but just takes off running in the most likely direction, and Otto actually visually tracks the ball, Otto can get to more of the throws than he ought to be able to at his age. He also will try to intercept Woody on his way back to me with the ball and forcibly take the ball from him! Thank goodness, even though Woody is 4 ½ years old, he is still very submissive in the face of Otto’s “attacks.” He doesn’t quite give in, but he has not yet once tried to retaliate, either; he either tries to outmaneuver the older dog, or will stop and hunker down in a submissive pose, holding the ball tightly in his mouth and squinting his eyes tightly shut as Otto bites his face, trying to get the ball. “Sorry, man, I just can’t let go!”
Does Otto actually want to play fetch himself? Is he jealous of the attention that Woody gets for fetching? It seems that he just wants the ball; if he gets it, he just leaves with it! “Ha! That stupid game is over!” he seems to say. And, yes, I’ve tried having two balls on site when we are playing, so if Otto steals one, Woody and I can play on . . . Otto will drop whichever one we let him have and come in pursuit of the “active” ball in the game, so lately I’ve been putting him in the house when Woody needs a good, long session to work off some energy. I don’t want him to get hurt trying to overdo the fetching heroics!
It’s just weird, because he used to just watch Woody fetching like, “Yuck! What an idiot!” And now he’s like, “I have to STOP this!”

Other changes in Otto’s behavior
Also new: For most of his life, even if he didn’t want to do something, like, suffer through a bath in the yard with a hose, he would come when I called him. Slowly, sadly, but he would come (and he would get thanked, rewarded, and fussed over). Now, if he sees a hose and thinks a bath might be in the works, he just leaves, even if I’m calling him. “Nope! Just… nope!” He thinks – actually, he knows – I’m just not going to make him suffer through a hose bath anymore if he doesn’t want one.
But the biggest surprise came a few days ago, when my husband left his dinner unattended on the coffee table for a minute, and Otto just started helping himself to the food. WHAT?! He’s NEVER been a counter-surfer or helped himself to food like that before, which made both my husband and I wonder if this is a bit of dementia creeping in. He actually looked a bit surprised when both my husband and I, shocked at the same time, yelled “Hey!” I told my husband, we have to treat him more like a puppy again; we can’t take it for granted anymore that he knows all the house rules and will follow them. While I’m happy to issue him that “permanent hall pass,” and will likely just go ahead and let him have the rest of any burrito he manages to steal from now on, part of me is a little sad at these age-related behavior changes. Dogs just don’t live long enough! We’ll cherish all the time we have together, a little more now.
Puppy Potty Training: Simple, But Not Easy
The litter of 10 pups that my good friend was fostering for our local shelter at her home had a spay/neuter surgery date, and I was relieved. Surgeries had been cancelled for weeks, and while the pups could have been adopted out and brought back later for surgery, the shelter director instead decided to postpone the adoptions until a plan could be made to arrange surgery under covid-safe conditions. (Getting folks to bring 10 puppies back to the shelter on a given date is impossible, especially when they get adopted by families who may live several hours from here in every direction.)
Anyway, surgery was planned for a Thursday and my friend and I made a plan that the three girl pups would recover at my house, and she’d keep the boy pups corralled at hers. And the following Monday, we’d release the puppies’ portraits on the shelter’s Facebook page and the shelter would make appointments with people who were interested in adopting. We would bring the selected puppies to the shelter for outdoor “meet and greet” appointments and pick them up afterward if they didn’t get adopted.
It took about two weeks to get them all adopted, given the more arduous process of emails and phone calls and appointments, but they all did get adopted. One of the girls was the last to go, so all in all, I had three, then two, then one girl puppy here with me for about two weeks. And boy, oh boy, was it an in-depth refresher course in potty training.
A simple process
I tell people ALL THE TIME that potty training is simple, and it is. You take them outside CONSTANTLY, and you walk around with them and you watch them. And when they pee, you praise and give them a treat. Then you can bring them inside for about five minutes of scrutiny-free time and breakfast. But right after breakfast, you are all outside again, walking around, looking for that poop! And when that happens, you praise and give them a treat, and then you can bring them inside again, for maybe 10-15 minutes of scrutiny-free time, before you need to go out again for another pee.
You take them out after every nap. You take them out after every meal. You take them out after every play session ends. You take them out if it’s been more than 15 minutes since they last “went”! Simple! Not easy!
And what if they don’t “go”? Well, the smart thing to do is to pop them into a crate, because very few puppies will potty in a crate, so you can make sure that they don’t have a chance to “make a mistake” and pee or poop indoors, where you don’t want them to while you are not paying attention. Because no one can watch them every minute, even while sheltering in place! And if they potty in the house (or in your home office), they have just effectively been reinforced for doing so; it feels good to relieve the fullness of your bladder! And every mistake seems to build on itself; it’s far easier to just make darn sure a mistake doesn’t happen. In my experience, if you can get through three days of not letting them make even ONE mistake indoors, you’re pretty much home free with the potty training. They will want to go outdoors to potty and get right to business when you take them outside.
What not to do
What about the old “rub their nose in it” business? It’s poppycock. It makes them afraid of you, they don’t understand why you’ve grabbed them and have attacked them and are being gross. It’s a terrific way to induce a lifelong fear of humans, especially if there is poop or pee around, and to make them want to hide from you when they do go (so they become reluctant to go anywhere, even outdoors, near you; instead, you may find pee spots in closets and poop under your bed).
It can be effective, if you see a puppy start to squat, to run and grab the pup and carry them outside quickly – not in a way that scares the puppy, just interrupts her long enough so that she has some left to finish outside, where you can praise her. Being whisked outside isn’t all that comfortable, and it may be a little alarming – hopefully, just enough to interrupt her and not scare her, and what she remembers is the praise and maybe a treat for finishing outside. Simple! Not easy!
It’s not quite as easy as it sounds
I had three pups for six days, two pups for three more days, and one pup for seven more days; call it 31 total puppy days. My record? Not good. I ended the period with three pee puddles in my office, and probably six or seven in my house. (No poops indoors, however.) My mistake, EVERY time! Going over the 15-minute limit, when I should have either taken the pup/s outside or put them in a crate. I’d start making myself a sandwich for lunch, let the puppy come in, get interrupted by a phone call and ACK! see the pup squatting on the far side of the kitchen. Again and again! It’s so hard to pay such good attention for very long! And, though this seems backward, I had more success on the three-puppy and two-puppy days than I did on the one-puppy days. You can’t take your eyes off three pups or two pups; they are just capable of way more mayhem than one, not just potty stuff but also shoes, cords, paperwork, plants in the garden, rock-chewing, you name it. But one puppy chewing a chewy on her bed is easy to forget, until you hear a trickling sound. Argh! But a look at the clock says you’ve been working on the computer for an hour straight; she was overdue!
Anyway, when people complain about potty training, I don’t think I’m usually very sympathetic, because I feel like the whole process is So. Very. Simple! But I forgot that paying such close attention is just NOT easy!
To Neuter, or Not to Neuter Your Dog: That is the Question
There are any number of third-rail topics that occasionally electrify the conversationally unwary dog owner: Grains or grain-free? Dewclaw removal, cropped ears and tails, or leave well be? Raw or cooked? Flat collars or choke, pinch, or electronic?
But dog owners who came of age in the decades before spay/neuter practices became de riguer are sometimes shocked by the charge, increasingly popular, that sterilizing a dog is tantamount to condemning him or her to a shorter or more painful life. After all, if you are a respectable dog owner, nearly your entire adulthood may have been spent judging people with reproductively intact dogs – especially intact mixed-breed dogs – as supremely irresponsible. What gives? Why the reversal?
Veterinary practitioners have long dithered about what might be the “best” time in a dog’s life to undergo spay/neuter surgery, and some have theorized that coming to maturation without the benefit of secondary sexual hormones might possibly have deleterious effects on health. There have even been small studies looking for such. But there wasn’t any really impactful data that made the average dog owner question the wisdom of spay/neuter until a 2013 study (Torres et al) out of the University of California – Davis that found a link between neutering and the risk of certain cancers and joint disease in Golden Retrievers.
Since then, there has been a steady trickle of studies (with more on the immediate publication horizon) that examine some aspect or another of canine health and how it may be affected by spay/neuter – and the effect of this unending drip of evidence has been torture for many dog owners. We thought we were doing the right thing by sterilizing our dogs!
But is it really so bad to subject dogs to spay/neuter? Many of the studies that people cite to support their claims that the practice is unhealthy for dogs are based on statistically tiny samples, or dogs of a single breed. Extrapolating the results of highly limited studies to assert that spay/neuter is deleterious to all dogs is quite a reach.
To help you understand the modern claims that spay/neuter is bad for dogs, we’ve looked at dozens of studies examining some aspect of the possible health effects of gonadectomy – the removal of the dog’s gonads (sex organs, the testes in males and the ovaries in females). We’ll describe the evidence and discuss what it all means – but here is a little hint about our conclusions: You are still going to have to make your own choice about what’s “best” for you and your dog. And if your dog is already gonadectomized, that’s okay! The evidence is not so cut-and-dried as to support any across-the-board recommendations for all dogs.
