You probably know someone with an underactive thyroid gland; in fact, you may have one yourself. The signs of hypothyroidism in humans include a subnormal body temperature, cold hands and feet, weight gain, hair loss, and constant fatigue. People aren’t the only ones afflicted by this disorder, for many dogs are hypothyroid, too. They may seem lethargic, gain weight while eating normal or below-normal amounts of food, seek warmth, and develop skin and coat conditions. But hypothyroidism causes other symptoms, too, and an accurate diagnosis can require thinking outside the box.
Consider Logan, a highly trained search and rescue dog who, at age three, became so fearful that he could no longer work and was going to be retired. Brodie, an agility dog, had normal thyroid test results but was slow in competition and had constant ear infections. Brewser, an Alaskan Malamute, became aggressive and lost his appetite. Ruq, a Eurasier at a perfect weight, became short-tempered, lethargic, and developed entropion, a condition in which her eyelids rolled inward, requiring surgery to correct.

The veterinarians who treated these dogs insisted they could not be hypothyroid because their test results were “normal,” they were not overweight, or they had beautiful coats. But the vets were mistaken; treating their underactive thyroids returned these dogs to health.
Metabolic Hormones
The butterfly-shaped thyroid gland, which resides in the throat on either side of the trachea, manufactures and stores hormones that control the body’s metabolism. When the thyroid is too active or not active enough, a variety of health problems result. In humans and dogs, hypothyroidism is the most common endocrine disorder; cats and a smaller percentage of humans are prone to hyperthyroidism, an overactive thyroid gland. Hyperthyroidism in dogs is rare unless too much thyroid supplement is given, but can be linked to thyroid cancer or cystic nodules.
The thyroid produces two forms of thyroid hormone: T3 (triiodothyronine), which is the active form, and T4 (thyroxine), the inactive form. When T4 is absorbed into tissues, it is converted into T3, but most of the circulating (total) T4 is not available for absorption. The part that is available is called free T4. In dogs, about half of the body’s T3 comes from the thyroid gland and about half is converted from T4 by other tissues.

The production of T4 is regulated by the pituitary, a tiny pea-sized gland at the base of the skull. The pituitary is known as the “master gland” because it controls so many hormone functions. Among other things, it produces thyroid stimulating hormone, or TSH, which causes the thyroid gland to release T4.
Every cell in the body responds to thyroid hormones, and low levels can affect multiple body systems. Nearly all canine cases of hypothyroidism are primary, which means they are caused by damage to the thyroid gland, usually by inflammation, degeneration, or a tumor.
Hypothyroid Signs
Because hypothyroidism affects many body systems, clinical signs are variable, non-specific, and often slow to develop. The most classic signs (significant weight gain, lethargy, and cold intolerance) do not appear until more than 70 percent of the thyroid gland is destroyed. Other symptoms may appear earlier, such as behavior changes (lack of focus, aggression, passivity, or fearfulness), minor weight gain despite caloric restriction, and apparent food allergies or intolerances.
As many as 88 percent of hypothyroid dogs suffer from chronic skin disorders, including dry, scaly, or greasy skin (seborrhea); thin or coarse, dry coat; excessive hair loss; and offensive skin odor. Additional effects of hypothyroidism can include bradycardia (slow heart rate), constipation, diarrhea, chronic skin and ear infections, corneal dystrophy or ulceration, and female infertility.
One classical finding in hypothyroid dogs is a thickening of tissue, especially in the face and head. The thickened skin produces folds and what is referred to as a “tragic face.” This thickening can occur in other tissues as well, such as facial nerves, causing neurological disorders.

Autoimmune thyroiditis may occur in conjunction with other autoimmune disorders. While the following are not considered symptoms of hypothyroidism, there may be connections between hypothyroidism and megaesophagus, laryngeal paralysis, Addison’s disease, ear infections, ruptured cruciate ligament, pancreatitis, vitiligo (pigment loss), unprovoked aggression, and the sudden onset of seizure disorders.
