Lymphoma accounts for 7 to 24% of all canine cancers and approximately 85% of all the blood-based malignancies that occur, making it one of the most common cancers found in dogs. Lymphoma – also referred to as lymphosarcoma – is not a singular type of cancer but rather a category of systemic cancers with over 30 described types.
Lymphoma occurs when there is a genetic mutation or series of mutations within a lymphocyte that causes the cells to grow abnormally and become malignant, ultimately affecting organs and body functions. Lymphocytes are the infection-fighting white blood cells of the immune system and are produced by the lymphoid stem cells in the bone marrow and lymphoid tissue in the bowel. Their role is to prevent the spread of disease, to provide long term immunity against viruses, aid in wound healing, and provide surveillance against tumors.
Lymphocytes are part of the lymphatic system – a network of tissues and organs that help rid the body of toxins, waste, and other unwanted materials. The primary function of the lymphatic system is to transport lymph, a fluid containing lymphocytes, throughout the body. Unfortunately, cancerous lymphocytes circulate through the body just as the normal lymphocytes do.
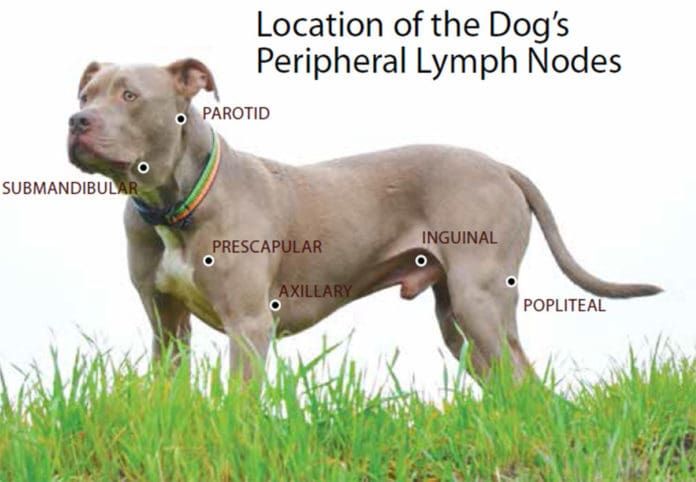
Although lymphoma can affect virtually any organ in the body, it most commonly becomes evident in organs that function as part of the immune system – the locations where lymphocytes are found in high concentrations – such as the lymph nodes, spleen, thymus, and bone marrow. Swelling occurs when the numbers of cancerous lymphocytes increase; one of the most common sites of accumulation are in the lymph nodes themselves, resulting in an increased size of these structures.
[post-sticky note-id=’377229′]
Canine lymphomas are similar in many ways to the non-Hodgkin’s lymphomas (NHL) which occur in humans, though dogs are two to five times more likely than people to develop lymphoma. The two diseases are so similar that almost the same chemotherapy protocols are used to treat both, with similar responses reported. NHL has been featured recently in the high-profile cases involving individuals who developed non-Hodgkin’s lymphoma after using the weed killer glyphosate (most highly recognized under its best-selling brand name, Roundup).
Because of its similarity to the human form, canine lymphoma is one of the best understood and well-researched cancers in dogs. It is one of the few cancers that can have long periods of remission, even lasting years, and although rare, complete remission has been known to occur.
CAUSE
The cause of canine lymphoma is not known. It is suspected that the cause may be multifactorial. In an effort to determine what factors affect the possibility of developing the disease, researchers are looking at the role of environmental components such as exposure to paints, solvents, pesticides, herbicides, and insecticides; exposure to radiation or electromagnetic fields; the influence of viruses, bacteria, and immunosuppression; and genetics and chromosomal factors (changes in the normal structure of chromosomes has been reported). It is thought that dogs living in industrial areas could be at a higher risk for developing lymphoma.
BREED DISPOSITION AND RISK FACTORS
Although the direct cause of lymphoma cannot be identified, studies have found that there are certain breeds that are at higher risk of developing the disease. The most commonly affected breed is the Golden Retriever, equally represented by B-cell and T-cell lymphomas (see below).
Other breeds showing increased incidence include the Airedale, Basset Hound, Beagle, Boxer, Bulldog, Bull Mastiff, Chow Chow, German Shepherd Dog, Poodle, Rottweiler, Saint Bernard, and Scottish Terrier. Dachshunds and Pomeranians have been reported as having a decreased risk of developing canine lymphoma.
Lymphoma can affect dogs of any breed or age, but it generally affects middle-aged or older dogs (with a median age of 6 to 9 years). There has been no gender predisposition noted, but there are reports that spayed females may have a better prognosis.
A recent large scale study published in the Journal of Internal Veterinary Medicine (Volume 32, Issue 6, November/December 2018) and conducted by the University of Sydney School of Veterinary Science in Australia, examined veterinary records for breed, gender, and neuter status as risk factors for developing lymphoma. A number of breeds were observed to be at risk that had not been previously identified as being in that category.
The study also demonstrated the opposite: Several breeds previously documented to have an increased risk of lymphoma failed to show an increased risk. Additionally, the study found males had a higher risk overall across breeds, as did both males and females that had been neutered or spayed. Mixed breeds generally had a decreased risk when compared with purebred dogs. While these findings may be inconsistent with other generally accepted risk factors, the study states, “These three factors need to be considered when evaluating lymphoma risk and can be used to plan studies to identify the underlying etiology of these diseases.”
LYMPHOMA TYPES AND SYMPTOMS
Typically, a dog who gets diagnosed with lymphoma will initially be taken to a veterinarian because one or more lumps have been found under the neck, around the shoulders, or behind the knee. These lumps turn out to be swollen lymph nodes. The majority of dogs (60 to 80%) do not show any other symptoms and generally feel well at the time of diagnosis.
Advanced symptoms depend on the type of lymphoma and the stage and can include swelling/edema of the extremities and face (occurs when swollen lymph nodes blocks drainage), loss of appetite, weight loss, lethargy, excessive thirst and urination, rashes, and other skin conditions. Breathing or digestive issues may be present if the lymph nodes in the chest or abdomen are affected.
Because the lymphatic system aids in fighting infection, fevers are often one of the first indicators of the disease. Additionally, since lymphoma affects and weakens the immune system, dogs may be more susceptible to illnesses, which can lead to complicated health issues. Lymphoma itself, however, is not thought to be painful to dogs.
Lymphoma can occur anywhere in the body where lymph tissue resides and is classified by the anatomic area affected. The four most common types are multicentric, alimentary, mediastinal, and extranodal. Each type has its own set of characteristics that determine the clinical signs and symptoms, rate of progression, treatment options, and prognosis. Furthermore, there are more than 30 different subtypes of canine lymphoma.
- Multicentric Lymphoma. This is the most predominant type of lymphoma, accounting for 80 to 85% of all canine cases. It is similar to non-Hodgkin’s lymphoma in humans. The first noticeable sign of this form is usually enlargement of the lymph nodes in the dog’s neck, chest, or behind the knees, sometimes up to 10 times their normal size, with the patient not showing any other distinctive signs of illness.
Multicentric lymphoma tends to have a rapid onset and affects the external lymph nodes and immune system; involvement of the spleen, liver, and bone marrow are also common. The disease may or may not involve other organs at the time of diagnosis, but it eventually tends to infiltrate other organs, causing dysfunction and eventually leading to organ failure.
As it progresses, additional symptoms including lethargy, weakness, dehydration, inappetence, weight loss, difficulty breathing, fever, anemia, sepsis, and depression may be observed. This form can also metastasize into central nervous system (CNS) lymphoma in later stages, which can cause seizures and/or paralysis.
- Alimentary (Gastrointestinal) Lymphoma. This is the second most prevalent form of canine lymphoma, however it is much less common, accounting for only about 10% of lymphoma cases.
Because it is in the digestive tract, it is more difficult to diagnose than the multicentric form. It is reported to be more common in male dogs than females. This type forms intestinal lesions, typically resulting in the manifestation of gastrointestinal-related signs, including excessive urinating or thirst, anorexia, abdominal pain, vomiting, diarrhea (dark in color), and weight loss due to malabsorption and maldigestion of nutrients.
The disease affects the small or large intestine, and it has the potential to restrict or block the passage of the bowels, resulting in serious and complicated health risks or fatality.