The term “neuter” can be used for both male and female dogs, though it is more commonly used to refer to the process of castration (removal of testicles) in male dogs. Castration is specific to males, as spay is to females.
Spay/neuter refers generally to the removal of the gonads (the male’s testes and the female’s ovaries); that is more accurately called a gonadectomy – but it should be noted that while the female’s uterus and uterine horns are not gonads, they are also removed in spay surgery. Confusingly, “spay” sometimes is used to refer to a hysterectomy – removal of only the uterus and uterine horns. Removal of the ovaries (sparing the uterus and uterine horns) is referred to as ovariectomy.
“Sterilization” is another generic term that is frequently used, but it can refer to a process that induces infertility without gonadectomy.
“Desexing” is a term that has gained popularity in research literature. It’s defined as castration or spaying an animal, but the phrase evokes strong negative connotations for many people, who may fear it refers to somehow removing the biological sex of a dog; it doesn’t!
Since alternative methods of preventing reproduction are not common yet in the United States, almost all of the research looks at dogs that have undergone spay (removal of all reproductive organs) or castration; we will use the terms “spay/neuter” and “gonadectomy” interchangeably.
There are other common terms that refer to the age of gonadectomy. “Early age” or “prepubertal” spay/neuter indicates dogs who have undergone gonadectomy prior to six months of age. “Pediatric” spay/neuter surgery is usually defined as that which occurs between 6 and 16 weeks of age.
WHAT DO GONADS DO?
Before we look at the studies that examine the effects of gonadectomy, it’s helpful to understand what functions the gonads have in addition to reproduction.
Normal male and female dogs each have a pair of gonads.
The male gonads – the testes – reside in the scrotum and produce the male reproductive cells (spermatozoa, sperm for short) as well as androgen hormones that promote male characteristics.
Sperm cells are formed in the seminiferous tubules in the testes; in between these tubules are groups of endocrine cells, called interstitial cells, which produce androgens in response to luteinizing hormone (LH, sometimes referred to as interstitial cell stimulating hormone [ICSH]) secreted from the anterior pituitary gland located in the brain.
The principal androgen produced is testosterone, which is responsible for the development of the male reproductive system and secondary male sex characteristics, such as male body shape and sexual behavior. Testosterone is a steroid hormone that has an overall anabolic effect on the body, promoting protein synthesis and growth of tissues, encouraging the growth of muscle mass and strength, increasing bone density and strength, stimulating linear growth, and supporting bone maturation – all of which results in the larger size and weight of male dogs compared to females of the same breed.
Testosterone also stimulates development of the penis at puberty, the functioning of the prostate (a male accessory sex gland), and activation of sperm formation. Testosterone reaches the highest level in male dogs around 6 to 12 months of age and then it begins to plateau. As soon as a male dog is castrated, testosterone production ceases.
The ovaries are the female gonads, producing the ova (reproductive cells) and the female hormones estrogen (a compound term for the estrus-producing hormones estradiol, estriol, and estrone) and progestin.
Estrogens are produced by the cells of the ovarian follicles and are responsible for female secondary sex characteristic development, contributing to the maturation of the reproductive organs, control of the reproductive system, and for the behavioral and physical changes that occur in preparation for breeding.
Progestins, and in particular progesterone, are produced by the corpus luteum, a mass of cells that develops from the empty follicle after ovulation; they help prepare the uterus for implantation of the fertilized egg, maintain pregnancy, and promote the development of the mammary glands.
The adult male dog’s testes produce spermatozoa and hormones continuously; in contast, adult female canines produce reproductive cells in cycles, occurring about once every six months.
The estrous cycle is controlled by follicle stimulating hormone (FSH) and luteinizing hormone (LH) from the anterior pituitary gland. Coinciding with this short period of ovulation, estrogen levels rise, followed by a rise in progesterone levels. After ovulation, progesterone levels remain high for several weeks, even if the dog has not become pregnant. When a female dog is not in estrus, her estrogen and progesterone levels are low.
In addition to these reproduction-based tasks, the dog’s hormones function as chemical messengers with far-reaching and diverse tasks in the body – and likely include some that have yet to be identified. It should not be surprising, then, that researchers studying the effects of gonadectomy on dogs keep coming up with results that require further exploration.
Early in the 20th century United States, the majority of dogs never saw a veterinarian. Very few were subjected to a procedure that would prevent them from reproducing. (If they were, spays were often performed at 3 to 6 months of age and castration as early as four weeks!)
Many pet dogs were allowed to roam and reproduce willy nilly until the late 1960s and early 1970s, when the stray dog population grew large enough to pose problems in human society, including dog bites, the fear of rabies, and the cost of public animal control agencies needed to deal with dogs and dog-related hazards to human health.
By the early ’70s, animal control agencies were impounding millions of dogs every year, and they euthanized most of them. In a 1973 survey of shelters, the Humane Society of the United States (HSUS) estimated that a staggering 13.5 million dogs and cats were euthanized nationwide by shelters. That number of euthanized animals finally sparked enough outrage for society to begin trying to solve the problem.
It was recognized from the outset that efforts to prevent dogs from reproducing would be a critically important weapon in the war on pet overpopulation, with spay/neuter surgery being the most common method of sterilization for dogs.
Prior to this time, in the uncommon event that a veterinarian recommended the procedure to a dog owner, it was presented as a convenience – a way to reduce behaviors the many owners found problematic, such as straying – as well as a way to prevent unwanted puppies. Starting in the mid 1970s, however, dog owners were encouraged to take credit for promoting the well-being of the overall canine population when their dog’s potential for contributing to the homeless dog population had been eliminated.
Over the next four decades, the practice of routine spay/neuter surgery became the societal norm in this country. An estimated 85% of companion dogs in the U.S. have undergone elective gonadectomy. According to the American Veterinary Medical Association (AVMA), there are currently no state or federal laws requiring gonadectomy of all dogs in the U.S., and the AVMA “does not support regulations or legislation mandating spay/neuter of privately owned, non-shelter dogs and cats.” Some states have proposed mandatory gonadectomy laws, though none have been successful. There are, however, cities and other local governments that have proposed and adopted ordinances regarding spay/neuter laws. Many municipalities require higher licensing fees for intact dogs, sterilization for dogs deemed vicious or dangerous, as well as requiring gonadectomies for all shelter animals prior to release.
Where do things stand today? No statistics are available to prove the rate of spay/neuter compliance is declining, yet conversations among dog owners today demonstrate an increased awareness of the potential detrimental effects of the procedure. No mention of spay/neuter practices can be made online or in print without commentary from owners who have been convinced by whatever critical literature they’ve encountered (or their personal experiences) that spay/neuter is unmistakably and unambiguously harmful.
We’re not that sure.
Understanding history can guide our present day decisions. No one wants to return to a world where more than 13 million dogs are being put to death in shelters annually, and we know that not all dog owners are capable of preventing their intact dogs from reproducing. As history marches on, we look forward to studies that will enable researchers to make more targeted recommendations, so that any owner can find information that will prevent her from choosing a course of action that will hurt her dog more than it helps the overall dog population.
LOOKING AT THE SPAY/NEUTER LITERATURE
The following is an overview of the major areas of concern regarding the possible adverse health effects of canine spay/neuter and findings from relevant studies. The studies mentioned in the text below (and referenced completely on page 22) are some of the most frequently cited in discussions in veterinary literature.
Lifespan
Overall it appears that spay/neuter is associated with an increased life-span. However, be aware that most of the studies that concluded this looked only at gonadectomy (as opposed to other methods of sterilization) and usually did not take into account the age of spay/neuter.
Furthermore, the occurrence of having spay/neuter performed may contribute to an increased likelihood of better husbandry and veterinary care, which theoretically has a positive effect on life expectancy.
In the retrospective study by Hoffman et al (2013), the records of more than 40,000 sterilized and intact domestic dogs listed in the Veterinary Medical Database (a collection of data from veterinary teaching hospitals) were analyzed for associations between gonadectomy and lifespans and causes of death. It was found that sterilized dogs lived on average 1.5 years longer than intact dogs and life expectancy increased by 13.8 percent in males and 26.3 percent in females.
The study also found that intact dogs were more likely to die of infectious disease, trauma, vascular disease, and degenerative disease, and sterilized dogs were more likely to die of neoplasia (including an increased likelihood of transitional cell carcinoma, osteosarcoma, lymphoma, and mast cell cancers) and immune-mediated diseases. No causal relationship was found; note that gonadectomized dogs live longer and cancer is more prevalent in older dogs.
The dataset did not include at what age a dog was spayed or neutered, or whether a dog had reproduced prior to gonadectomy.
The Hoffman study findings were supported by Banfield’s State of Pet Health 2013 Report, which looked at data from Banfield facilities across the nation and included 2.2 million dogs.
Orthopedic Concerns
The literature review by Houlihan (2017) looks at the research on musculoskeletal diseases and possible associations with spay/neuter. Several studies have found gonadectomy to be a risk factor for development of cruciate ligament disease (CLD) and hip dysplasia (HD) in both male and female dogs.