As many as 77 percent of dogs with seizures may be hypothyroid, although the link between these conditions is unclear. One study showed a significant relationship between thyroid dysfunction and seizures as well as between thyroid dysfunction and dog-to-human aggression. Treatment follow-up in 95 of these cases showed a significant behavioral improvement in 61 percent of the dogs.
Potential Causes
The leading cause of hypothyroidism in dogs is damage caused by the body’s own immune system. W. Jean Dodds, DVM, author of The Canine Thyroid Epidemic: Answers You Need for Your Dog, specializes in canine thyroid problems. Dr. Dodds estimates that more than 80 percent of canine hypothyroid patients have an inherited autoimmune disorder resulting in a condition similar to Hashimoto’s thyroiditis in humans. Lymphocytic thyroiditis, which is common in dogs, is an inflammation of the thyroid gland caused by the immune system attacking the gland by mistake.
Most of the remaining cases are caused by idiopathic follicular atrophy: degeneration of the thyroid gland without evidence of inflammation (idiopathic means that its cause is unknown), and may be the end result of immune-mediated destruction.
Dr. Dodds blames poor breeding practices, frequent vaccinations, immune-suppressing medications, nutrient-deficient diets, and exposure to environmental toxins for today’s epidemic of canine hypothyroidism.
Because the thyroid needs iodine in order to function, an iodine deficiency may contribute to hypothyroidism. However, most commercial dog foods contain adequate levels of iodine, so this is unlikely to occur unless the dog is fed a home-prepared diet lacking in iodine. Excess iodine from oversupplementation can also suppress thyroid function and even contribute to autoimmune thyroiditis. Do not add kelp to a commercial diet that already contains iodine. According to Dr. Dodds, excessive iodine resulting from adding kelp to commercial food while a dog is pregnant or nursing can destroy the thyroid glands of fetal or newborn pups.
Although rare, some dogs are born with congenital defects that prevent the production of thyroid hormones. This condition has been seen in Giant Schnauzers and Boxers.
Thyroid tumors are another uncommon cause of hypothyroidism, but unless a tumor affects both lobes of the thyroid and the gland is completely destroyed, hormone output usually remains normal.
Secondary hypothyroidism develops when some other influence causes the thyroid gland to produce insufficient thyroxine, such as when a brain disease interferes with the regulation of thyroid gland activity, or when the gland is destroyed by radiation therapy, surgical removal, or the administration of medications that affect thyroid gland activity.
Diagnosis
To diagnose hypothyroidism, veterinarians rely on several thyroid function tests, including total T4, free T4, total T3, free T3, TSH, and tests for autoantibodies T4AA, T3AA, and TgAA, which indicate autoimmune thyroiditis.
Thyroglobulin (or Tg) autoantibodies will be high in about 92 percent of cases where T3 or T4 autoantibodies are present, so tests for TgAA can be used in their place and to monitor response to treatment. About 20 percent of dogs with thyroglobulin autoantibodies but no signs of hypothyroidism will progress to overt signs within one year. Rabies vaccination within 45 days of the test can cause falsely elevated results; giving thyroid supplementation up to 90 days before the test will decrease the result.

The TSH test, which is commonly used to diagnose human hypothyroidism, is not reliable in dogs. High TSH combined with low free T4 helps to confirm the diagnosis, but normal or low TSH does not rule it out. The total T4 screening test also cannot be used to rule out hypothyroidism, as the presence of autoantibodies can falsely increase the result. The most accurate test is the Free T4 by Equilibrium Dialysis, although even that by itself gives an incomplete picture.
T3 results are not reliable for diagnosing hypothyroidism. T3 levels are typically normal in hypothyroid dogs. High levels can be caused by T3 autoantibodies; low levels are often linked to non-thyroidal illness (NTI).