- Mediastinal Lymphoma. This is the third most common type of canine lymphoma, but it is still a fairly rare form. Malignant lesions develop in the lymphoid tissues of a dog’s chest, primarily around the cardiothoracic region. This form is characterized by enlargement of the mediastinal lymph nodes and/or the thymus. The thymus serves as the central organ for maturing T lymphocytes; as a result, many mediastinal lymphomas are a malignancy of T lymphocytes.
The symptoms of mediastinal lymphoma tend to be fairly apparent, involving enlargement of the cranial mediastinal lymph nodes, thymus, or both. It can also cause swelling and abnormal growth of the head, neck, and front legs.
Dogs manifesting with this disease may have respiratory problems, such as difficulty breathing or coughing and swelling of the front legs or face. Increased thirst resulting in increased urination can also occur; if it does, hypercalcemia (life-threatening metabolic disorder) should be tested for as it seen in 40% of dogs with mediastinal lymphoma.
- Extranodal Lymphoma. This is the rarest form of canine lymphoma. “Extranodal” refers to how it manifests in a location in the body other than in the lymph nodes. Organs typically affected by this type include eyes, kidneys, lungs, skin (cutaneous lymphoma), and central nervous system; other areas that can be invaded include the mammary tissue, liver, bones, and mouth.
Symptoms of extranodal lymphoma will vary greatly depending on which organ is impacted; for example, blindness can occur if the disease is in the eyes; renal failure if in the kidneys, seizures if in the central nervous system, bone fractures if in the bones, and respiratory issues if in the lungs.
The most common form of extranodal lymphoma is cutaneous (skin) lymphoma, which is categorized as either epitheliotropic (malignancy of T lymphocytes) or nonepitheliotropic (malignancy of B lymphocytes.) In the early stages, it usually presents as a skin rash with dry, red, itchy bumps or solitary or generalized scaly lesions and is fairly noticeable as the condition causes discomfort.
Because of this presentation, it is sometimes initially mistaken for allergies or fungal infections. As it becomes more severe, the skin will become redder, thickened, ulcerated, and might ooze fluids; large masses or tumors can develop. Cutaneous lymphoma can also affect the oral cavity causing ulcers, lesions, and nodules on the gums, lips, and roof of the mouth (sometimes mistaken at first as periodontal disease or gingivitis).
SUBTYPES
Within each of the four types described above, the disease can be categorized further into subtypes. There are more than 30 different histologic subtypes of canine lymphoma identified; some researchers theorize that there may be hundreds of subtypes, based on molecular analysis of markers, classifications, and subtypes of lymphocytes.
At the moment, further knowledge about the various subtypes would probably not result in significant changes in treatment protocols. In the future, targeted therapies for subtypes could lead to more effective treatments and improved prognosis.
The two primary and especially relevant subtypes are B-cell lymphoma and T-cell lymphoma. Approximately 60 to 80% of lymphoma cases are of the B-cell lymphoma subtype, which is a positive predictor; dogs with B-cell lymphoma tend to respond positively to treatment with a higher rate of complete remission, longer remission times, and increased survival times. T-cell lymphoma constitutes about 10 to 40% of lymphoma cases and has a negative predictive value based on not responding as well to treatment and for being at a higher risk for hypercalcemia.
DIAGNOSING CANINE LYMPHOMA
Early detection and treatment are essential to ensuring the best possible outcome for lymphoma cases. Because dogs generally feel well and there are often only swollen lymph nodes (with no pain exhibited) as a symptom, catching the disease early can sometimes be quite difficult. As a result, the cancer can be quite advanced by the time a diagnosis is made. (Lymphoma is not the only the disease that creates swollen lymph nodes; this symptom does not guarantee your dog has lymphoma.)
Because multicentric lymphoma accounts for the majority of cases, an aspirate of an enlarged peripheral lymph node is usually sufficient to reach a presumptive diagnosis of the most common types of lymphomas.
Although diagnosis from cytology is fairly easily obtained, it does not differentiate the immunophenotype (B versus T lymphocyte). Histopathologic tissue evaluation (biopsy) is required in order to identify the type with the process of immunophenotyping.
Immunophenotyping is a molecular test usually performed by flow cytometry (a sophisticated laser technology that measures the amount of DNA in cancer cells) that classifies lymphomas by determining if the malignancy originates from B lymphocytes or T lymphocytes. Determining whether a lymphoma is B-cell or T-cell is invaluable as it provides the best predictive value; the adage “B is better, T is terrible” reflects this in its simplest form.
Diffuse large B-cell lymphoma (DLBCL) is the most common histologic subtype of lymphoma occurring in dogs. Most intermediate to high grade lymphomas are B-cell lymphomas – they tend to respond better and longer to chemotherapy than T-cell lymphomas; however, dogs with T-cell lymphoma have been known to go into remission for several months.
Another phenotyping test, the PCR antigen receptor rearrangement (PARR), can determine whether the cells are indicative of cancer or more consistent with a reactive process. For example, because the lymph nodes in the area of the jaw are reactive, the PARR test can help determine if cancer is present or if the dog just badly needs his teeth cleaned. The PARR test can also be used to detect minimal residual disease. Research is continuing to determine if this will be a useful clinical marker of early recurrence.
To ascertain the patient’s overall health, a complete physical exam will be performed; additional diagnostics often include a blood chemistry panel, urinalysis, x-rays, ultrasounds, and other forms of diagnostic imaging (these tests are also used for staging the disease).
In particular, it is important to screen for hypercalcemia. Hypercalcemia is a condition in which the hormone PTHrP (parathyroid hormone-related peptide) creates dangerous elevations in the blood calcium level. This well-documented syndrome is associated with lymphoma in dogs and is most often seen in T-cell lymphomas.
About 15% of dogs with lymphoma overall will have elevated blood calcium levels at diagnosis; this increases to 40% in dogs who have T-cell lymphoma. The condition causes additional clinical signs including increased thirst and urination, and, if left untreated, can cause serious damage to the kidneys and other organs and be life-threatening.
Unfortunately, due to the rapidly progressive nature of lymphoma, decisions regarding treatment need to be made as soon as possible after diagnosis. Unlike most other forms of cancer, lymphoma requires urgent care; without treatment, the median survival time is one month after diagnosis. Therefore, owners should be prepared to start treatment on the day of diagnosis, or within a day or two at most.
STAGING
Once a diagnosis of lymphoma has been made, the stage (extent) of the lymphoid malignancy should be determined, and to assess this, several tests are recommended: lymph node aspirate, complete blood count, chemistry panel, urinalysis, phenotype, thoracic and chest radiographs, abdominal ultrasound, and a bone marrow aspirate.
Staging is prognostically significant; in general, the more extensive the spread, the higher the stage, the poorer the prognosis. However, even dogs with advanced disease can be successfully treated and experience remission. These tests also provide information about other conditions that may affect treatment or prognosis. The World Health Organization (WHO) five-tier staging system is the standard used to stage lymphoma in dogs:
- Stage I: Single lymph node is involved.
- Stage II: Multiple lymph nodes within in the same region are affected.
- Stage III: Multiple lymph nodes in multiple regions involved.
- Stage IV: Involvement of liver and/or spleen (in most cases lymph nodes are affected but it is possible that no lymph nodes are involved).
- Stage V: Bone marrow or blood involvement, regardless of other areas affected and/or other organs other than liver, spleen and lymph nodes affected.
In addition, there are two categories of clinical substages. Dogs are categorized with substage A if clinical signs related to the disease are absent, and categorized as substage B if clinical signs related to the disease are present (systemic signs of illness).
TREATMENT
Although canine lymphoma is a complex and challenging cancer, it is one of the most highly treatable cancers and most dogs respond to treatment. In fact, many dogs with lymphoma outlive animals with other diseases such as kidney, heart, and liver disease. While lymphoma is not curable, the goal with treatment is to quickly achieve remission for the longest period possible thus giving dogs and their owners more quality time together. It is essential that the type of lymphoma is identified as the type impacts treatment and prognosis. And because lymphoma is a very aggressive cancer, it is important to begin treatment as soon as possible.
Since lymphoma is a systemic disease that affects the whole body, the most effective treatment is also systemic in the form of chemotherapy, which provides many dogs with prolonged survival times and excellent quality of life, with little or no side effects.
The specific type of chemotherapy treatment used will vary based on the type of lymphoma. Other factors to consider when choosing a protocol are the disease-free interval, survival time, typical duration of remission, scheduling, and expense. Again, dogs with B-cell lymphoma tend to respond much more favorably to treatment than those with T-cell.
