[Updated February 7, 2018]
REHAB THERAPY FOR DOGS: OVERVIEW
1. Include your primary care veterinarian in your healthcare team; rehab specialists have the most to offer when they are confident your dog has been properly diagnosed.
2. Look for a rehab veterinarian or educated, experienced rehab practitioner it your dog has any sort of mobility problems or weakness. Ask about her training and experience; she should be proud to describe it!
About a decade ago, my then-young Bouvier, Jolie, had surgery to repair a herniated disc. From reading Whole Dog Journal, I was vaguely aware that veterinary physical therapy or rehabilitation existed. I decided that a similar modality would help Jolie, and set out to find a veterinary rehabilitation specialist to help us with her recovery.
I asked the veterinary orthopedist who had diagnosed Jolie’s condition, but while he thought some sort of pool-based therapy might be useful for my dog, he didn’t know anyone who offered such a service. I was unable to locate anyone in Georgia to help Jolie, but finally found a practitioner in Alabama – Jan Steiss, DVM, PhD, PT – who was able to give us a variety of exercises to practice with Jolie to speed her recovery and help with mobility, strengthening, and flexibility.
Photo by Samantha Fogg
Fast forward 10 years, and the field of veterinary rehabilitative medicine, sometimes referred to as Physical Medicine and Rehabilitation (PM&R), has blossomed. Just as physical therapy clinics for humans have popped up across the country over the past several years, so, too, has the field of veterinary rehabilitation grown. Still fairly young, the specialty is unknown to (and perhaps not completely understood by) many consumers and even veterinarians.
It’s Physical Therapy for Dogs! (But Don’t Call It That)
Veterinary rehabilitation uses many of the same modalities and techniques for animals as physical therapy does for humans; the two are similar in almost every way. However, the specific term “physical therapy” is legally reserved in most states for use by licensed physical therapists and for licensed physical therapists who work with humans only. The term is frequently used erroneously in canine rehab.
The American Association of Rehabilitation Veterinarians (AARV) was formed in 2007 to educate veterinary surgeons, veterinarians, and the public about the role this specialist can play in our dogs’ health. The organization defines a physical medicine and rehabilitation (PM&R) veterinarian as a doctor of veterinary medicine who has advanced training, expertise, and experience in the management of pain and loss of function through injury and illness.
Many PM&R veterinarians have post-doctorate training in the areas of orthopedic surgery, pain management, acupuncture, chiropractic, and/or rehabilitation that has led to specialization and/or certification in these fields. The AARV website elaborates, “The PM&R veterinarian is trained to evaluate the whole patient and not just focus on the perceived injury or illness. Following evaluation the PM&R veterinarian can perfect a treatment plan, monitor patient progress, and adjust therapeutic recommendations to achieve success.”
In a further bid to bring light and credibility to the field, a group of veterinarians have dedicated the past several years to creating a board-certified specialty in the discipline, the American College of Veterinary Sports Medicine and Rehabilitation. According to M. Christine Zink, DVM, PhD, the initiative is now at the American Veterinary Medical Association as the AVMA solicits comment from the public and the profession. If approved, Dr. Zink anticipates that the board certification will become a reality within the next year.
Veterinary Medicine Specializing in Mobility
To learn more about canine rehabilitation, we talked with Evelyn Orenbuch, DVM, vice president of the AARV. Dr. Orenbuch has practiced veterinary rehab medicine in the Philadelphia area for the past seven years, focusing much of her time on sports medicine for performance and working dogs. Several of her patients are nationally and internationally ranked agility and working dogs. Her next most commonly seen patient is the geriatric (usually arthritic) dog. Although soon to relocate to the Atlanta area, she took time to discuss this growing field with us.
WDJ: Why become a rehab vet? Why not an orthopedist or a “primary care” veterinarian?
A rehab veterinarian is someone who specializes in neuromuscular and musculoskeletal conditions. This is in contrast to an orthopedist, who is also highly trained in these areas, but uses surgery as his primary tool. Orthopedists are good at diagnosing, but they are typically not the ones who guide a client through correcting a condition or strengthening an area of the body.