Normal T4 test results can vary by age, size, and breed – normal levels are lower in older dogs, large dogs, and especially sighthounds – and unrelated illnesses can reduce thyroid levels, as can treatment with seizure medications, corticosteroids, non-steroidal anti-inflammatory drugs, beta blockers, drugs used to treat separation anxiety, and some antibiotics. Because circulating blood levels of thyroid hormones may not reflect the cellular and tissue levels of these hormones, dogs with normal test results but with clinical signs may benefit from thyroid supplementation.
At the same time, an accurate diagnosis is important because treating a dog for hypothyroidism that doesn’t exist creates new problems.
Sick Euthyroid Syndrome (SES) is often misdiagnosed as hypothyroidism. In SES, dogs with normally functioning thyroid glands (euthyroid) have decreased thyroid hormone levels because of trauma, stress, injury, or poor diet, any of which can affect hormone levels. The thyroid responds to stress, illness, or injury by reducing thyroid hormone secretion, thus slowing the body’s metabolic rate and conserving energy. Because the underlying cause of SES may be difficult to identify, this protective mechanism can be mistaken for hypothyroidism. Examples of non-thyroidal illnesses that can lower thyroid levels include Cushing’s disease, diabetes mellitus, chronic renal failure, liver disease, and Addison’s disease. When these diseases are treated, the apparent hypothyroid problem corrects itself.
Other test results may help confirm the diagnosis. Over 75 percent of dogs with end-stage hypothyroidism have high cholesterol levels in blood drawn after a 12-hour fast, though this may not be seen in early stages of the disease. Approximately 40 percent are anemic. Liver enzymes (likely due to altered fat metabolism) or creatine kinase (CK) are sometimes elevated. Because other factors can affect these test results, they support a diagnosis of hypothyroidism without being definitive on their own.

Even the weather can affect results, for a ride to the vet on a hot summer day may temporarily decrease total T4 levels, causing false low-thyroid results.
When diagnosis is in doubt, blood can be sent to Dr. Dodds’ Hemolife Laboratory, a division of Hemopet. Dr. Dodds will also review test results from other labs with dog owners and veterinarians. She keeps track of normal test result ranges for different breeds and situations, which can help determine whether a low-normal test result might indicate hypothyroidism.
A therapeutic trial for at least six weeks can also be used when there is a question about diagnosis, although improvements may be seen in dogs with SES who are not truly hypothyroid.
Treatment
Hypothyroid dogs respond quickly to thyroxine (T4) treatment, with improvements in attitude, mood, mental alertness, energy, activity levels, appetite, and aggressive behavior during the first week or two. Skin and coat problems usually improve within four to six weeks, while hair regrowth may take four months or longer. In most cases thyroid medication is needed for life.
Medication can be given either with or without food but should always be given the same way because food interferes with absorption and thyroxine binds to soy and calcium. Many veterinarians recommend giving thyroid medication at least an hour before or three hours after meals. If symptoms do not resolve or T4 levels remain low when supplements are given with meals, they should be given separately to ensure adequate absorption.
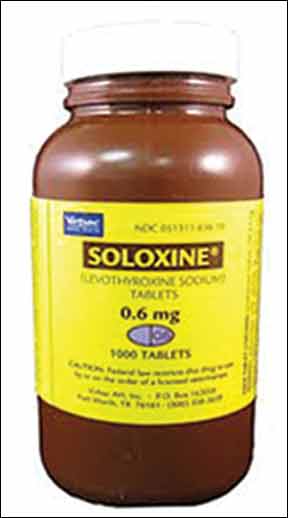
Soloxine (levothyroxine sodium) is the most commonly prescribed medication for dogs with hypothyroidism. (Synthroid is the same drug’s human formulation.) Because thyroid supplementation increases the metabolic rate, dogs with significant heart disease or hypertension (high blood pressure) should be treated with caution.