Because lymphoma is so common in dogs, there has been a substantial amount of research and testing of many different combinations of chemotherapy treatments. Multiagent chemotherapy protocols are considered the gold standard of treatment and have shown to provide the best response in terms of length of disease control and survival rates, as compared to single agent protocols.
The Madison Wisconsin Protocol, also known as UW-25 or CHOP, is a cocktail of drugs modeled after human lymphoma treatments and is widely considered to be the most effective treatment for intermediate- to high-grade canine lymphomas. This protocol utilizes three cytotoxic chemotherapy drugs – cyclophosphamide, doxorubicin (hydroxydaunrubicin), and vincristine (brand name Oncovin) – in combination with prednisone (CHOP). The prednisone is typically given daily at home as a tablet with the remainder of the protocol agents administered by an oncology specialist.
On average, 70 to 90% of dogs treated with CHOP experience partial or complete remission. For dogs with B-cell lymphomas, 80 to 90% can be expected to achieve remission within the first month. The median survival time is 12 months with 25% of patients still alive at two years. For T-cell lymphoma, about 70% will achieve remission with an average of six to eight months survival.
Other treatment options include the COP chemotherapy protocol (cyclophosphamide, Oncovin [vincristine], and prednisone), vincristine and Cytoxan; single-agent doxorubicin; and and lomustine/CCNU. As a primary treatment, single-agent doxorubicin can result in a complete remission in up to 75% of patients with median survival time of up to eight months, though cumulative treatment with doxorubicin may result in cardiotoxicity, so the protocol may be contraindicated in any dog with evidence of or a history of pre-existing heart disease. Lomustine/CCNU is reported to be the most effective treatment for cutaneous lymphoma.
REMISSION
Remission is the condition in which the cancer has regressed. Partial remission means that the overall evidence of cancer has been reduced by at least 50%; complete remission indicates that the cancer has become undetectable to any readily available diagnostic screening (but it does not mean that the lymphoma has left the dog’s body, only that it has been treated into dormancy).
A dog in remission is essentially indistinguishable from a cancer-free dog. The lymph nodes will return to normal size and any illness related to the cancer usually resolves. Overall, there is approximately a 60 to 75% chance of achieving remission regardless of the protocol selected.
Studies show that the average time for a dog to be in remission the first time is eight to 10 months, including the period of chemotherapy administration. Remission status is continually monitored; for dogs with enlarged lymph nodes it typically involves checking the size of the lymph nodes. For dogs with other types of lymphoma, periodic imaging may be recommended. The Lymphoma Blood Test (LBT) from Avacta Animal Health can also be used monitor status since LBT levels can increase less than eight weeks before relapse.
Unfortunately, remission eventually relapses in most cases, but many dogs can restart chemotherapy with the hope of regaining remission status. At times, the same chemotherapy protocol may be used. For dogs successfully treated initially with the CHOP protocol, restarting CHOP at the time of the first relapse is typically recommended. About 90% of those treated with a second CHOP protocol will achieve another complete remission, however, the duration is usually shorter than the first time.
If a patient does not respond to the first CHOP protocol before completion or the treatment fails during the second protocol, the use of rescue protocols can be attempted; these consist of drugs that are not found in the standard chemotherapy protocols and kept in reserve for later use.
Commonly used rescue protocols include LAP (L-asparaginase, lomustine/CCNU, and prednisone) and MOPP (mechlorethamine, vincristine, procarbazine and prednisone). These are less likely to result in complete remission and some dogs will only achieve a partial remission, with an overall response rate of about 40 to 50%, and a median survival rate of 1.5 to 2.5 months.
Because cancer cells evolve over time, the disease can become resistant to certain drugs. Further treatments can be given, but it can become more difficult to achieve remission a second or third time and there does not appear to be any substantial effect on survival times.
OTHER TREATMENT OPTIONS
Here are some compelling alternatives to consider in addition to the standard protocols described above:

- Prednisone. This is usually a component of most lymphoma treatment protocols because it actually destroys lymphoma cells. It can even be administered as a standalone treatment. The average survival time without chemotherapy is about one month but treating with prednisone alone can increase this to about two to three months, with an average of 50% responding.
- Tanovea-CA1 (rabacfosadine). This is a promising new advancement in treating canine lymphoma. This drug has been conditionally approved for use by the U.S. Food and Drug Administration (FDA), pending a full demonstration of its effectiveness (additional field studies are currently taking place to obtain full approval). [post-sticky note-id=’377235′]
Tanovea-CA1 is designed to target and destroy malignant lymphocytes and can be used not only to treat dogs that have never received any treatment but also those no longer responding to chemotherapy. It has demonstrated a 77% overall response and a 45% complete response rate. It is administered by veterinarians in five treatments every three weeks via intravenous infusion and is shown it to be generally well-tolerated.
- Bone Marrow Transplant. One of the newest approaches to treating canine lymphoma is the bone marrow transplant – a form of stem cell therapy – modeled after a method used in human medicine. The process involves the dog receiving and completing CHOP therapy (which puts the cancer in remission); the harvesting and preservation of healthy stem cells from the patient; the administration of radiation to destroy any remaining cancer cells; and the returning of healthy cells to repopulate and restore blood cells.
In humans, the cure rate is about 40 to 60%; the procedure has been determined to be safe for use in dogs with cure rates of 33% for B-cell lymphomas and 15% for T-cell lymphomas. The process is expensive ($19,000 to $25,000) and requires about two weeks of hospitalization. Currently there are only two locations in the U.S. offering the procedure: the North Carolina State College of Veterinary Medicine (in Raleigh) and Bellingham (Washington) Veterinary Critical Care.
At some point lymphomas become resistant to treatment and no further remissions can be obtained. Eventually the uncontrolled cancer will infiltrate an organ (often the bone marrow or the liver) to such an extent that the organ fails. Under those circumstances, it is best to focus on high quality of life for the longest possible survival time.
PROGNOSIS
Like most cancers, the eventual prognosis for dogs with lymphoma isn’t very uplifting. But it is a very treatable cancer, and dogs live well and longer with treatment. Several prognostic factors have been identified for estimating a dog’s response to treatment and survival time:
- Dogs with signs of systemic illness (substage B) tend to have a worse prognosis than dogs with substage A.
- Dogs with lymphoma histologically classified as being either intermediate- or high-grade tend to be highly responsive to chemotherapy, but early relapse is common with shorter survival times.
- Dogs with lymphoma histologically classified as being low-grade have a lower response rate to systemic chemotherapy yet experience a positive survival length advantage when compared to intermediate- or high-grade tumors.
- Dogs with T-cell lymphomas have a shorter survival time when compared with dogs with B-cell based malignancies.
- Dogs with diffuse alimentary, central nervous system, or cutaneous lymphoma tend to have shorter survival times when compared to dogs with other anatomic forms of lymphoma.
- Presence of hypercalcemia or anemia or a mediastinal mass are all associated with a poorer prognosis.
- Intestinal lymphoma has a very poor prognosis.
- Expectations for cases with Stage V lymphoma are much lower than those assigned to Stages I to IV.
- Prolonged pre-treatment with corticosteroids is often a negative prognostic factor.
- Ultimately, the estimates for survival times depend on the type of lymphoma combined with the stage and the treatment option selected (if any).
- In the absence of treatment, most of the dogs diagnosed with lymphoma succumb to the disease in four to six weeks.
- The median survival time with a multi-agent chemotherapy protocol is 13 to 14 months.
- Traditional chemotherapy results in total remission in approximately 60 to 90% of cases with a median survival time of six to 12 months.
- In about 20 to 25% cases, dogs live two years or longer after initiation of standard chemotherapy treatment.
- Dogs treated with rescue protocols have a survival rate of 1.5 to 2.5 months.
- Studies indicate that dogs who underwent splenectomy show a median survival rate of 14 months.
- Complete cure is rare, but not unheard of. Bone marrow transplants show promise and potential for increased cure rates.
Above all, remember that prognoses are only guidelines based on average accumulative experiences. They are numbers, and as a dear friend and veterinary oncologist has said to me many times, “Treat the dog, not the numbers.”






I am an oncology nurse. Your article is accurate and well written. However, you do not address the cost of these drugs. Humans who have insurance can still be financially devasted by their co-pays. You also do not address the intense side effects or quality of the dogs life while undergoin g treatment.