HD has a high genetic component but is recognized as a multifactorial condition. Incidence of CLD tends to occur in young, active, large breed dogs from degenerative or traumatic causes, but it has also been correlated to aging, conformational abnormalities, and immune-mediated joint issues.
One focus for recent research is the assessment of the tibial plateau angle (TPA) – the slope at the top of the tibia. The steeper the TPA, the more stress on the ligament resulting in an increase in risk for CLD. Studies have demonstrated that the TPA is steeper in dogs that undergo gonadectomy before the closure of the tibial growth plates. The risk, however, may have a breed predisposition: Hart et al (2014) found that CLD risk increased in Golden Retrievers who were gonadectomized between the ages 6 and 11 months, but the risk for Labrador Retrievers did not increase when undergoing gonadectomy at the same age.
In a study of 759 client-owned Golden Retrievers, Torres et al (2013) looked at the effects of spay/neuter on joint disorders and cancer. The authors state, “An important point to make is that the results of this study, being breed-specific, with regard to the effects of early and late neutering, cannot be extrapolated to other breeds, or dogs in general.”
It is well documented that both testosterone and estrogen play an important role in the growth and maturation of bones. A decrease in bone density in spayed Beagles has been described in one study, but these results have yet to be reproduced in subsequent studies.
One heightened concern is whether gonadectomy affects the closure of growth plates (physes). Salmeri et al (1991) found that overall growth rates appear to be unaffected by spay/neuter, although prepubertal gonadectomy has been associated with delayed closure, resulting in lengthening of associated limb bones. While this can be statistically relevant, it is not readily visible or determined to be clinically relevant.
The age at which growth plates close is dependent on breed, genetic factors and disorders, physiological conditions, disease, and nutritional conditions (unbalanced or incomplete diets can result in growth abnormalities). Certain categories of breeds, such as working, herding, and sporting breeds, show greater susceptibility to orthopedic disorders in general; specifically dogs having large stature or great substance are at a greater risk for hip and elbow dysplasia (Oberbauer et al, 2019).
Spain et al (2004) found no specific correlation between age at spay/neuter and incidence rates of arthritis or long bone fractures, including physeal fractures. This retrospective study at the Erie County (New York) SPCA looked at 1,842 dogs who underwent spay or neuter surgery between 6 weeks and 12 months of age. Dogs who had the procedure before 5.5 months of age were found to have a higher incidence (6.7%) of hip dysplasia and were diagnosed at an earlier age when compared to dogs undergoing the procedure at the age of 5.5 months or older (4.7%).
However, those dogs who had spay/neuter surgery when they were older than 5.5 months were three times more likely to be euthanized due to hip dysplasia than those who had surgery when they were younger. This suggests that early gonadectomy may be associated with a less severe form of HD.
Estrogen has a number of metabolic functions and its effect on muscle, tendons, and ligaments has become the focus of more research. Chidi-Ogbolu and Baar (2019) found that, while estrogen improves muscle mass and strength and increases the collagen content of connective tissues, it decreases stiffness in tendons and ligaments, which can directly affect performance and injury rates. (Risk of cranial cruciate ligament [CCL]injury appears to increase with spay/neuter across the general dog population as well as in the individual breeds studied.)
Kustriz (2007) did not find any studies at that time that would implicate changes in physeal closure with subsequent asynchrony of long bone growth and abnormalities in joint formation as a cause of CCL rupture in dogs.
When you read any study (or read about any study) that presents information about the benefits or hazards of spay/neuter, it’s important to try to identify and keep the limitations of the study firmly in mind. Not all study conclusions will be relevant to all dogs.
Most of the research conducted on the health effects of spay/neuter is retrospective; researchers examine past and present medical records for a given population of dogs and look for patterns and trends in order to develop hypotheses. These retrospective studies can reveal only associations; some may be confounding while others are instructive and meaningful.
It’s challenging to evaluate the effects of spay/neuter and the resultant loss of hormones on canine health. The multifactorial nature of many diseases can interfere with definitive determination of causation. In humans, for example, areas of investigation related to cancer development include such factors as age, gender, ethnicity, diet, occupation, and environment, resulting in a complex composite of potential health impacts. Rarely are factors like these taken into account in veterinary studies, but research is beginning to expand to include these considerations.
When considering a study’s conclusions, don’t forget to evaluate overall incidence rates for diseases that are of concern. If an overall rate is rare or low, and the likelihood is shown by a study to increase with spay/neuter, the overall risk is going to remain rare or low. Kustritz (2007) categorized 11 different canine conditions based on their incidence rates of rare, low, moderate, or high. Those conditions considered high (mammary neoplasia, pyometra, benign prostatic hypertrophy), along with one in the moderate category (testicular tumors), all experienced a decrease in impact when gonadectomized. The conditions rated rare (transitional cell carcinoma), low (prostatic tumors, osteosarcoma, hemangiosarcoma, cruciate ligament disease, hypothyroidism), and moderate (urinary incontinence) have all been shown to increase with spay/neuter, but even with an increase, that risk continues to be small overall.
Biases can affect the value of a research study, even if it is unintentional. Recall bias can occur with studies that ask owners to provide information; the accuracy of owners’ reports about their dogs can be highly problematic. Selection bias occurs when the selection of a group for study does not achieve proper randomization. Many studies are affected by this bias because the datasets are often obtained from records at veterinary teaching/referral hospitals. This leaves out a percentage of dogs from the general population that don’t have their diseases brought to veterinary attention (which also skews incidence rates of diseases, as they are not reported). Furthermore, dogs who are treated at these hospitals are apt to be from upper- and middle-income owners and tend to have conditions that are treatable to some extent.
Finally, often studies only include one breed of dog, resulting in a breed bias; studies of this type cannot be extrapolated to all breeds, but they sometimes provide useful information.
Behavior
Behavior is the result of a complex interaction between genetics and environment. It has been noted that spay/neuter can mitigate some behaviors – and that’s about as far as the data can take you. The few effects that have been studied and found to be statistically relevant have generally been positive.
Studies generally report that spay/neuter reduces libido and decreases the associated reproductive behaviors. Spayed females tend not to engage in any of the behaviors associated with estrus and therefore do not seek out breeding opportunities.
Neutered males tend to show a decrease in roaming, intermale aggression, mounting, and urine-marking behaviors. There is consistent evidence that the frequency of urine marking does not depend on the age at gonadectomy.
Kustritz (2007) reported that neither reproductive status nor age at the time of spay/neuter has been found to affect the trainability of working dogs.
According to Duffy and Serpell (2006), behavioral changes are difficult to measure; the parameters with which they are measured are too subjective. Breed, sex, and individual differences need to be considered when examining the manifestation of behavioral changes following spay/neuter. As a result, there is not a clear consensus on what the real effects are.
Furthermore, “interpretation of the literature related to behavioral changes is further complicated by various definitions of aggression” (Houlihan, 2017); as a result, evidence for the influence of gonadectomy on aggressive behavior is inconsistent and sometimes contradictory.
Kustritz (2007) reported that several studies showed an increase among female dogs of heightened reactivity toward humans following spay. It is hypothesized that this may be due to a decrease in estrogen and oxytocin levels. Additionally, testosterone has been shown to increase confidence; this may be useful for timid dogs, but may not be for overconfident ones.
Reproductive System
Spay surgery has been shown to have a beneficial effect on life-limiting diseases in female dogs. It not only eliminates the risk of pyometra and uterine and ovarian cancers, but also reduces the risk of mammary cancer.
Research into the influence of spaying on mammary cancer has been extensive. Dorn et al (1968) found that there is strong evidence that ovarian hormones are essential for the development of most cases of mammary cancer, so removal of the ovaries decreases this risk. Subsequent studies have continued to support the protective effect of early spay.
The greatest benefit occurs if spay takes place before the first estrus; the reported rates are .05% if before estrus, 8% if performed after the first estrus, increasing to 26% after second estrus cycle (Schneider et al, 1969). Mammary cancer rates increase greatly with age in dogs. Purebred dogs have been shown to have two times the rate of mammary cancer when compared to mixed-breed dogs of the same age. The incidence rate of mammary neoplasia is estimated to be about 3.4%, with about 50% being benign fibroadenomas and 50% malignant adenocarcinomas.
Castration eradicates the risk of testicular cancer (as the testes are removed) in males. Castration also reduces the risk of age-related prostate issues, benign prostatic hyperplasia (common but not generally life-limiting), and perianal adenomas.
Several studies that show testicular neoplasia is common in older (mean age of 10 years) intact male dogs; however, metastasis is uncommon and castration at time of diagnosis is curative. Benign prostatic hypertrophy is also common in intact male dogs (63.4% in one study). It tends to manifest in 50% of dogs aged 2-3 years, and in 75-80% by age 6. Castration results in a decrease in prostate size resulting in a reduction of clinical signs (Kustritz, 2007).
Cancer
The literature review by Urfer and Kaeberlein (2019) reports that there are many studies that provide evidence for an increase in risk for cancer in dogs of both sexes that have undergone gonadectomy. Smith (2014) summarized that male dogs were at an increased risk after castration for developing cardiac tumors, osteosarcoma, prostatic tumors, transitional cell carcinoma, and lymphoma, while the risk decreased for testicular cancer.