The typical thyroxine starting dose is 0.1 mg per 10 pounds of ideal body weight every 12 hours (twice daily dosing works best due to the medication’s short half life in dogs). Smaller dogs require higher doses for their size, while sighthounds should be given less. In complicated cases, where the patient also has diabetes or an illness affecting the liver, kidneys, or heart, treatment should begin more slowly, at 25 percent of the standard beginning dose, and gradually increase over three months.
Veterinarians report differences in how dogs respond to generic and brand-name drugs; many warn against using generics because of differences in absorption and bioavailability. Fortunately, brand-name thyroid drugs are inexpensive, just a few dollars a month, so there is little economic advantage to using generics. Once a dog is stabilized on a particular thyroid medication, it’s better to keep the dog on that product rather than switch from one brand to another.
Follow-up T4 testing ensures that the dosage is correct. The timing of the test is important, as T4 levels will be lowest just before the pill is given and highest four to six hours after. This testing is usually done four to eight weeks after therapy begins. TSH levels can also be checked, for high TSH indicates that the dosage is too low. (Normal or low TSH levels are not meaningful.)

Signs of a too-high dosage can include increased thirst, drinking, and urination; weight loss; diarrhea; panting; nervousness or anxiety; restlessness; pacing; hyperactivity; and an elevated heart rate.
After the initial dosage is confirmed, annual monitoring is recommended unless the dog develops new symptoms in the interim. If a dog has been on thyroid supplementation for some time and there is any question about the diagnosis, treatment must be discontinued for at least two months before test results will be valid. There is no apparent harm in abruptly stopping thyroid supplementation. If possible, medications known to interfere with thyroid levels should be discontinued.
Complementary Therapies
While thyroxine is safe when taken as directed, some caregivers prefer to avoid synthetic drugs and would rather use natural products whenever possible. Natural thyroid extracts made from bovine or porcine thyroid glands are used in human medicine (Armour Thyroid, Westhroid, Nature-Throid, and the Canadian product ERFA are all good choices), but because these products contain both T4 and T3 thyroid hormones, their dosages require adjustment.
Natural thyroid dosages are measured in grains (60 mg = 1 grain), and 1 grain natural thyroid extract equals 74 mcg (0.074 mg) synthetic thyroxine. Thus, 0.1 mg thyroxine equals about 1.5 grains natural thyroid, 0.2 mg thyroxine equals approximately 3 grains, and 0.3 mg thyroxine equals about 4 grains natural thyroid.
Dessicated thyroid extracts cost more than synthetics and larger amounts may be needed. Because they contain T3 as well as T4, they can help the few dogs who are unable to convert T4 to T3.
There are also non-prescription thyroid support supplements that contain thyroid glandular material from which thyroid hormones have been removed. Although these products cannot replace thyroid hormone medication in true cases of canine hypothyroidism, says Dr. Dodds, they have been used successfully to lower the prescribed dose, and may also help dogs with declining thyroid function who are not yet fully hypothyroid.
Dr. Dodds recommends Standard Process Thytrophin PMG and Standard Process Canine Thyroid Support. Other products that include glandular material among other ingredients include Metabolic Advantage Thyroid Formula, Thyroid Glandular, Bovine Thyroid Health, and Thyrosine Complex (see Resources list on page 19).
Nutrition is a key factor in treating hypothyroidism, and a high-quality diet is crucial. The most important mineral for thyroid health is iodine, which should be present in optimal amounts.
The National Research Council (NRC) recommends about 100 mcg iodine daily for a dog weighing 10 pounds, 300 mcg for a 50-pound dog, and 500 mcg for a 100-pound dog. Iodized salt contains about 105 mcg iodine per 1/4 teaspoon. (Unrefined sea salt contains trace amounts but is not a significant source of iodine.) Yogurt, eggs, and fish contain iodine, but the most important food source of this essential mineral is seaweed.