My Kirby had T cell Stage 3 Lymphoma. We used the CHOP therapy minus the doxorubicin. (very nasty) He lived 8 months. Total cost without insurance $15,000. At the beginning of treatment his health was very good. When we entered the sixth month his health began to decline. Organs began to not work as well. By the eight month we were battling kidney issues., hand feeding and extremely tired. We made the decision at this point to say goodbye, be cause we did not want him to suffer any further. We had just come back from vacation with him and he gave us all he had. I worked very closely with a holistic vet, and he was on many supplements. That is very important. I would never do chemotherapy again. I would look for more holistic treatments immediately and enjoy the time together..There are many new treatments available (stem cell, oxygen therapy, vit c therapy, and so on).
How does one find a wholistic Vet that does stemcell therapy?
The best way is to google holistic veterinarians in your area. Cal all of them. If there is a large clinic in your area, call them. If you go to a dog park, ask people there. Groomers might know as well. Also trainers will know. I hope
this helps.
Thank you for pointing out these two very important considerations. ❤️
You do not address the more rare intestinal small cell lymphoma, which is more common in cats. My dog has it, and the treatment protocol is Prednisone and chlorambucil. Remissions can be obtained, and changes in diet can help with symptoms of digestive upset.
It would be helpful if someone would look into this form of lymphoma.
My dog (7 year old male lab mix) was just diagnosed with small cell lymphoma and I was given the same treatment recommendation. What diet changes did you find were helpful? I’ve spent many hours on PubMed trying to get a better grasp of the diagnosis and situation…
You did not mention what happens to dogs who have neither T or B cells. My dog fell into that category. She had null cells the rare firm that less than 3 to 5 percent of dogs get and very little is known about what to do.
The author is incorrect in stating that a “histopathologic tissue evaluation (biopsy)” is the only way to do immunophenotyping of canine lymphoma. Flow cytometry is performed using living cells obtained from an enlarged lymph node via fine-needle aspirate (the same way cells are obtained for cytology) which are placed into a special transport medium and sent to the laboratory for testing. This is very important, as fine-needle as pirates may be done in the awake dog, while biopsy typically requires general anesthesia. Fine-needle aspiration is a less expensive and much easier test to perform than biopsy!! Similarly, the PARR test, if indicated, is also performed on fine-needle aspirate samples.
Very thorough -thank you! My little guy fought multicentric lymphoma all of 2018… & while I learned all these things during that battle, believe many will find this in-depth article informative and very helpful, UP FRONT. Dog parents can know what to look for! Looking back, had found out my sweet boy had this disease for several months before it was identified & diagnosed as such. In part, because he was happy, energetic, playful and inquisitive. – definitely not sick! I was blind-sided. As for treatment, my little guy went through all these protocols, one by one, along with alternative and holistic therapies. I might add… as for alternative therapies, found their place in treatment protocol is still not recognized by many veterinarians… However, dog parents who are suiting up to battle this dreaded disease might just find them worthy of consideration, just as I did.
Last spring my always healthy, 8 year old Chow mix became ill. She was thoroughly examined, and her vet ran every blood test available. The vet diagnosed uveitis, and started prednisone and antibiotics. She seemed to recover fully, but only for about two months. Same symptoms again, lack of appetite, labored breathing, lethargy. Back to vet for more blood tests, exam by two different vets, and full body x-rays. At no time did any of her lymph glands feel swollen. More steroids and antibiotics. After 10 days on the drugs she seemed to be getting worse. Luckily, my vet is open weekends. This time we could both feel multiple swollen glands. Vet took a biopsy and sent to lab. We were hopeful of treatment.
But two mornings later, at around 5 am, I awoke to her having a massive seizure in her sleep. She never regained consciousness, and after another major seizure about 45 minutes later, she passed away on the floor next to my bed. Her vet was shocked she went so quickly. We received the lymphoma results from the lab two days later. J
First let me say how sorry I am about your wonderful Chow mix. It is extremely heartbreaking to lose our companions.
My experience with Lymphoma for my 10 year old sweet Cavalier has been a roller coaster ride. In May of this year one morning one side of my dog’s face was swollen and then hour later, the swelling went down. Went to vet who noticed swollen lymph nodes on both sides of his neck and under the arm. A fine needle aspirate confirmed Lymphoma. Was put on Prednisone while I was deciding on chemo and 2 weeks later we went with it. All the while my dog was happy, eating, walking while he had chemo and Prednisone for the first month. Then in July things changed. He seemed to have aged 10 years, had on and off diarrhea from chemo and would sometimes hide. Yet he continued to eat, play and was actually gaining weight. On July 25 he developed facial paralysis on one side of face, which was awful. Oncologist didn’t know what caused this as he had never seen this before, so I ran around having his teeth checked for infection, thyroid tests and ear exam. In Aug. chemo wasn’t working so well and he was slowing down. He began to be afraid of going to oncologist and would stress out. He began having neurological problems and severe eye problems. Rescue protocol was tried at end of Aug. but didn’t have the results the oncologist would have liked and yet my dog continued to eat and play and walk. In Sept. was told I could try another protocol but it would be short lived and I should think of dog’s quality of life. Let him know in a week. Gave him low dose of Prednisone and Gabapentin to take. But oncologist had neurologist look at my dog on our final visit, and he said paralysis was due to disease progressing and he had COMS which affects the brain. whereby my beautiful boy would just freeze and not move and look scared
And confused. A week later he was still waking me up every morning and would look ok but then a few hours later he would breathe heavy, then be fine, then pant really heavy and then the lymph nodes enlarged and returned making it hard for him to sleep at night as he struggled to breathe. Yet he continued to eat, gain weight and be happy to see company. He only lasted as long as it would have been if he was on Prednisone only and I wish I had gone that route because I believe the chemo brought all this out and while he was suffering, didn’t let it show because that is how dogs are. We decided to let him Go a few days later and I am still heartbroken with that because I didn’t want to do it. This stoic little dog went through 2 surgeries, had mitral valve disease and PSOM but was always a happy boy. He will be missed.
Thanks for shareing.bless you and your dog
Cam,
we have a cavalier also, 2 yrs old, birthday this coming Nov1. we also have his brother.
about a week ago, stopped eating and very lethargic. took him to our vet, two days ago. they did some blood work etc, diagnosed as lymphoma . spleen enlarged, abdominal lymph nodes, fluid in the abdomen. we started him on steroid until test results come back in a few days. we are now trying to get him into an oncologist sometime this week. seems everyone is busy and appointments 2-3 weeks out. out Vet is going to get involved to get Lance in early this week.
We were shocked at this rapid change in his eating, and further shocked that it can happen in a 2 yr old. we have gone to great lengths with both of them to keep them healthy and get them in for all their exams etc. we make our own food with chicken, veggies, salmon turkey.
we also are leaning toward no chemo but will wait for further conclusive diagnosis. we also want Lance to be as happy and healthy as he can for whatever time he has left instead of treatment visits. we welcome your further comments. of course, we are heartbroken.
Hi Kathy, we just out 2 days ago that our 2yr old cavalier has lymphoma. We are devastated. Your post stood out as you are dealing with the same situation. How is Lance doing? Did you do chemo? We are evaluating our options so if you have anything you found helpful please share. Thx
My (Birthday was just in Dec) 3 year old Boston Terrier was diagnosed in December. She had a tiny swollen lymph node. Came back Muticentric Lymphona. We are devasted. We got right in with a oncologist. Oncologist couldn’t believe that she was positive. Too many “maybes” for treating with chemo. Basically told, 12-14 months average with chemo. No promises if she would be sick. We can’t do that to her. My vet is a holistic vet so we started her on Chinese herbs on 1/6/2021. Today is 1/23/21. She appears to be having equilibrium issues. Also in the last few days she has had a loss in appetite.
I’m so afraid that this is the start of the end for her. She is our baby. I’ve told my husband that I won’t watch her suffer. It’s quality not quantity. I am calling my vet today to see about starting Prednisone now. I know it only buys a little more time.
Vaccines are a factor, especially if there is an uptick in the past few years
because of the increase in the number of vaccines.