In female dogs, there was an increased risk post-spay of cardiac tumors, cardiac and splenic hemangiosarcoma, osteosarcoma, mast cell tumors, and lymphoma, while the risk decreased for ovarian, uterine, and mammary cancers.
Many of the studies did not take age into account – which is arguably the most important factor for tumor development. However, when the studies did take age into account, increased age was found to be a higher risk factor than spay/neuter.
It’s been said that cancer is, ultimately, the result of failed immune surveillance. It is suspected, but not yet proven, that cancer-hunting immune cells depend to some extent on signals from the sex hormones to perform this surveillance. Researchers have speculated that the cancer-hunting immune cells may be less effective at this task in gonadectomized dogs due to the lack of hormonal signalling.
In the breed-specific retrospective study by Kent et al (2018), the timing of spay/neuter was not available for most of the Golden Retrievers. While the study assessed cancer as a cause of death, the association of hormonal exposure on lifespan or the risk of death by cancer couldn’t be evaluated, nor was it part of the evaluation for the risk of cancer development. Given that Golden Retrievers are known to be at a high risk for cancer, these results cannot be extrapolated to other breeds.
The study by Cooley et al (2002) found that Rottweilers of both sexes who had undergone early spay/neuter had higher risks for bone sarcoma (1 in 4) when compared to Rottweilers who were intact throughout their lifetime. However, the study acknowledges that it is not known how hormones affect the development of osteosarcoma. Makielski et al (2019) published a comparative review of osteosarcoma risk factors in dogs and humans and included this commentary on trending current hormonal studies:
“… associations between reproductive status and development of osteosarcoma have been inconsistent. Although several reports suggest that spayed and/or neutered dogs have higher incidence of certain cancers, including osteosarcoma, the relationship between reproductive status and cancer risk may be confounded by other variables, such as the documented tendency toward increased adiposity and body condition in gonadectomized dogs.”
Obesity
In dogs, obesity is influenced by diet, breed, activity level, and age, but spay/neuter has also been reported to be a common predisposing risk factor for increased body weight. There is conflicting information as to whether gonadectomy alters metabolism (Reichler, 2009). It is speculated that gonadectomized dogs in general have lower metabolic rates (it has been estimated that they may require as much as 30% fewer calories) and tend to gain weight more than intact dogs, however, the cause and effect relationship is not well defined.

Spain et al (2004) conducted a population study that indicated that gonadectomy of dogs before 6 months of age is associated with a lower prevalence of obesity when compared to those undergoing gonadectomy after 6 months of age.
In 2019, Bjørnvad et al published a study of dog- and owner-related risk factors for obesity in Danish companion dogs. The research found castrated male dogs were at increased risk for obesity; it is suspected that this may be due to a reduction in testosterone and a subsequent lowering of basal metabolic rate. Female dogs were found to be at risk regardless of reproductive status. They also found that there was a complex association between the owner’s weight, the dog’s weight, and feeding habits.
Urinary System
Studies place the incidence of urinary incontinence in spayed female dogs at 4% to 20%, compared to a rate of 0.4% to 8% for intact females. Spayed dogs may develop incontinence within days of surgery or more commonly years later; it is typically controlled with treatment. Large and giant breeds appear to have a higher risk. Other factors that may contribute to the condition and need further evaluation are urethral length, resting position of the urinary bladder, breed, thyroid level, allergies, and level of obesity.
Studies are contradictory when it comes to determining a correlation between age at time of spay and the likelihood of developing incontinence. Spain et al (2004) and Thrusfield et al (1998) reported an increase in urinary incontinence in females who were spayed at an early age, yet other studies have failed to support this conclusion. More research is required, but in those studies that did find a correlation, it was associated only with pediatric (6-12 weeks) gonadectomy. Females spayed at an early age have also been reported to have had a slightly higher incidence of bladder infections, but these infections were easily treated and did not become chronic.
It has been theorized that it is the lack of estrogen that causes incontinence in spayed females, but this is controversial and not fully supported by research. Increased rates of incontinence are not reported in pregnant females even though they have extremely low estrogen levels during pregnancy.
Palm and Reichler (2012) report that incontinence in spayed dogs has been successfully treated with use of gonadotropin-releasing hormone (GNRH) superagonist implants. The implants work by suppressing the release of gonadotropins.
In contrast, surgical gonadectomy increases the release of gonadotropins. This suggests that an increased risk for incontinence is not caused by the lack of sex hormones, but rather by the increased levels of gonadotropins induced by removal of the ovaries.
Male dogs who have been castrated prepubertally tend to have a smaller penis and prepuce, but their urethral diameter and function are the same as dogs neutered later and no clinical significance or condition has been associated with this difference (Salmeri et al, 1991).
Immune System
Findings from Sundberg et al (2016) suggest that spay/neuter is associated with an increased risk for certain autoimmune disorders. Six of the 11 immune diseases evaluated (atopic dermatitis, autoimmune hemolytic anemia, Addison’s disease, hypothyroidism, immune-mediated thrombocytopenia, and inflammatory bowel disease) showed an increased prevalence in gonadectomized dogs.
The study notes that even though the dataset included more than 90,000 dogs and expression of the diseases were statistically relevant, the actual incidence rate was not high and it declined over the 15-year evaluation.
Given that this was a retrospective study limited to dogs seen at a referral veterinary hospital, it may not reflect incidence rates within the population at large but rather may be biased to complex or more severe cases.
Cognitive Function
There has been limited research conducted on the risk that cognitive function may be altered as a result of spay/neuter. A comparison of the progression of cognitive dysfunction in intact and castrated male dogs was performed in the Hart study (2001) with a small sample size (6 dogs); it revealed a slowing of progression in the intact dogs.
In contrast, a 2000 study by Waters et al found that intact Beagles showed DNA damage to the neurons in the brain when compared to castrated Beagles (again, sample size was small, with only four dogs in each group). This is an area of research that is just beginning to be explored. Much more research is needed to understand the processes that influence cognitive function and how they may be changed by spay/neuter.
Anesthesia
Statistically, puppies are less likely to die under anesthesia and recover faster from gonadectomy than their adult counterparts. Complications arising from the procedure are uncommon and the rates are consistent across ages.

In 2018, my five-month-old, intact Border Collie began to display an abnormal outward turn to his left front leg. Parker’s orthopedic surgeon diagnosed him with an early closure of the ulnar growth plate, probably as a result of inury. The ulna ceased growing while the radius continued to lengthen. The radius began to bow as it was restricted by the nongrowing ulna, resulting in the outward splay of the leg. Ultimately, his leg was repaired within a few degrees of normal through a series of surgeries as he grew.
Knowing that my young pup faced multiple surgeries, I did not want to have to put him through an additional anesthetic for neuter surgery within the next year and opted to have his gonadectomy done during one of his orthopedic procedures.

Some friends questioned my decision when they heard that I was going to have my young dog neutered, citing unnamed “studies” alleging that early spay/neuter can have a disastrous effect on the bones and growth plates. I researched all the studies I could find – and concluded that they were limited in scope. But I also consulted with his orthopedic surgeon (one who treats a great number of canine athletes). He related that he had not seen any negative effect of early spay/neuter in the animals he treated. I was aware that this was anecdotal evidence, but if the person working on the bones of agility dogs wasn’t seeing anything he could relate to early spay/neuter, that was good enough for me.
Two years later my boy is happy, healthy, and active with no residual orthopedic concerns. His appearance is similar to his dad (intact), mom (recently spayed), and sister (intact) from another litter, but not so much like one of his intact male littermates. Is this a result of the lack of testosterone? Or due to his own individual genetic structure and environment? Did neutering him “early” (at 6 months of age) predispose him to cancer and other health concerns? While I may wonder about these issues, I am confident that I made the best decision I could for me and my dog at that time.



WHAT (AND HOW) SHOULD YOU DECIDE?
Even a minimal survey of the research regarding the effects of spay/neuter reveals that the situation is extremely complex and, at times, ambiguous. There is evidence to support correlations for both beneficial and adverse effects, but even more important is that it demonstrates how much we still don’t understand about reproductive hormones and the consequences of spay/neuter.
When the time comes for you to make spay/neuter decisions for a dog that you do not want to reproduce, remember: There is no single course of action that is “best” for all dogs and all owners, and don’t let anyone make you feel bad for your decision, whatever it is – that is, as long as it doesn’t end with an accidental breeding and unwanted puppies.
Here’s the one time that we feel it makes the most sense for an owner to give more weight to published research than their own preferences: when the person owns a purebred dog of a breed that has been the subject of large, well-respected studies of the effects of spay/neuter on dogs of that specific breed, and the study found clear and significant statistical advantages to a certain course of action. In that case, we would strongly recommend reading the conclusion of those studies and discussing them with your veterinarian. Oberbauer et al (2019) determined that many canine health disorders reflect the dogs’ genetic heritage. Within breeds, there may be shared genetic susceptibility that increases risk for certain diseases within breeds and this risk may be enhanced with neutering.