The famous herbalist Juliette de Bairacli Levy considered kelp an essential supplement for dogs and other animals. “I introduced seaweed to the veterinary world when a student in the early 1930s,” she wrote. “It was scorned then, but now it is very popular worldwide.” She credited kelp and other sea vegetables with giving dark pigment to eyes, noses, and nails, stimulating hair growth, and developing strong bones.
When adding kelp or other seaweeds to a home-prepared diet, be sure to consider their source, for plants grown in polluted waters can be contaminated by heavy metals. In 2007, researchers at the University of California/Davis found that eight out of nine kelp supplements tested contained abnormal levels of arsenic. Look for organic certification on labels and check with manufacturers regarding their testing for heavy metals and other contaminants.
Because the iodine content of kelp and other sea vegetables varies widely, there is no single dose that provides the NRC’s daily recommendation for dogs fed a home-prepared diet. If the label doesn’t provide a seaweed product’s iodine content, contact the manufacturer for that information.

Note that raw cruciferous vegetables (members of the cabbage family) can suppress thyroid function if fed in quantity. These include broccoli, Brussels sprouts, cauliflower, cabbage, kale, collard greens, and more. Another ingredient to avoid is soy, which contains isoflavones that can block the activity of thyroid peroxidase (TPO), the enzyme that helps convert T4 to T3.
A selenium deficiency can slow the conversion of T4 to T3, a problem unlikely to occur in dogs on commercial pet food but possible with home-prepared diets. Ocean fish, turkey, chicken, and beef are all significant sources of selenium, but the mineral’s wonder food is the Brazil nut. The NRC recommends 37 mcg selenium daily for 10-pound dogs and up to 207 mcg daily for dogs weighing 100 pounds. Brazil nuts contain 70 to 90 mcg selenium each, so a single Brazil nut given every few days to a small dog or every day to a large dog can be inexpensive insurance for dogs fed a home-prepared diet that might be low in selenium. Like most minerals, too much selenium can be dangerous, so don’t oversupplement.
Because adrenal exhaustion or fatigue can impair thyroid production, adrenal support supplementation may result in a marked improvement.
Diagnosing Outside the Box
It would be wonderful if every hypo-thyroid dog presented the same obvious symptoms and veterinarians never missed a diagnosis. But hypothyroid dogs come in all shapes, sizes, and conditions, and you can’t always tell just by looking. Here are seven dogs who demonstrate the wide variety of symptoms that an underactive thyroid can cause.
-Logan: Too Scared to Work
Logan is an IPWDA-certified Trailing K9 (search and rescue dog) active with ATT Search and Rescue Dogs of Virginia. A 7-year-old Golden Retriever/Malinois-mix, he lives with Joanne Kuchinski and Barry Wood in Danville, Virginia.
“After three years of training,” Kuchinski says, “Logan went from being a working fool to being afraid to get out of the car. He would sit and shake. He was scared of everything.”
She was about to retire Logan from search and rescue work when she had his thyroid tested. The result was very low normal. “The veterinarian brushed me off,” she says, “but from my research I knew that low normal might be the issue. I went to another vet who listened to my concerns and put Logan on thyroid medication. Two weeks later Logan attended a seminar and was almost back to his old self. He worked in a crowded parking lot (the same one he sat and shook in) like a champ.
“That was in February of last year,” she continues. “In May he took his International Police Working Dog Association trailing test during a thunder storm and passed it. The instructor, who saw him before and after his thyroid treatment, could not believe it was the same dog. Before his treatment we went to the beach because Logan loves water, but all he did was hide under a picnic table. The following year we went back to the same beach and he ran in the surf, chased a ball in the waves, and enjoyed himself racing all around.”

-Brodie: Slow Agility Dog?
Brodie, a Labrador Retriever, has a long string of titles after his registered name (Weymouth’s Scottish Brodie, AXP, OJP, NFP, NAC, NCC, CTL3-R, CTL4-F, CTL3-H, CGC), most from agility, the sport in which he’s competed for eight years.