My dog was diagnosed with lymphoma several years ago. We did chemo and she went into a strong remission which continues today. I think it is very important to note, however, that since then we have had her on a protocol of medicinal mushrooms (turkey tail, reishi, maitake and chaga) plus Chinese herbs. We are using Wei Qi Booster that boosts immunity and another herbal formula called Si Miao San. It is important, especially with the Chinese formulations, to have your dog see a knowledgeable holistic vet to monitor your pet but I think that the medicinal mushrooms are very safe to use. We use mushrooms from Mushroom Science because they are very pure. Also, the Chinese herbs and lots of other cancer support is available at Well Pet Dispensary online.
Dear Kim
I would be grateful if I could get in touch with you. My dog has just been diagnosed with B cell Lymphoma (high grade) and I would like to explore the mix of holistic treatment and chemotherapy. I am heartened by your dog’s success in this and I would like to explore this. Thank you.
I would love to explore this route, my 6 year old boxer is being diagnosed as I speak. Please help! I can’t even begin to think about life without her.
What type of lymphoma did your dog have? My girl was just diagnosed with Cutaneous Epitheliotropic Lymphoma. T cell skin cancer. It is not anywhere else at the moment. I can’t find a holistic vet near me that has experience with this. My oncology appointment is Monday. I am not sure if she is familiar with holistic medicine. How and where did you find the information you got on what holistic things such as the mushrooms to give your dog? Any details would be most appreciated.
Thank you
Laurie
I hope that Whole Dog Journal will do a follow up article on holistic and complimentary treatment for canine lymphoma and other cancers. It is challenging (and sometimes costly) but the information and the tools are out there so don’t give up! All in all, the natural remedies are very affordable compared to conventional treatments but of all cancers, it does seem as if lymphoma responds really well to chemo. There are also natural supplements you can use even during chemo. VCA Animal Hospitals seem to be getting more involved in the use and dissemination of info about natural additions to treatment. Sometimes it is also hard to know the right doses or combos of natural supplements, but again, the information is out there.
My oncologist at the VCA was not too versed in holistic treatments. Wanted to give my dog Liquid Gold but he felt it would be useless. Because I didn’t know if any of the holistic treatments would interfere with chemo, I was hesitant.. Asked about CBD oil and he said well it couldn’t hurt. Used it throughout short lived chemo. Asked about tumeric. He said he wasn’t familiar with it but later I did give it to my dog. My dog never went into remission and he is gone now but I wish my oncologist had been more knowledgeable.
I am neither a vet nor a professional nutritionist but here is our story:
My 12 year old English Setter was diagnosed with oral lymphoma in January 2019. Prognosis for his condition was 60 days, four months at the most. At that stage of his life, I chose not to do chemo. Instead I intensively researched holistic diets for dogs with cancer. I thus began creating home cooked meals for Merlin. This food was mixed with a premium dry kibble as I wanted to be sure he was getting adequate vitamins and minerals. Supplements were wild salmon oil in the morning, and K9 Power Show Stopper in the evening. To keep his mind active, we continued training in obedience. He earned his final CD leg in March!
It is almost September and Merlin is still with us! Yes, he has declined and my guess is that sadly he does not have much time left. However, he still wakes up with a wagging tail and eating heartily! My extremely competent vet is amazed. Merlin is the first dog he has treated that has lived so long.
Cooking for your dog does is not time consuming. A crockpot plus organic meats, vegetables and bone broth is all one needs. Yes, it added about $200 a month to my grocery bill but how can you put a price on the health and longevity of your best friend?!
My 7 year border collie was diagnosed with multicentric Lymphoma.
I decided to change his diet for a natural diet prepared at home. He is doing very well for now and I hope he will be able to remit. Thank you for your comments Deb!
Our 4 &1/2 year old extremely active and healthy Collie recently passed on from Lymphoma. I was baffled by this article’s statement that it is good news if the diagnosis for a dog’s cancer is Lymphoma. Since the article goes on to state that the median length of life after treatment with (extremely expensive) chemotherapy is one year, how can this possibly be considered good news? I was pleased to see the success experienced by Deb Ashlock’s English Setter and found Kim McDonald’s recommendations for medicinal mushrooms and Chinese herbs encouraging. We were blindsided by the diagnosis.
I will add that if introducing a holistic home cooked diet for your dog, the addition of a few Tablespoons oatmeal to each meal (1 C whole oats that have been processed in a food processor to a fine texture and then cooked with about 1&3/4 cups boiling water to a full boil, stirring ) can help to prevent diarrhea. The excess oatmeal can be refrigerated for later use.
I am convinced that daily runs in a park that had been treated with pesticides ( even though we waited for about a month after treatment before using it) was a factor in our Collie’s illness.
Catherine
I definitely agree that the pesticides in a park caused lymphoma in your dog. My dog used to love to roll on his back on the grass and did so many times over the 10 years. There would be an excessive amount of these blue pellets and all of us dog owners let our dogs play on the fields, because we didn’t know. It is amazing to me how many dogs in our neighborhood all passed from Cancer, Unfortunately, I would love to put the people who own the park on notice and have them be accountable, but as the fields belong to a very wealthy private academy here, I don’t think we have a prayer of that happening. I just don’t want other dogs to get Lymphoma like my dog. It was first evidenced as a small cyst on his back which grew to a cauliflower like mass but all the while our vet kept saying it was a cyst even while it was full blown for awhile and then in Nov. 2018 was removed and turned out to be a tumor. That probably was the beginning of the end for my dog because in Ma 2019 he was diagnosed with Lymphoma and passed in Sept. with complications from this disease.
Our Trina was diagnosed with stage V lymphoma 6 months ago. She went through 19weeks of CHOP treatment. Initially was on prednisone but once we found the adverse effects and her not acting like herself consulted with a holistic dr at week 3. Has been in remission since week 4. Now eats not kibble but a balance homemade cooked meal- we freeze it for a week at a time.
Along with cbd oil, a probiotic, vrs omega fish oil, yunan baiyao, six gentle pets, and mushroom kings—- she has been doing great for a pup w stage v lymphoma initially with thrombocytopenia… bleeding out of her rectum, vomiting, bruising, and blood in her eyes…
With finishing the last treatment we are now told to be on a monthly oral
Chemo pill.. and a small
Dose of injectable chemo again… vincristine and chlorambucil… we do not want to continue chemo and are considering tumeric paste… but are hesitant because it’s hard to attribute whether it was the nutrition change, chemo, or both that have helped her…
The longer between treatments she’s been off chemo… she acts like a puppy again… she’s a 7yr old pitbull…
Hello
Our 12.8 month lab Mickey had a tumor
And diagnosed with lymphoma at age 9
He went into remission until age 12.8
When two inner ear infections and and abscess near his ear occurred. We treated these with Antibiotics and it took a solid month for him to recover. He also had some increase in kidney values.
Because of the kidney issue I avoided any invasive procedures. We took him to an internist for the kidney issue. When the ear infection resolved a tumor grew on the ear that was infected. At the internist
Appointment we had a sample of the ear tumor taken which was found to have lymphoma cells. Still I hesitated to treat him any further due to the kidney issue,
And the fact that it took the ear so long to heal. Also his age was a factor. At that point he was acting fine, taking walks, eating well and having good life quality.
The vet recommended seeing an oncologist immediately
We went for a consult
Immediately she was pushing chemo .As I questioned his recent health issues she just said it was not a problem
My gut said different.
She recommended prednisone and elapar for the tumor before actually starting chemo
We agreed to that
As soon as he started the prednisone
He had diarrhea I called the oncologist
Two days in a row with pa return call from her directly
I stopped the prednisone as diarrhea is a severe side affect
We had an appointment that week so when I went to that the oncologist was literally yelling at me for stopping the prednisone
I told her I had to because of the diarrhea. She said that was from the lymphoma.
Mickey was never sick
Until all these drugs were started
I should have walked out then but she
Said we had little time left and he should have chemo
We agreed thinking all these symptoms were from the lymphoma and wanted to help him
2 days after the first chemo treatment
Mickey couldn’t walk and wasn’t eating
2 days after that he went into heart failure and we had to have him put to sleep
Always follow your gut and comment sense
I’ll always regret not walking out of that office that day
Carmela
I agree. My post on Oct. 20 confirms that my dog developed all these terrible conditions due to chemo. Should have listened to my instincts and taken a chance on doing something else because in the end my dog suffered, more from the side effects of the chemo and lymphoma and the end result was the chemo stopped working and all the glands enlarged again.