However, you have to take single-breed studies with a grain of salt if your dog does not share any of the subject breed’s genes. Some of these studies are widely cited by people who think the studies should inform the decisions of all dog owners, but the findings often are contradicted when applied to another breed.
Some people strongly believe that it’s unethical to spay or neuter dogs, because the procedure irretrieveably alters the dog’s physiology and might might cause an adverse side effect, perhaps years in the future. As we have described, however, intact dogs are also prone to adverse health conditions; there simply isn’t a choice that doesn’t have consequences!
OWN YOUR DECISION – AND RESPECT OTHERS
As we’ve stated elsewhere in this article, it has become sort of politically correct today to maintain a dog in his or her intact state. But this isn’t something that everyone can manage in a responsible fashion! If there is a single weak link in a household, whether it’s a forgetful child, a distracted adult, or a less-than-super-secure fence, accidents can and will happen.
We know owners who swear their female dogs never left their sides and had zero contact with another dog, and yet – poof, a virgin pregnancy? Doubtful, and irresponsible, too.
And while some people will try to make you feel bad about it, it’s okay to admit that you do not enjoy living with an intact dog of either sex! If you have grown up in a time and place where literally all the dogs you’ve ever known were neutered, you might be quite alarmed at the personality change exhibited by your female dog when she comes into heat. You may not feel comfortable with some of the more strongly masculine attributes of an intact male dog, which may include more competitive urine-marking, humping, or overzealous sexual interest in female dogs.
Also, there are many people who are strongly committed to adopting only from shelters or rescue organizations, where spay/neuter is not only mandated but might also have been performed on very young puppies. Not only is prepubertal gonadectomy an important tool against pet overpopulation, it is likely to improve the odds that dogs will be retained by their owners. Studies have found that intact dogs are more likely to be relinquished than those that have undergone spay or neuter.
For intact dogs with homes, veterinarians and owners are challenged with making the best decision for that specific dog. An informed decision requires an evaluation reflective of our dogs and our risk tolerances. Every dog is an individual, including how they respond to gonadectomy or remaining intact. We always recommend consulting with your veterinarian to determine the best strategy for your dog based on age, body condition, breed, genetics, lifestyle, behavior, temperament, and reproduction management – and then taking responsibility for your choice.
If you’ve gotten this far, we applaud you! It’s a lot of information! But if you want to delve even more deeply into the research on the possible health effects of spay/neuter, this list is a great resource. It’s impossible to mention every study on the subject, but this list includes all the studies referenced in the foregoing article as well as other frequently cited works.
Banfield Applied Research and Knowledge Team. “Banfield Pet Hospital State of Pet Health 2013 Report, Trends of Life Spans for Dogs and Cats.” banfield.com.
Bentley A, Thalheim L. “Controversies in spaying and neutering: Effects on cancer and other conditions.” Cornell University Veterinary Specialists, Stamford, CT.
Bjørnvad CR, Gloor S, Johansen SS, et al. “Neutering increases the risk of obesity in male dogs but not in bitches: A cross-sectional study of dog- and owner-related risk factors for obesity in Danish companion dogs.” Prev Vet Med 2019; 170:104730.
Chidi-Ogbolu N, Baar K. “Effect of estrogen on musculoskeletal performance and injury risk.” Front Physiol 2019; Jan 15; 9:1834.
Cooley DM, Beranek BC, Schlittler DL, et al. “Endogenous gonadal hormone exposure and bone sarcoma risk.” Cancer Epidemiol Biomarkers Prev 2002; 11: 1434–1440.
Dorn CR, Taylor D, Schneider R, et al. “Survey of animal neoplasms in Alameda and Contra Costa Counties, California.” J Natl Cancer Inst 1968; 40:307-318.
Duffy DL, Serpell JA, Hsu Y. “Breed differences in canine aggression.” Appl Anim Behav Sci 2008; 114:441–460.
Duffy DL, Serpell JA. “Non-reproductive effects of spaying and neutering on behavior in dogs. Presentation from proceedings of the 3rd International Symposium on Non-Surgical Contraceptive Methods for Pet Population Control, 2006.” Alliance for Contraception in Cats & Dogs. naiaonline.org/uploads/WhitePapers/EarlySNAndBehaviorDuffySerpell.pdf.
Duval JM, Budsberg SC, Flo GL. “Breed, sex, and body weight as risk factors for rupture of the cranial cruciate ligament in young dogs.” J Am Vet Med Assoc 1999; 215: 811–814.
Farhoody P, Mallawaarachchi I, Tarwater PM, et al. “Aggression toward familiar people, strangers, and conspecifics in gonadectomized and intact dogs.” Frontiers in Veterinary Science 2018; 5:18.
Grumbach M. “Estrogen, bone growth and sex: a sea of change in conventional wisdom.” J Ped Endocrinol Metab 2000; 13: 1439–1455.
Hart BL, Eckstein RA. “The role of gonadal hormones in the occurrence of objectionable behaviors in dogs and cats.” Appl Anim Behav Sci 1997; 52: 331–344.
Hart BL, Hart LA, Thigpen AP, et al. “Neutering of German Shepherd Dogs: Associated joint disorders, cancers and urinary incontinence.” Vet Med Sci 2016; 2: 191–199.
Hart BL, Hart LA, Thigpen AP, Willits NH. “Long-term health effects of neutering dogs: comparison of Labrador Retrievers with Golden Retrievers.” PLoS ONE 2014; 9: e102241.
Hoffman JM, Creevy KE, Promislow DE. “Reproductive capability is associated with lifespan and cause of death in companion dogs.” PLoS ONE 2013; 8: e61082.
Houlihan KE. “A literature review on the welfare implications of gonadectomy of dogs.” J Am Vet Med Assoc 2017; 250(10):1155–1166.
Howe LM, Slater MR, Boothe HW, et al. “Long-term outcome of gonadectomy performed at an early age or traditional age in dogs.” J Am Vet Med Assoc 2001; 218: 217–221.
Howe LM. “Current perspectives on the optimal age to spay/castrate dogs and cats.” Vet Med (Auckl). 2015 May 8;6:171-180.
Howe LM. “Prepubertal gonadectomy in dogs and cats, part I.” Compend Contin Educ Pract Vet 1999; 21: 103–110.
Howe LM. Rebuttal to “Early Spay Neuter Considerations for the Canine Athlete,” 2007. semanticscholar.org/paper/Rebuttal-to-“-Early- spay/neuter-Considerations-for-Howe/f9c144ef90d398772af99856d6ec2518ae1a47a8Semantic Scholar.
Kent M, Burton J, Rebhun R. “Association of cancer-related mortality, age and gonadectomy in Golden Retriever dogs at a veterinary academic center.” (1989-2016). PLoS One 2018; 13(2): e0192578.
Kustritz MV. “Determining the optimal age for gonadectomy of dogs and cats.” J Am Vet Med Assoc 2007; 231: 1665–1675.
Kustritz MV. “Pros, cons, and techniques of pediatric neutering.” Vet Clin North Am Small Anim Pract 2014; 44: 221–223.
Makielski, K., Mill, L., Sarver, A., et al. “Risk factors for development of canine and human osteosarcoma: A comparative review.” Vet. Sci 2019, 6(2), 48.
Oberbauer A, Keller G, Fanukla T. “Long-term genetic selection reduced prevalence of hip and elbow dysplasia in 60 dog breeds.” PLoS ONE 2017 12:e0172918.
Oberbauer, AM, Belanger, JM, & Famula, TR. “A review of the impact of neuter status on expression of inherited conditions in dogs.” Frontiers in Veterinary Science 2019; 6:397
Palm J, Reichler IM. “The use of deslorelin acetate (Suprelorin®) in companion animal medicine.” Schweiz Arch Tierheilkde 2012, 154, 7-12.
Reichler IM, Hubler M, Jöchle W, et al. “The effect of GnRH analogs on urinary incontinence after ablation of the ovaries in dogs.” Theriogenology 2003; 60(7):1207–1216.
Reichler IM. “Gonadectomy in cats and dogs: a review of risks and benefits.” Reprod Domest Anim 2009; 44: 29–35.
Salmeri KR, Bloomberg MS, Scruggs SL, et al. “Gonadectomy in immature dogs: effects on skeletal, physical, and behavioral development.” J Am Vet Med Assoc 1991; 198: 1193–1203.
Salmeri KR, Olson PN, Bloomberg MS. “Elective gonadectomy in dogs: A review.” J Am Vet Med Assoc 1991; 198: 1183-1192.
Schneider R, Dorn CR, Taylor DO. “Factors influencing canine mammary cancer development and postsurgical survival.” J Natl Cancer Inst 1969; 43: 1249–1261.
Serpell J, Hsu Y. “Effects of breed, sex, and neuter status on trainability in dogs.” Anthrozoos: A Multidisciplinary Journal of The Interactions of People & Animals 2005; 18: 196-207.
Smith AN. “The role of neutering in cancer development.” Vet Clin North Am Small Anim Pract 2014; 44: 965–975.
Spain CV, Scarlett JM, Houpt KA. “Long-term risks and benefits of early-age gonadectomy in dogs.” J Am Vet Med Assoc 2004; 244: 380–387.