Despite all his titles, says Laura Williams of Old Bridge, New Jersey, Brodie was always slow, and he weighed more than she liked. “In addition,” she says, “he always seemed to have dirty ears no matter how much I cleaned them, and his toenails grew so slowly, they never seemed to need clipping.”
Brodie’s blood test results were evaluated by Dr. Jean Dodds, who determined that as a performance dog, his thyroid levels were too low. “After being put on Soloxine,” says Williams, “his coat improved to the point where friends noticed and commented, his nails needed clipping on a regular basis, his ears improved, and his weight came down from 77 to 65 pounds. I attribute all of these changes to getting his thyroid regulated. Also, his energy level improved, which carried over into the agility ring.”
Brodie turns 11 on August 5 and he currently competes at the Excellent level in AKC Agility. “I hope to keep running him as long as possible,” says Williams. “I think it helps keep him healthy.”
-Diagnosing Ruq
Ruq (which rhymes with duke and is short for Amaruq, an Inuit word for wolf) is a Eurasier living with Pam Richard in Portsmouth, New Hampshire.
“When we realized something was wrong with her,” says Richard, “we had a terrible time getting a diagnosis. Ruq’s problems included a very delicate digestive system with frequent diarrhea, plus hair loss and lethargy. She went from being a social, playful dog to being short-tempered and uninterested in play.
“The vet we were seeing did not recommend thyroid testing. I eventually took Ruq to a holistic vet and asked about her thyroid based on research I had done. Her blood was sent to Dr. Dodds, and in November 2008 she was diagnosed with hypothyroidism. We began giving her 0.4 mg of Soloxine twice a day.”
One reason it took so long for Ruq to be diagnosed was that she was never overweight. She was her heaviest at 57 pounds, only two pounds more than her optimum 55 pounds. “I think the fact that she eats a home-prepared diet may have helped keep her weight under control despite the thyroid problem,” says Richard, “but that was a disadvantage when we were looking for answers.”
By 2008, when she was finally diagnosed, Ruq had developed the symptom known as “tragic face,” and she eventually had surgery for entropion, which Richard thinks may have been a result of the change in her facial muscle structure caused by hypothyroidism.
Thanks to her medication, Ruq is once again a playful, amusing dog. She no longer suffers from chronic indigestion or diarrhea, and despite being almost eight, she acts like a puppy. “I am so happy to have my girl back!” exclaims Richard. “I have used Ruq’s story to urge people to screen their dogs for hypothyroidism, as it is so much better to receive an early diagnosis.”
-Brewser: Atypical Signs
In 2007, Brewser, a 3-year-old Alaskan Malamute belonging to Lisa Jones of Uxbridge, Massachusetts, was a sociable, happy dog who played well with other dogs and people, worked as a therapy dog, and earned titles in Rally. He was working on his AKC Companion Dog (CD) title when, according to Jones, he suddenly became dog-aggressive. “He never hurt another dog, not even in day care where they were all loose together, but he growled and snarled at them,” says Jones. “This took him out of competition. The group ‘stay,’ which had been his most solid exercise, was now impossible.”
Brewser’s veterinarian believed the changes stemmed from his breed, age, and a learned behavior from day care.
Jones removed Brewser from day care and began a painstaking process of rehabilitation by slowly building his tolerance for other dogs. She tried clicker training, but he wouldn’t eat treats, so she found other ways to reward him. Brewser’s behavior improved, and he even enjoyed the new puppy Jones got in 2009, but his appetite waned and he began to lose weight. A year later, Brewser lost interest in obedience training. His energy was low, he didn’t learn new things as quickly as he used to, and his stamina disappeared. But whenever Jones asked their veterinarian about Brewser’s thyroid, she was told that his coat was too nice for him to have thyroid issues.