I first dealt with this disease in 1986. Woke up one morning and my female dobie had a larger pouch under her chin. Took her to the vet and it turned out to be lymphoma. We started chemo immediately. The doctor warned me that although she appeared to be a perfect specimen of her breed, she was infact dying. For the next 5 months she appeared healthy. Then one night she acted lethargic. The next day, without warning she went into convulsions. Shortly after she was dead. Now 34 years later, history repeats itself with my 8 year old boxer. Back in 86′ I had a sold support base. Now I’ve outlived my family. That boxer is all I’ve got.
dear Keith so sorry to hear about your dear friend. I am looking after my lovely dog who is being treated homeopathically – it feels very touch and go but he’s still eating and enjoying a slow walk and a sniff about. i. hope it goes ok and that you’ll find a way through. there’s so many people out there – doggy and human who need you
Thank you for all of your comments. Our Buster Boy, a 7 year old mixed hound dog that we rescued as a puppy was diagnosed with lymphoma after we noticed 2 lumps under his jaw. He’s had 1 dose of Elspar (chemo) and his lumps are almost gone. We are trying to decide if we should continue with the CHOP protocol of chemotherapy. He has had no side effects from it that I’ve noticed. Maybe he is a little more tired but he’s eating well and still goes on 3 mile walks with me. He’s also taking prednisone. I’ve also started him on the Chinese herbs and my neighbor who is a holistic vet started acupuncture with him. Please help me decide if I should continue with the chemo. The total cost for 19 weeks is about $6K which I would do to have more time with my dear boy. I just don’t want him to suffer. He seems like himself right now.
Well here i sit in Fl. crying as to the decision we need to make. Our very sweet Chihuahua age 13.5 was diagnosed with lymphoma be. A tiny little grape sized lump under his neck on the right side. Immediately put on prednisone and that was two years ago. His skin has little dry scabs ever so often on it, and now is having gas been breathing episodes that follow up with a gag reflex. Put back on anabiotic’s but this Time the antibiotics are not taking affect in anyway. In hopes that maybe he had caught a cold type of cough. He eats really well loves to sunbathe, tries to sleep but the episodes are happening even while he sleeps. This is all breaking my heart. We were told back two years ago at best 4 to 6 months, I do realize we were blessed with much more time than expected. But I look in his eyes and it’s so hard to make this call. He does not seem to be in pain, but with the breathing episodes that cannot make him happy. I’m torn.
I get so emotional reading all of the above 🙁 my ridgeback was recently diagnosed with B-Cell multicentric lymphoma. Stage V high grade. The prognosis wasn’t the best, however our oncologist believes that we had a good chance to get her into remission. For a lot of people they hear “12 months survival time on average after chemotherapy” and think that’s not good news at all. But for an 11 year old dog, that’s more than 10% we can give her extra of life-time.
We are currently going through CHOP, which is classified as VCVD 1 week break VCVD and continue for 16 weeks.
I have to say, that there is nothing I love more than knowing that I have done everything in my power to make my girl not feel sick, and to stop this cancer from spreading. She is due for doxorubicin in a couple of days, and I’m very nervous, but I know how important this particular treatment is in order to achieve remission.
It’s important to know that board certified oncologists are highly trained and educated, and each dog treatment regime and dosage etc is unique and specific to your dog. We’re talking about people who have studied hard for 12 years, and have written thesis, for a very average pay. Vet oncologists LOVE DOGS TOO.
So far I have watched my dog improve, from a tired, distant and somewhat depressed girl with lymphoma, to a happy girl that I remember when I first fell in love with her 11 years ago.
Please speak with your oncologist before making any decisions about treatments, it is costly (but insurance covers this), and your dog wants to live!
I hope everyone has many more happy months and years with their companions <3
As I read each and every comment, my heart aches. My 7 year old American staffy x dogue de boardeux was diagnosed with lymphoma 8 months ago. After finishing Chemo 1 month ago, his swollen lymph nodes have returned. He still acts like his normal self, you wouldnt know he was sick. We have decided to go through with the rescue procedure as without it, we were given a few weeks with him. Crazy considering he still acts like an excited puppy.
I am absolutely devastated. He has been the only constant in my life. He has been by my side through a traumatic breakup, the unexpected death of my mother and through my depression. I dont know life without him but I know his comfort is most important. Family and friends wonder why my heart is breaking and can’t relate to what im going through and its comforting albeit incredibly sad that some of you have experienced similar things. Our pups have brought us so much unconditional joy and deserve so much more than this
Nikita,
I read every single comment above as well and feel the same- each one more aching. Your first sentence made the tears fall. Mine too got me through a horrific breakup… followed by the worst year of my life.
My heart is so broken it’s unreal. My Siberian Husky Atlas is only 4 years old. I seriously cannot wrap my head around any of this.
Atlas came into my life 3 years ago from the streets of Las Vegas…and I swear he hasn’t left my hip. Huskies have such funny personalities but Atlas clicked perfectly with my other husky- Akira. The connection I have with these dogs has been one of the most amazing things. I believe Atlas was abandon by his previous owner because of his health issues. He was born with a musculoskeletal deformity which affected both of his knees. He was very bow-legged and it was clear that he struggled to run and keep up. He also had one of his main canine teeth cracked down to the gumline- with what appeared to be an exposed tooth nerve. This PUPPY never whined or cried… it was obvious he had the energy to play like a normal one-year old…but would run for a few minutes and have to sit down because of his knees. It made me so sad, and I promised myself I would do everything to make his life better. After adoption- Atlas got his first knee replacement… followed by the second one the following year… followed by the broken tooth removal. I swear before/ during/ and after it all- he has always been the happiest little thing…as if every damn day was the best day of his life…and I finally felt he had the young healthy body to match his spirit. Or so I thought.
Atlas has been having some GI issues- very mild…aka didn’t want to eat some days, had a couple episodes of mild diarrhea. The events were far and few in between, but I knew there was something going on. I talked to a couple vets, did my research, and tried changing his food, but still these random episodes were occurring. I was recommended to try omeprazole for acid reflux- and he did great for 3-4 days…appetite/ stools were normal…. and then he had diarrhea for 2 days straight. Still throughout all this time Atlas never had any behavioral changes at all. He is SUPER energetic, plays with his sister all day every day…until 6 days ago. Atlas did not eat that morning and was super lethargic. I didn’t think much of it because it was one of the first really hot days. But when I picked up his leash he looked as though he struggled to lift his head… and even more so when he tried to get up. I took him to the ER, and after 2 hours they told me he’s “just a little dehydrated, if you want we can give him fluids,” and they sent us home. Still incredibly lethargic…I was sitting on the floor next to him when he stood up and started SCREAMING. Like the most awful, blood curling scream… he ran in a circle with his eyes bulging out of his head. Lasted 45 secs/1 min before he ran into the couch…and collapsed. I laid down next to him and he was relaxing. It was the craziest thing. Scared to move him… I let him rest for some time. But after awhile I tried to get him up and he was unable. At this point he was barely responding to me. I took him back to the ER…they still don’t know, but they decided to admit him. X-ray clear… blood work shows minor infection (elevated WBCs).
Following morning- abdominal ultrasound results show the mesenteric lymph node is swollen and composed of suspicious cells- they collect a biopsy (results won’t be back for a few days). 1 hr later I get a call that the Vet noticed free fluid surrounding his stomach… and that in fact he had a large intestinal mass (that didn’t show on the ultrasound)…that had ruptured- hence his screaming pain!! As a result, Atlas now has a septic abdomen- and is going to die if they don’t perform emergency surgery to “see what is going on.” Based on the abnormal cells seen thus far, they suspected it was cancer…and also suspected that his insides may be full of it… therefore I needed to make a pre-determined decision that in the event his organs are visibly full of cancer- if they should euthanize him on the table.
Shocked doesn’t begin to describe how I felt. Within 24 hours I went from “mild dehydration”–> “he’s will go into septic shock and die if we don’t operate…but he may be full of cancer and die anyway.” I literally could not breathe. I forced them to hold off and bring him out to me (no one is allowed inside due to COVID). He came out wagging his tail and ready to go home. I was absolutely hysterical. I made that little wolf promise me he was going to pull through surgery and make it home…and I swear on anything- he did promised me. The cut him open- removed the mass, and resectioned his intestines. The surgeon said he did not see any other visible masses, however took a biopsy of a normal piece of the intestine… as well as the swollen mesenteric lymph node. Atlas came home to me the following day…and the day after that- he was 95% back to his normal self (which is unreal considering he has 25 staples holding his gut together). But of course, the day after that… I got the call that all the biopsies were positive. He has intestinal lymphoma.