Sundburg CR, Belanger JM, Bannasch DL, et al. “Gonadectomy effects on the risk of immune disorders in the dog: A retrospective study.” BMC Vet Res 2016; 12: 278.
Torres de la Riva G, Hart BL, Farver TB, et al. “Neutering dogs: Effects on joint disorders and cancers in Golden Retrievers.” PLoS ONE 2013; 8: e55937.
Urfer SR, Kaeberlein, M. “Desexing Dogs: A Review of the Current Literature.” Animals 2019; 9(12):1086.
Von Pfeil DJ, DeCamp CE, Abood SK. “The epiphyseal plate: Nutritional and hormonal influences; hereditary and other disorders.” Compend Contin Educ Vet 2009; 31(8):E1–E14.
Waters DJ, Kengeri SS, Clever B, et al. “Exploring mechanisms of sex differences in longevity: Lifetime ovary exposure and exceptional longevity in dogs.” Aging Cell 2009; 8: 752–755.
Waters DJ, Shen S, Glickman LT. “Life expectancy, antagonistic pleiotropy, and the testis of dogs and men.” Prostate 2000; 43: 272–277
Zink MC, Farhoody P, Elser SE, et al. “Evaluation of the risk and age of onset of cancer and behavioral disorders in gonadectomized Vizslas.” J Am Vet Med Assoc 2014; 244: 309–319.
Barbara Dobbins, a former dog trainer, writes about dogs and studies canine ethology. She lives in the San Francisco Bay area with her dogs, Tico and Parker.
Protocol for Teaching a Safe “Trade” With Your Dog
Start with your dog on a leash and either stand on the end of the leash or tether him to something solid so he can’t leave with the item at any point in the “game.”
1. Say “Take it!” and give the dog a low-value object – something he will easily and willingly give up in exchange for a high-value treat.
2. Offer him your high-value treats – close enough that he can sniff then, but don’t try to push them into his mouth. (Anything that resembles coercion will likely increase his resistance.) Have a large enough supply of high-value treats that it will take him a little while to eat them all. Do not use a cue yet.
3. If he drops the low-value item (in order to explore or take the higher-value treats you offered), click your clicker (or use a mouth click or verbal marker) and, while you keep him occupied nibbling at the high-value treats in one hand, pick up the low-value object with your other hand and hide it behind your back. You must use two hands for this! If you let him eat the high-value treats and then race him back to the object, you’re likely to lose the race and you might elicit resource-guarding.

As soon as he finishes eating the treats in your hand, bring out the object from behind your back, say “Take it!” and give it back to him. This teaches him that he doesn’t lose the object – that he can trade with you and then get it right back. This will make him more willing to trade with you again in the future. It’s a win/win for him!
If he doesn’t show any interest in taking the low-value object after you’ve traded it for high-value treats, you may need to start by giving him a slightly higher-value object and/or using lower-value trade-treats.
If he doesn’t drop the item, make a short “Hansel and Gretel” trail of treats under his nose and then trailing a foot or so off to the side. Engage his mouth with the treats in your hand after he follows the trail, while you pick up the item with your other hand.
If he still doesn’t drop the item, you need to start by
giving him an even lower-value item and/or using far higher-value treats in your hand. (Think meat, not dry cookies.)
4. When you can predict that he will always drop the item when you offer your treats, you’re ready for the next step. First, give your cue (“Trade!”), pause for a few seconds, and then do what you’ve been doing: offer the treats, click when he drops the item, and pick up the item with your free hand while you keep his mouth busy nibbling treats from your hand.
5. After several repetitions, sometimes pause a few seconds longer before offering your treats. Your goal is to get him to drop the object when you say “Trade!” – before you offer the treats. When he will do this reliably, it means you have the behavior “on cue” – he drops the object because he heard and understood the cue, not just because you stuck high-value treats under his nose.
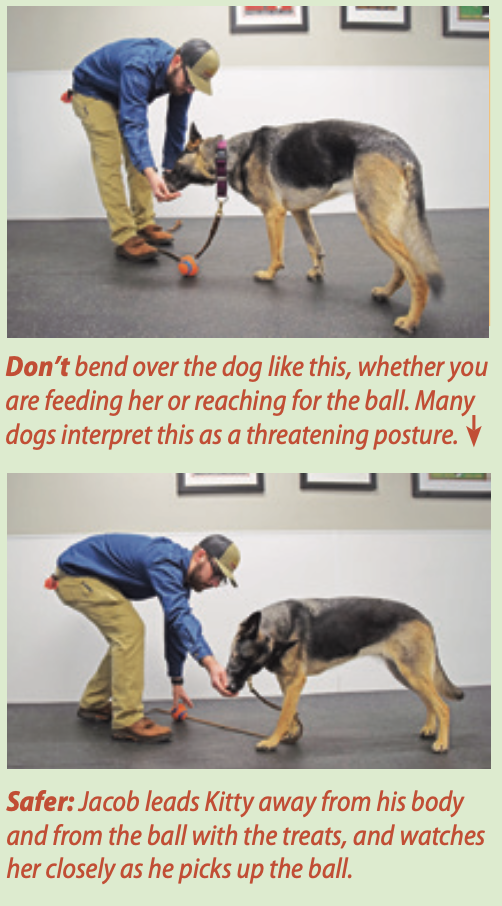
Thanks to Jacob Paxson of The Canine Connection in Chico, California, who demonstrated the do’s and don’ts of the “Trade” protocol.
The “I Come In Peace” Guarding-Modification Protocol

This article is a sidebar/companion piece to “Changing of the Guarder: Resource Guarding in Dogs.”
This guarding-modification protocol, created by my friend and fellow trainer Kelly Fahey, owner of The DogSmith of Hunterdon in Pittstown, New Jersey, is a simple protocol that can be used by shelters, people who have adopted dogs who showed guarding behavior in the shelter or whose dogs started guarding in their new home, and by any dog owner with a guardy dog. When done properly, it teaches the dog that a person approaching means more good stuff is coming, helping to dispel the dog’s notion that the person might take her good stuff away.
The procedures should be undertaken by one person at first, then generalized to others.
As always, when modifying behavior, we want to remove as many opportunities for the dog to practice the unwanted behavior as possible. If a dog in a shelter is being “guardy” as visitors pass by, she is at risk of being triggered by every passerby, and her behavior will worsen. If possible, such a dog would benefit from being moved to a kennel in a ward without public access and brought out to be shown to potential adopters who seem like a good match.
Note: If at any time you elicit a growl or other guarding behavior, you are too close and/or have proceeded too quickly.
1. Tether the dog to an eye bolt affixed to the wall for that purpose, or to a solid, heavy object. Give her a valuable chew object (not a Kong – it will roll out of her reach) or a small bowl of food.
2. Have a good supply of high-value treats that you can toss easily. (Chicken does not work well for this – it’s too messy and hard to accurately toss.) Small bits of cheese or meat work well.
3. Walk past the dog at a safe distance. Depending on the dog, this may be six to eight feet beyond the end of the tether, or it may be closer. As you pass, toss several high-value treats near the bowl or chewy, where she can easily reach them. Keep walking; do not pause to toss. If the dog growls, lunges, or shows other obvious guarding behavior, you are too close.
4. Repeat Step 3 until, as you approach, you see the dog starting to look up in happy anticipation of the treats she expects you to toss. When she does this consistently, decrease the distance between yourself and the dog by a few inches as you pass by.
5. As long as she is consistently happy at each new distance, continue passing by and dropping treats, gradually getting closer to her when you pass.
6. When she is happy with you walking past at a distance close enough to touch her, pause as you pass and feed a treat from your hand. Then walk on.
7. When she stays happy with your pause-and-feed, gradually increase the length of time that you pause and feed her treats. The increase should be no more than 1 to 2 seconds. As you increase the length of your pause, start talking in a happy voice as you feed her the treats.
8. When you can pause for about 10 seconds and she stays happy, occasionally bend slightly and drop a treat into the bowl or next to her chewy, then feed some more from your hand and walk on.
9. Repeat, gradually increasing the number of times you bend and drop.
10. Now, gradually increase how much you bend over until you can touch the bowl or chewy. Remember, if you see any sign of tension you have moved too quickly. Back up a few steps and continue more slowly from there.
11. Finally, as you are pausing, bending, and feeding, occasionally play the Trade game, always returning the bowl or object to her after she has happily allowed you to take it.
12. Now, start the protocol over again at Step 1 with another staff member, volunteer, or reliable family member. Continue until the dog is comfortable with a variety of people approaching her. Repeat the process with any new family friends or shelter visitors that can follow your directions, always starting with Step 1.
Resource Guarding in Dogs: What You Need To Know

Resource-guarding in dogs – that is, protecting valuable possessions – is a natural, normal behavior. Yet at some point we humans developed the arrogant and misguided belief that we should have the right to take anything away from our dogs, any time we darn well please, and our dogs should have no right to object. Dogs who attempt to protect their valuable resources in their humans’ home tend to be punished, sometimes severely.
Until very recently, shelter dogs who exhibit resource guarding were almost always met with a more permanent outcome: euthanasia.