Primary care veterinarians often don’t understand the broad range of conditions with which the rehab vet is familiar. I think veterinarians as a whole are getting better, but I remember when I graduated from veterinary school 15 years ago – I didn’t know how to diagnose a specific type of strain very well. Back then, we were told that if you didn’t see it on an x-ray, then it’s a soft tissue injury. But what type? A bicep strain? Iliopsoas? Medial shoulder instability? A bunch of different things can be soft tissue injury and each should be treated very differently!
courtesy of Caring Canine

The typical protocol is to put the dog on a nonsteroidal anti-inflammatory (NSAID), and recommend rest for the dog; we call it “R&R”: Rimadyl and Rest. If they can do surgery, they do surgery. “R&R” might fix the problem, but often not permanently; it might just mask the problem. We’ll sometimes see a chronic waxing and waning of the problem after using the R&R approach. Well, if it’s a strain of the teres major (a scapulohumeral muscle) or medial shoulder instability, until you treat it appropriately, it’s never going to get better!
Another classic scenario is when a dog has a little pain in his hind end, so he stops using it efficiently, and puts more weight on the front end. Then he becomes weaker and can’t get stronger because of the pain and fatigue due to muscle atrophy. You’ve seen them – old Labrador Retrievers with huge shoulders and skinny butts. Unless we’re proactive about strengthening the hind end, the dog is never going to come out of the spiral.
But now we have rehab vets. Ideally, when a veterinarian sees that the dog has a soft tissue injury, she’ll send him to a rehab vet, realizing that the dog needs to see a musculoskeletal specialist. The bottom line is that the field is becoming a lot more like human medicine, in terms of specialization. There is just too much to know to expect one veterinarian to be able to do it all – and it’s odd that we didn’t realize it sooner.
What services and modalities should we expect a rehab vet to offer?
Because a good portion of what is going on during rehab is working on building strength, flexibility, proprioception, and range of motion, the means of addressing those issues will vary depending on who is administering treatment.
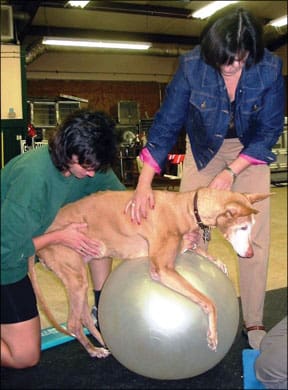
For example, I frequently use acupuncture and chiropractic. Other practitioners use those modalities and/or laser, ultrasound, electrical stimulation, hydrotherapy (underwater treadmill and/or swimming), massage, physio balls, wobble boards, land treadmills, cavaletti, weights, Thera-Bands, Chinese herbs, homeopathy, and nutrition. And that’s not an exhaustive list!
What kind of training should I look for in a rehab vet?
Ideally find someone who has trained at one of two schools in the U.S. The Canine Rehabilitation Institute (with locations in Florida, Maryland, and Colorado) awards the certificate of Canine Rehabilitation Therapist (CCRT) to veterinarians; the University of Tennessee University Outreach and Continuing Education Department, in conjunction with Northeast Seminars, offers a Certified Canine Rehabilitation Practitioner (CCRP) certificate.
But you might also find someone who has been practicing in the discipline for a long time. Maybe they don’t have one of the certifications, but perhaps they’ve spent a lot of time learning on their own, working with physical therapists, and getting invaluable practical experience. As with any specialist, you’ve got to ask them! A good rehab vet also usually has another modality such as acupuncture or chiropractic in her toolbox. Those kinds of tools allow the veterinarian to get a lot more done, including the ability to deal with both the condition and pain relief.
What are the typical goals of rehab and what are some examples of injuries or conditions we might see treated?
With hip dysplasia, we can use rehab to help with strength and flexibility. We find that we’re able to put off using pain medication and surgery to the extent that we’re seeing a lot of cases that would have needed surgery, now don’t need it.
If you know your dog has hip dysplasia early on, and you manage her, you can begin work early to prevent the hind end from becoming weak, and keep the pain at bay – pain that we often see in the low back and the muscles around the hips. Rehab can keep those areas loose, flexible, and strong.
After anterior cruciate ligament (ACL) surgery, we used to see protocols that called for the dog to start walking for five minutes one week, then 10 minutes the next, and so on. There wasn’t anything else, and particularly nothing to address stretching and strengthening.
Now we can prescribe passive range-of-motion exercises to do at home; light weight-bearing exercises to practice early on; and starting hydrotherapy anywhere from two to eight weeks post-op. And sometimes we see the use of lasers, electrical stimulation, or ultrasound to help with tissue healing. With rehab, animals get better a whole lot faster; they return not just to functionality, but to the condition in which they were in, pre-injury.
When should I consider consulting a rehab vet?