I had an apt with the oncologist the next day. 1-2 months estimated I have with him. I seriously cannot understand this. He is FOUR YEARS OLD. I’m supposed to have another TEN YEARS with him!! And he has been through enough for one lifetime! I am beside myself. I have tried to do everything right for him…and he saved me just as much as I saved him. He is Akira’s best friend. She sat and stared at the door for 2 days straight while he was in the hospital and it broke my heart.
Chemo gives me an estimated 4-6 months, which apparently is highly unlikely with intestinal lymphoma. Not to mention- it’s upwards to $10k. Regardless, nothing can be done until his stomach heals from surgery, the staples are removed, and he completes his medications. I’m trying so hard to be positive and to spend every single moment loving him, but every hour or so I have a total breakdown with this gut-wrenching pit in my stomach reminding me that this isn’t just a terrible nightmare.
Today was the first day I began accepting the diagnosis, but I still am not willing to accept the prognosis. My instinct was telling me no on chemo, and to proceed down the route of any homeopathic measures that I can…with maybe prednisone treatment. Today was his first homecooked meal on his new “cancer diet” (plus a crapload of CBD). I feel good about it- more so because he loved it. My thought is that choosing this path for him will truly give him the best quality of life…while allowing Akira and I to spend every last second enjoying his companionship.
And that is where we are today.
Hi Nicole, your story brought tears to my eyes and at the same time gave me a sense of happiness. Tears obviously for the story of Atlas, he sounds like he is an amazing guy! And happiness because I can feel/see the love you have for your furry babies. I wish more people could be like you and treat all animals with love and compassion. I truly hope Atlas will defeat this just as he did with all the other obstacles life has thrown to him. I’m currently struggling with the diagnosis the vet gave me about my sweet boy Max. He said he has a lymphoma and recommended to start Chemo ASAP 🙁
I’m not so sure if I want to put max through that. He is almost 14 years old an I’m afraid he will not be able to go through that. Vet is going to start him on steroids tomorrow so I’ll see how he responds to that and meanwhile I will continue researching other alternatives. This post was very informative and extremely helpful, specially since I saw how many other dog parents have gone through the same thing and shared their stories of their furry babies.
My thoughts and prayers to everyone that shared their stories and to the person who shared this post!
Thank you all!
Sending my condolences, thats so awful! My sweet golden retriever, Finn was diagnosed at.4 as well (he will be 4.5 next month). It’s awful! Finn was barely a year old when my daughter was born and I always imagined he’d be around for my daughter’s first ten years. I have cried every single day since I suspected the diagnoses a month ago. I can’t believe one day soon I’m going to have to tell my 3 year old her dog is gone. My heart is so broken.
We have a 3 year old chocolate sprocker (cocker / springer spaniel cross). Lives in the country – happy and full of energy. He has been diagnosed 2 weeks ago and has enlarged lumps under his jaw and one on his back leg. We have decided not to go for chemo as he gets very stressed in the vets (wee’s himself) and would need sedating for each treatment. He’s on Prednisone, but I can see one lump has grown again today. Do the lumps change size or continue to grow? I am devastated as he is so young and I haven’t really got over the death of my other dogs 2 and 3 years previous but at least that was old age. I can’t believe how quickly they can deteriorate.
Just wanted to share this in hopes of any advice or words of encouragement. I have a 3yr old male dog small mix that was just diagnosed with lymphoma cancer. Last Saturday I noticed a huge lump on the left side of his neck, Sunday 2 more on the other side popped up, his face was now swollen he wasn’t eating or drinking and had no energy, Tuesday he saw the vet they did blood work and a biopsy. Because of his lab work alone, the vet said that there was a real possibility that it could be cancer. His WBC was off the charts, the highest he’s ever seen in an animal 225.19 K/uL and a temp. of 103.0. Needless to say the biopsy came back positive. He told me treatment options would be chemo depending on what stage it was in or steroids to keep him comfortable for whatever time he has left. I asked the vet if it was him what would he do and he said that chemo can be hard on dogs and that the cancer has more than likely already spread and that steroids can help him feel a lot better and possibly slow down the cancer a little maybe given us a month or so before it would be time to let him go. I have him in antibiotics and steroids and what a difference it has made. This can feel very deceiving at times because even though he’s acting like he feels better the cancer is still growing and taking over his poor little body. If anyone could tell me what I should prepare for and what other symptoms will come and how quickly will they come. I’m trying to mentally and physically prepare myself and my family for this unfortunate journey we have to take and make the most out of it for my puppy. Any input or advice would be appreciated.
I have a 6 year old boxer names Daisy. She was just diagnosed with Lymphoma cancer. As many of you mentioned, she is eating well and full of energy. Its hard to take in all that bad news when they seem so full of life. I am trying the CNNU Chemo option plus looking into holistic options to combine. I don’t have that kind of money but I will take out a loan, my family will help a bit. I am lost I am hanging on to hope and prayers. I cant give up on her, she is family and I cant give up and must give her my all. Boxers all so loyal, loving, kind, and Daisy loves to great all my guest. I cry everyday since we found out. My kids and I sat in the car as the Vet game us the bad news. And to add to it all she could not start CHEMO yesterday because she has a low WBC. As many mention its hard to accept when they seem so happy, it brakes your heart. I pray to God to please guide us and heal her. She is on a home cooked meal diet, CBD, and Gold pet supplements, they seem to help. I hope next week we get better news about her starting CHEMO and she has an appt with a holistic vet….prayers to everyone in this hard journey. This will be a sad Christmas…”Trust in the Lord with all your Heart!!!!!!” I keep repeating.
Hi, my dog was diagnosed with lymphoma cancer on September 26th of this year. She was put on prednisone and was doing great. Her lymph nodes decreased significantly. A week and a half ago I noticed that they got bigger and I got more worried because you could hear the struggle to breathe in her breath. She’s only three years old. And I’m not ready to lose her. Lately she has been not wanting to move as much. And I’ve noticed from the way she sits down, it looks like it hurts her. The lymph nodes are pretty big and it doesn’t seem like the medicine is helping much. This morning I practically had to drag her out of my room to go outside because she wouldn’t get up. I’m worried about her and the cancer. I don’t want to lose her but I don’t want to put her through any more pain just because I’m afraid to let her go. If anyone has had an experience like this with their dog and has any advice, I would extremely appreciate it.
My sweet golden retriever Finn was diagnosed with lymphoma at only 4 years old. Finn received his annual checkup + vaccinations near the end of December. We were told his fecal test revealed he had worms and we were given Drontol Plus which we started right away. Within a week I noticed he was very thirsty. I thought he was trying to flush the worms out although it wasn’t a side effect of the pills. He seemed back to normal the next week but then I noticed he wasn’t eating as much. I figured since it was a week after starting medication it must be related. He was still eating treats and whatever the kids leave out for him to steal, just not his kibble which he has always been slow to eat. A day or two later, we decided to give Finn a bath. I usually take him to a groomer but due to the COVID pandemic, groomers have been closed and it had been a number of months since he was groomed and he was looking quite dirty from rolling around outside, so my husband and I bathed him ourselves. When i was brushing him I felt the enlarged lymph nodes. I had already planned to take Finn to the vet on the weekend if he didn’t start eating more, but as soon as I felt those lymph nodes, I googled, freaked out, and booked him to be seen that day.
I hoped he had a virus causing the enlarged lymph nodes.. maybe the worms/parasite he had wasn’t eliminated with the dewormer medicine and that’s what was causing his symptoms.. but I had this horrible feeling in the pit of my stomach that it was cancer. He had all the symptoms I read about. I had what felt like the longest week of my life waiting for Finn’s biopsy results.. Sure enough, the lymphoma was confirmed. We must have caught it pretty early since he appeared to be in perfect health at his checkup. Part of me wonders if the vaccines or dewormer caused this since he got ill a week later but I found little research on the topic. Regardless, when not faced with a pandemic, Finn is a social dog so he needs to be vaccinated, and we wouldn’t want him to have worms either, so I don’t think we could have done anything differently.
I asked for a copy of Finn’s biopsy report and it did not indicate what type of lymphoma Finn has (B or T) or his staging. It implied he would need further testing for that which my vet did not mention. Maybe it does not matter the specifics since we made the very difficult decision not to do chemotherapy.