Should dogs really be met with cruelty or death because they’d prefer not to share their food, toys, or bed?
I’m a passionate advocate for families who want to adopt from a shelter and want a dog who won’t hurt other members of their family. But I also believe that many dogs who exhibit resource-guarding in the highly stressful environment of a shelter can be safely incorporated into many family homes.
ASSESSING RESOURCE GUARDING IN A SHELTER
Most shelters use some sort of behavior assessment, formal and structured or informal and ad hoc, to determine which unclaimed or relinquished dogs should advance to the shelter’s adoption program or be designated for behavior modification, and which should be deemed “unadoptable.” In recent years, the behavior assessments that are most widely employed by shelters have come under fire due to studies that suggest that they are not predictive and not replicable.
“Not predictive” refers to the studies’ findings that behaviors presented by dogs during a shelter assessment are very often never seen in the adoptive home – and, conversely, behaviors not seen in the shelter assessment often do occur after dogs are placed in homes.
“Not replicable” means that results of one shelter staff person’s assessment of a dog may be entirely different if the same dog is assessed by a different person, or on a different day. Both of these flaws put the validity of the assessment tools into question.
In our view, given that aggression is caused by stress, and even the best shelter in the world is a stressful place for almost any dog, it’s not surprising that a stressed shelter dog might be more likely to snap and snarl when pressured in the presence of a high-value resource – or in response to some of the other provocative procedures in an assessment.
The findings of recent studies about assessments put responsible shelters in a difficult position. How do they best ensure they are not putting dangerous dogs into the hands of the public if they cannot trust the results of their assessment protocols? There are no easy answers – but there are things that shelters can do to keep from killing dogs who are unlikely to cause harm after being adopted into a family environment:
- Realize that resource-guarding is, indeed, a natural and normal canine behavior, especially for a dog who is living in a stressful environment.
- Be more forgiving when a dog exhibits some tension over a valuable resource during the assessment process. Rather than an immediate “You failed!” response when a dog tenses or growls, gently pursue the process (assuming a fake hand is being used). During my long career working with shelters and doing assessments, I have seen a significant number of dogs de-escalate their level of tension when the assessor remained calm and continued the process with gentle persistence.
- Recognize that a dog who stiffens and growls during the procedure is communicating, not attacking. She is saying, “This is mine and I don’t want to share.” If you proceed (inappropriately, in her estimation) after giving you a polite warning, she may escalate to a more intense, “I really mean it; this is mine and you can’t have it.” Though her behavior may seem aggressive to inexperienced dog owners, the dog is actually showing admirable restraint and still may be a good adoption candidate for an appropriate home, without further intervention needed.
- If the shelter is uncomfortable placing dogs who exhibit the kind of behavior described above, its management could establish a behavioral foster program. Staff and/or volunteers who are knowledgeable and capable of working with behaviorally challenging dogs can assess and work to modify their guarding behavior in the shelter. Alternatively, the dog could be placed in a foster home (with one of those experienced dog-savvy volunteers or staff members) to see if this is one of those behaviors that ceases when the dog is no longer dealing with the stress of the shelter environment.
- Continue to consider dogs who show an extreme response to a reasonably mild threat to their resources as not-adoptable, unless the shelter has the expertise and resources to do significant behavior modification.
The shelter that I worked with a few years ago created a continuum that spelled out how dogs who offered varying degrees of resource-guarding behavior would be handled (see the table below). Each possible response corresponded with a specific recommendation. As a result, they began safely and successfully placing many dogs who, previously, would have been euthanized.
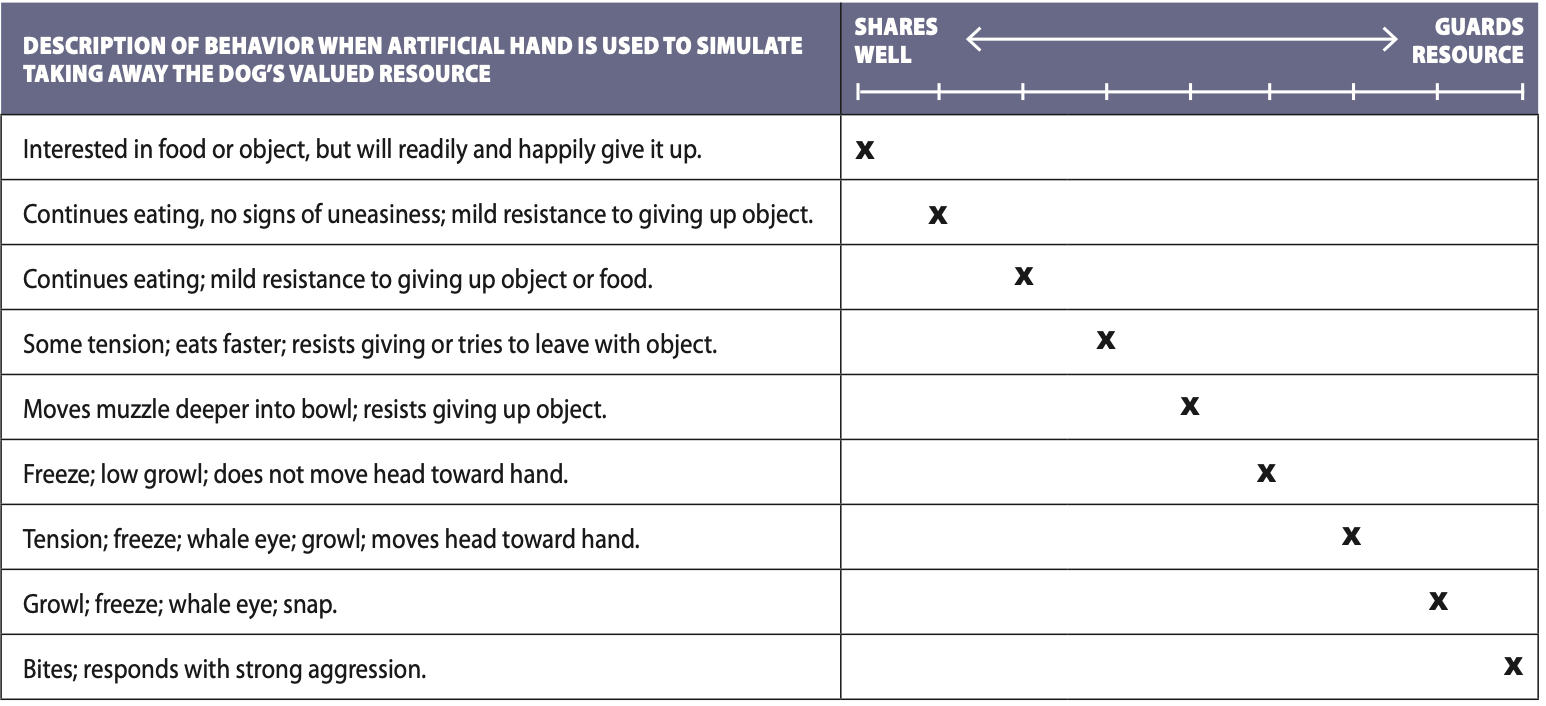
This table is an assessment form for a resource-guarding evaluation.
The left column describes possible responses that a dog might exhibit to a test in which the dog is given a valuable resource, such as canned food or a favorite toy, and then a handler attempts (with an artificial hand on a stick) to take the resource from the dog.
Dogs who display behaviors marked on the “Shares easily” end of the spectrum could be placed in any home. If their responses were marked somewhere in the middle of the spectrum, they were placed for adoption with restrictions (such as “no small children” or “experienced home only”), moved to the shelter’s behavioral foster program, or sent to a known rescue with behavior modification resources. If, however, their behavior was judged to match the most extreme descriptions at the “Guards Resource” end of the spectrum, they would be judged a candidate for euthanasia.
WORKING WITH A DOG WHO RESOURCE-GUARDS
Today, progressive trainers and shelter managers are aware that resource-guarding behavior can be managed, modified, and/or minimized. It requires understanding that this is a natural, normal canine behavior; a willingness to modify the dog’s environment in order to set him up for success; and, depending on the degree of drama that the dog brings to his guarding, a bit of work.

From the outset, adopters of all dogs (not just those with a history of guarding) need to be educated that the concept “I should be able to take anything away from my dog” is false and dangerous.
Then, whether the dog is living in a shelter or in a home, the first critical task is to make sure that no one (purposely or unwittingly) antagonizes the dog into aggressive behavior. All staff and volunteers or family members need to be thoroughly trained on procedures for working with the dog and minimizing guarding behavior; obviously, only staff or family members who are capable of and committed to staying cognizant and alert to these procedures should be allowed in the dog’s proximity.
When handling any item that has any value for the dog, people need to learn how to safely trade with the dog for anything he might covet, including bowls, toys, or anything he might have randomly grabbed, such as a dropped cell phone or keys (see “Protocol for a Safe Trade”).
When circumstances prevent a trade from taking place, the dog’s handlers should manage the environment to prevent the dog from having an opportunity to guard. For example, in a shelter, the staff might be instructed to move the dog to the other side of a double-sided kennel (and closing the door between them) before picking up items in the kennel; in a home, Mom would be instructed to put the dog outside before she picked up his empty food bowl.