Any time you have an animal who needs to work on increased strength, proprioception, and/or flexibility. And pain management is huge – it’s a big part of rehab. In fact, there is a brand new pain management certification offered by the International Veterinary Academy of Pain Management (IVAPM) called the Certified Veterinary Pain Practitioner (CVPP). The need to recognize and address pain in our animals is essential to their healing and well-being.
Rehab and pain management go hand in hand. It’s important to realize that you need both to get anywhere when dealing with pain. We can throw drugs at it, but if the animal is in significant pain, we need to be doing other things as well. For example, if a dog is stiff and painful, even doing things as simple as stretching and massage can be a big part of pain management.
How do I find a rehab vet and do I need a referral?
Both certifying courses (mentioned above) have websites that list graduate practitioners, but remember that these lists will include veterinarians, veterinary technicians, physical therapists, and physical therapy assistants, as the certifications are open to all of those disciplines. The AARV has a list of veterinarians who do rehab, and the American Canine Sports Medicine Association has a listing of rehab practitioners.
Usually a person can make an appointment to see a rehab vet without a referral. However, most rehab veterinarians I know would prefer to have a referral to ensure that the animal has been looked at, and know that the animal is healthy. On the flip side, the benefit of us being vets is that we can determine that!
How is a physical therapist (PT) or registered veterinary technician (RVT) who has earned one of the certifications best utilized?
The way I see it, the veterinarian is the “physiatrist” – a rehabilitation physician. She oversees and manages the case as far as the rehab aspect goes. She can then send the animal to a physical therapist (PT) who will help develop the rehab protocol.
Alternatively, a rehab vet can create the treatment and send the animal to a registered veterinary technician (RVT) who’s been trained to carry out a rehab program. PTs can be an important part of the team; they are well trained in biomechanics and can be very good at coming up with appropriate exercises to strengthen a very specific muscle.
Photo courtesy Orenbuch Veterinary Rehabilitation

One of the issues we face if sending a dog to an RVT or a PT without a vet’s supervision is that RVTs and PTs are not trained to specifically recognize or diagnose animal diseases. Therefore, if an animal is not being overseen by a rehab vet, we worry that conditions could be overlooked, affecting not only the rehab therapy but the overall health of the animal.
What are challenges facing the field?
The biggest challenge is educating our veterinary colleagues so that they understand when the rehab vet needs to enter the picture.
In what sort of case do you think your perspective as a rehab veterinarian is particularly helpful?
I’ve seen many cases in which a conventional veterinary approach leaves the client wanting; there is a lack of knowledge about the other tools that are available to us. Take intervertebral disc disease, for example. You might have a dog who is partially paralyzed or weak in the hind end because a disc is pressing on the spinal cord. Often, we can avoid surgery through acupuncture and rehab, by waking up nerves and bringing the dog back to function.
I’ve seen cases in which hip dysplasia was assumed because when the dog’s hip was extended, it was painful, but the dog never had an x-ray! It might not even be hip joint pain – there are so many other things happening mechanically. It could be something going on up in the back. I see a lot of sacroiliac joint dysfunction and pain that can appear to be a hip problem, when it’s really in the back or iliopsoas.
My practice is a lot of sports medicine. About 40 to 50 percent of my patients are agility or flyball dogs. A big part of rehab is keeping the dog in top shape. We have people who spend a lot of money on competitions – entry fees, travel, etc. – that the last thing they want to do is bring a dog who is not in top form to a trial.
A few weeks ago, I was at an agility trial and met a woman and her dog. She was completely distraught; her dog needed only one more “double Q” (a qualifying agility standard run and a qualifying jumpers run on the same day) to earn his MACH (Master Agility Champion) title. On day one of the three day trial, the dog tweaked something, and by day two she had to pull him from the trial.
I saw him at the beginning of the third day, and he was clearly sore, and head-bobbing lame. It appeared he’d injured his shoulder. I treated the dog once, then reviewed with the woman how to rest, stretch, and massage the dog, and she followed my protocol to a T. Less than two weeks later, they went to a trial and the dog was feeling so good that on the first day he went off course! But on day two, he earned his MACH.
Lisa Rodier lives in Alpharetta, Georgia, with her husband and two Bouviers. She is also a volunteer with the American Bouvier Rescue League.







I have a small Maltese cross dog who is 10 months old. She has been training for agility and loves it. Over the last week she has suddenly become lame in her right leg and was diagnosed with luxating patella. The recommendation was a surgical procedure to fix the effected knee. My question, will she be able to do agility once her knee is fix? Will rehab be a better course for her?
Worried about her future as an agility dog, but she is such a sweet heart it doesn’t matter.
Thanks