I hate to say it but we made the decision not to do chemo primarily due to the financial strain it would cause our family. I have told myself I don’t want to “put him through” chemo. I want to give him the best quality life for what he has left. However, I have read that dogs respond well to chemo (as in they do not lose their hair or have side effects as bad as humans). So I think I am just telling myself I have Finn’s best interests so I don’t feel guilty about not doing the chemo.
Selfishly, although I want Finn around as long as possible, I know there is no cure and it’s borrowed time. I think doing chemo to prolong’s Finn’s life would be too painful for ME. I have cried every day since his diagnosis. Not knowing how long he has is killing me. I am obsessing over every move he makes, wondering if it’s a sign.. wondering if he’s trying to tell me he’s ready to go.. so I know if he were on chemo, it would prolong my worrying.. We just lost my grandma who was my best friend to cancer a year ago and although Im grateful she did chemo to get more time with us, it was just absolutely awful.. the waiting for scans to see if the tumour had grown etc.
My 3 year old daughter who was born about a year after Finn is growing more and more attached to him (my 9 month old son loves Finn as well, but at 9 months, he has a different level of understanding). My daughter will be confused where her dog has gone. I so badly dread telling her what has happened when Finn goes. My heart breaks thinking about it! But the selfish part of me feels it will be easier on her emotionally if we say goodbye sooner. Also, my fear is the chemo will not work, what if we pay several thousands of dollars and still only get a month or two left. We barely have enough to cover our mortgage and bills as is. The idea of losing Finn and paying off the vet bills for years and years after he’s gone is stressful. If chemo would cure him it would be a different story.
Finn is currently responding well to prednisone. He went from having zero appetite right before his diagnosis to being hungry all the time after starting his medicines. Finn now finishes all of his meals plus many many treats. He is napping more than normal, but when he’s awake, he’s very hyper and energetic, and if it weren’t for the medication we give him, I would forget he’s sick. I am thankful for everyday with my golden boy. As awful as this is, I am grateful we caught this early and can cherish our time with Finn.
My daughters beautiful 5 year staff X was diagnosed last week with Lymphoma after we noticed the swelling under his chin. He appeared a healthy happy active dog leading up to this. We have pet insurance so opted for the Chemo and the steroids. Week 2 and he appears happy, healthy enjoying his walks and his appetite is still normal. The only side affect is runny stools atm. We will be getting some Liquid Gold and the Mushrooms and I am making bone broths and cooking his meat now so fingers crossed.
Hello, We have a beautiful 10 yo border collie, Zorro, who was diagnosed with lymphoma over 4 months ago. Our wonderful vet told us that there was no cure, and if she were in our position she wouldn’t put her own dog through chemo. She predicted he had 4-6 weeks left before we would need to call her to euthanise him. We were, and still are, shattered, but we are also very grateful for her advice as he has exceeded her predictions and has had 4 very happy months since diagnosis. We know he is dying but he is still enthusiastic about his walks and has a very good appetite. His breathing is often laboured and his submandibular nodes are now very swollen. We won’t let him suffer and will call our vet when we notice that his life is too much of a struggle. We have lost several beloved dogs to old age in the past but this is different. Too cruel, too early. Your stories all tell of similar heartbreak and my heart goes out to you all.
How soon after noticing 1 or 2 enlarged lymph nodes in your dog, did other symtoms start happening, was it days, weeks, etc., I would appreciate any information in regard to that progression. Thanks
I just wanted to say that I really appreciate this article. My GSD was diagnosed with lymphoma at the end of July and the only feasible option I had for treatment was prednisone. Most of the articles that I read are very biased about pushing for CHOP and other expensive treatments and usually end there. I appreciate that this article lacked those biases and objectively explained the prognoses of the available treatment options without making me feel bad for the choice I had to make for my dog. She is just the most wonderful creature and I so wish I could’ve done better for her, but felt very conflicted due to my financial situation in the wake of the pandemic and other stories that I have heard about not all dogs responding as well as others to chemotherapy. So far she has made it a month and 2 weeks on prednisone, but she is winding down quickly. I estimate that she’s hit stage 4 or the beginnings of stage 5 based off of her behaviors/symptoms. She is lethargic and doesn’t want to play as much, but still tries to bring me her frisbee. It breaks my heart. For anyone else going through this, I wanted to share some of her symptoms and their progression because I know it can be difficult to find other firsthand accounts on the internet. For the first two months of diagnosis, she was completely fine and normal. We were able to put her on prednisone after approximately 24 days of knowing her diagnosis due to delays getting into the oncologist. She barely showed any side effects with prednisone for the first month, only drinking moderately more water with slightly increased frequency of ruination. Only the lymph nodes near her jaw were swollen for the first month and two weeks, but not long after we started prednisone, I noticed swelling of the ones under her belly had started as well. I noticed she was getting more tired about 2 weeks ago. She loves to run and play with her frisbee, but started to only trot with her frisbee, which was completely abnormal for her. About a week ago, she peed in the house, which is something she has never done in the 2 and a half years I have had her for. The frequency at which she was drinking water and urinating increased dramatically. She now cannot hold it much more than 2-3.5 hours without an accident. 4 days ago, the lymphedema kicked in and her left hind leg swelled up to 1.5-2x its normal size. She’s had blood in her feces sporadically since then. We started doing the wraps on her legs, which help for awhile but it doesn’t last. Her breathing is slightly labored as well. However, her appetite is still great and she even wants to eat more than usual. We’ve had regular check ins with our vet and unfortunately he is not as familiar with canine lymphoma, but he is doing everything he can for her. She is on lasix for the edema, but the results are not very strong. She has also experienced some bloating with frequent gas. I don’t think we have much longer with her so I have just been trying to prepare for the worst. The swelling of her lymphs fluctuates a lot. I hope this was helpful to anyone who reads it. So sorry to anyone who is also going through this, it is just terrible. My girl is my best friend in the world and I have just been absolutely beside myself.
Ruination should be ** urination! Whoops!
Thank you for sharing and helping others in this situation. Sorry for you going through this.
My heart goes out to you all. I have now lost three dogs to cancer, liver failure and tumor. My beautiful rescue foxy who is a staffyx is about to also embark on the fight of her life also, lymphoma.
All I can say to you all is, if you are using chemicals like roundup, insecticides, lawn weed killer and feeder, please stop.
it’s proven to be the number one cause of cancer in animals and people. We need to all remember we have shoes to protect our feet, our furbabies do not, all chemicals on the ground will get absorbed into their blood stream, airborne chemicals we our lungs breath in just as theirs do. It may just pay us to make doggie shoes for our friends.
It’s unfortunate the doggy parks we let them run free on are not green just because they water them, it’s the chemicals. Dogs and cats eat grass!
And no I do not use any of these chemicals, I use my hands to pull the weeds out. I did a shit load of research over the last ten years and found most farmers die of cancer as did my mum because of the chemicals they use. To give you an example a tomato is sprayed 13 times with a casagenic before it reaches your mouth. A so called organic tomatoes is still sprayed five times as are every other vegetable.
I just wanted to make you all aware as the chemical companies certainly will not, after all their goal is only to make money.
Regards,
Tammara
I’m a living proof that you can be cured from Non-Hodgkin Lymphoma. Lymphomas are blood cancers” in the lymph nodes. They develop more frequently in older adults and in compromised individuals. After years of living with Non-Hodgkin Lymphoma. I was cured naturally with the use of World Rehabilitate Clinic herbal formula, with a period of (3) three weeks I was recovering. In 2019 I begin using World Rehabilitate Clinic herbal formula specializes in internal and pulmonary medicine.
Our Weimaraner boy was diagonosed with T Cell lymphoma when he was 3 Yrs and 10 months old. Also had hypercalcemia and that was the reason we even noticed something was wrong, because he developed increased urination. Lab results took 1 week and after that he went straight to chemo. We also used CBD and CBG oil drops, arthemisinin and all of the above mentioned mushrooms (turkey tail, reishi etc.) Sadly it wasn’t enough and after 5 months his health declined so musch we had no choice than to say goodbye 2 weeks ago. The pain is horrible. My heart goes to all of you who are fighting lymphoma with your phurry family members, because I know how hurtfull it is. Even if the fight is eventualy going to be lost, your pets will be thankfull, that you fought it with them.