YOU CAN MANAGE
Most resource-guarding behavior is much more easily managed or modified than once thought. In an appropriate adoption home, with family members mature and committed enough to adhere to management protocols, resource-guarding doesn’t have to be an issue at all.
The same is true in a shelter with adequate understanding and resources. Complications arise with young or careless handlers, those who resist the new understanding of guarding behavior, and/or those who may deliberately undermine management protocols.
Nevertheless, the time is long past for resource-guarding to be a capital offense for our canine companions. Dogs have a right to want to keep their good stuff. Manage the home or shelter environment so stress and conflicts over resources don’t have to occur. Implement “Trade” and guarding behavior modification protocols as needed to keep everyone safe and happy. And let them live.
Stomach Ulcers in Dogs: Symptoms, Causes, Diagnosis, and Treatment

Gastric ulcers also called stomach ulcers can be a pain – causing indigestion, reflux, and discomfort. But did you know that stomach ulcers in dogs are also a problem? It’s true!
The problem with stomach ulcers in dogs is that they can’t tell us when they have heartburn. The symptoms can be very subtle and may often be misdiagnosed or overlap with other conditions. Further, the problems that are often associated with ulcers in humans (stress and Helicobacter pylori infections) are not well-described or understood in dogs.
Stomach ulcers in dogs are usually gastroduodenal – meaning they are located in the stomach and upper intestinal tract, specifically the duodenum.
The stomach is comprised of four layers: The innermost is the mucosa, which is generally protected from the stomach acid by several important physiological mechanisms. The next layer is the submucosa, then the muscularis, the muscle that moves and contracts to cause peristalsis, the movement of the gastrointestinal (GI) tract. Lastly, on the outside, is the serosa.
A stomach ulcer is a spot in which the normal, healthy tissue has been eroded away. The spot becomes irritated and friable, and bleeds easily. Ulcers can involve only the mucosa or can go full thickness through to the serosa (or any layer in between). When the serosa is involved, the ulcer is considered perforated, as now the stomach contents can leak outside of the GI tract.
SIGNS OF STOMACH ULCERS IN DOGS
The symptoms of a stomach ulcer in dogs are varied and include decreased appetite, frequent burping or regurgitation, lip licking and drooling, vomiting with fresh or digested/dark blood, weight loss, abdominal pain, and dark, tarry stool (called melena). Of these, about 90% of dogs will present with vomiting.
Because these symptoms can represent an extremely large variety of problems, a thorough physical examination with your veterinarian is the first step in addressing these concerns.
There are no specific breed, sex, or age differences in patients with gastric ulcers. It is interesting to note, however, that extremely athletic dogs such as Iditarod sled dogs do have a higher prevalence of gastric ulcers. If you have an agility dog with these symptoms, gastric ulceration should be on the list as a possible cause. It is not well understood why this is the case.
Helicobacter pylori is well known as a cause of gastric ulceration in humans. This bacteria infects over 50% of people, though many never have symptoms.
H. pylori has also been isolated in dogs. However, its significance in relation to gastric ulcers in dogs is unknown. The GI tract of some dogs can be populated with H. pylori even though the dog never has symptoms of GI problems, while others have symptoms but no
H. pylori.
If gastric ulcers are present, and a cause cannot be found, H. pylori may be the culprit. It can be diagnosed either with a biopsy taken during endoscopy or by appropriate empirical therapy. Treatment is a month of the antibiotics metronidazole and amoxicillin, as well as antacids such as famotidine (Pepcid) or omeprazole (Prilosec).
CAUSES OF STOMACH ULCERS IN DOGS
There are a number of things that can cause ulcers in dogs.
NSAIDs/corticosteroids. The best-known cause of canine ulcers is the use of non-steroidal anti-inflammatory drugs (NSAIDs) and corticosteroids (such as prednisone and dexamethasone).
These drugs are amazing and useful for many conditions like acute injury and arthritis. As a result, they are prescribed frequently. Both decrease inflammation by inhibiting prostaglandins (PGs). However, if the dog’s prostaglandin levels are decreased too much and/or for too long, stomach ulceration can occur, since PGs are critical for maintaining a healthy stomach barrier against acid.
While NSAIDs are extremely beneficial drugs for the management of pain, they do not come free of side effects and risks. Therefore, when managing painful conditions, it is reasonable to start with alternative and complementary therapies such as physical therapy, joint supplements (e.g., glucosamine and chondroitin), fish oils, and acupuncture prior to using NSAIDs.
Unfortunately, steroids are critical for the management of certain autoimmune conditions such as immune-mediated hemolytic anemia and thrombocytopenia. In those cases, they cannot be avoided, so monitoring for the symptoms of gastric ulceration is critical.
Important: Steroids and NSAIDs should almost never be used in combination. There are rare cases such as autoimmune diseases where high doses of steroids will be used with very low doses of aspirin, but these are specific conditions. In most cases, the two should never be administered together. Doing so significantly increases the risk of life-threatening ulcers.
It is also crucial to remember not to administer over-the-counter products to your dogs. Ibuprofen, naproxen, meloxicam, ketorolac, and aspirin are all human NSAIDs. These can be extremely toxic to dogs, leading to gastric ulceration and kidney failure.
Endocrine disorders. Both Addison’s disease (a lack of cortisol) and Cushing’s disease (an excess of cortisol) are known to predispose to gastric ulceration. If your dog has either of these conditions, your veterinarian should be on the lookout for gastric ulcers.
Acute and chronic kidney disease. As kidneys fail, the body loses its ability to rid itself of toxins. Gastric acid levels go up, leading to ulcers. The signs of kidney disease can be exactly the same as that of ulceration, so treatment for both is usually started.
Tumors. Mast cell tumors are common in Boxers and other breeds. They secrete histamine (responsible for allergic reactions), which increases gastric acid secretion and predisposes to ulcers. Gastrinomas are tumors found in the stomach and will also release large amounts of gastric acid.
Other, less common causes. These include liver disease, inflammatory bowel disease, foreign bodies, and ingestion of caustic materials.
DIAGNOSIS
If your dog has symptoms of gastric ulceration, the first step is consulting with your veterinarian. A thorough physical exam and diagnostics are needed to rule out many of the above causes. This will include a nose-to-tail physical and bloodwork such as a complete blood count and a chemistry panel.
Findings may include anemia and low proteins (from blood loss though the ulcer) and an elevated blood urea nitrogen (BUN). In some cases, white blood cell counts may be elevated in response to inflammation.
Other tests that your veterinarian may be able to do include a barium study and abdominal ultrasound. In a barium study, a large amount of bright contrast is given to a dog by mouth. Radiographs are taken immediately and then at various predetermined intervals. The barium shows up bright white on x-ray. It can show defects in the stomach.
Ultrasound can also be used to evaluate for ulcers, although they can be very difficult to see. If a stomach mass such as a gastrinoma is causing the ulceration, then ultrasound may be able to identify it.
Specialized testing can more definitively diagnose an ulcer. Endoscopy is the gold standard, but this isn’t available at many clinics. Generally, you must be referred to a specialist for an endoscopy, which will be done under anesthesia. While asleep, a camera is passed down the esophagus and into a dog’s stomach and upper small intestine. Frequently small samples are taken (biopsy) for definitive diagnosis. The results can take one to two weeks.
HOW TO TREAT STOMACH ULCERS IN DOGS

Treatment for gastric ulceration depends on the underlying cause. If one is not found, then general treatment includes antacids, a bland diet, and gastroprotectants such as sucralfate. If a bacterial cause is considered (see “H. Pylori and Canine Ulcers,” above), then a specific therapy with antibiotics is recommended.
The major classes of antacids are proton pump inhibitors (PPIs) and H2 blockers. Both work in slightly different ways to lower gastric acid production. Famotidine (Pepcid) is an H2 blocker, while omeprazole and pantoprazole are PPIs.
Carafate (sucralfate) is another drug frequently used in the management of ulcers. It is a soothing agent that coats ulcerated areas. It is given as a tablet dissolved in water (a slurry). It can be give up to three times a day for relief of discomfort.
Other approaches may include a bland diet such as boiled chicken and rice. Probiotics can be added to food to maintain normal GI flora populations. Slippery elm and ginger may have some positive effects on GI ulcers, as well.
Perforated stomach ulcers are severe, life-threatening emergencies. A perforation occurs when the ulcer has eroded completely through all four layers of the stomach or intestine. This allows leakage of bacteria-laden stomach and intestinal fluid into the abdominal cavity, leading to massive inflammation, infection, and sepsis. Treatment for perforated ulcers includes stabilization of shock and infection followed by surgery to repair the ulcers.
PROGNOSIS
Prognosis varies and depends on the underlying cause. For uncomplicated ulcers and ulcers related to H. pylori, prognosis is good with appropriate treatment. It is important to know that they can recur. Discontinuation of NSAIDs and steroids (when possible) will improve the prognosis for cases related to these medications. In the case of perforated ulcers, prognosis is guarded.