In July 2011 Brewser developed a corneal ulcer. Jones took him to an ophthalmologist at Tufts University in Massachusetts. “It was a routine injury,” she says, “but I was stunned that in the few weeks since his last vet visit he had gained four pounds despite continuing to turn his nose up at food.” A week after Brewser healed, he developed a corneal ulcer in the other eye and more weight gain. “I asked the ophthalmologist if this could be the result of a disease and he said his eye looked healthy. I asked about thyroid and was once again told that his coat was too nice.”
Two weeks later Jones took Brewser to a holistic veterinarian, and his life turned around. “She said she didn’t care what his coat looked like,” says Jones. “Eye changes and appetite changes can absolutely be related to the thyroid. She drew some blood and he tested low, so low that Dr. Dodds, whom we consulted, started her comments with the word ‘Wow!’”
Brewser began taking Soloxine. Within 10 days, his leash aggression waned, his appetite returned, and he lost weight. In hindsight, Jones describes his symptoms as similar to depression. He had decreased mental alertness, difficulty concentrating, less playful behavior, was easily fatigued, suffered from sore joints, lost interest in activities he previously enjoyed, became overly sensitive to stress, displayed erratic behavior and moodiness, was fearful and anxious, lost his appetite, and experienced weight changes. In 18 months his weight went from 83 to 74 to 91 pounds.
“He is maintaining a healthy weight of 82 pounds,” says Jones, “and I no longer have to bait his food with special treats or hand-feed him. He takes treats in training and enjoys working again. He does not want to complete, most likely because I get nervous and he is sensitive to me, but we train for fun. At seven years of age, he is more like the boy I knew from birth to age three.”
-Reese: What Does Cancer Have to do With It?
Reese, an 8-year-old Dachshund living with Angel Seibert in Virginia Beach, Virginia, was diagnosed with throat cancer in 2009 when she was five years old.
Reese’s veterinarian removed the tumor but left “dirty margins” in the throat area, so Reese was treated with radiation at North Carolina State Veterinary Hospital, a procedure that destroyed her thyroid gland. “No one mentioned it to me at the time,” says Seibert. “I was just happy that the cancer was gone. She gained a lot of weight and never acted as though she felt very good. I just thought she was getting old and that the radiation treatment took a toll on her.”
Reese eventually grew seriously ill. “When the vet ran tests,” says Seibert, “everything came back crazy. Her liver levels were very elevated and her pancreas was abnormal. My vet was stumped but asked if anyone had mentioned that her thyroid might be damaged by the radiation. They hadn’t, but we immediately put her on thyroid medication, and what a difference! We didn’t realize how sick she was until she started the medication. She began to play all the time and chased critters in the back yard like she had a new lease on life. She lost six pounds over the next few months and is now a happy, healthy dog.”
-Donnagan: From Friendly to Fear-Aggressive
Marion Westerling of Maryville, Tennessee, adopted Donnagan, a 7-year-old mixed breed, from a rescue organization in 2005, when he was seven weeks old. “For the first two years he was an absolute joy,” she says. “He went to training class, got along with everyone, and was a great dog. Then we introduced another dog into the house. We knew it might be a little tough, but we had no idea what was coming.”
Overnight Donnagan became aggressive, viciously attacking both of the family’s other dogs – and Westerling, when she tried to break up the fights. “He bit me four times,” she says, “once putting me in the hospital with a blood infection. Everyone, including my own vet, told me he was just a vicious dog and needed to be put down.”
But Westerling knew there was something wrong with Donnagan, and she kept looking for answers. Finally she found a veterinarian who listened to her and did some blood work. “Sure enough,” she says, “hypothyroidism. Donnagan continues to have anxiety and we watch for certain triggers, but since he went on thyroid medicine, he is a different dog. Six months ago we introduced another dog to the family and after a week, he accepted her and loves her.
“It’s frustrating to me,” she continues, “that so many vets are not listening to their clients. We know our dogs and know when something is wrong. Euthanasia is not always the best answer. I own a doggy daycare and hotel, and when I see a dog come in with a lot of fear aggression, I encourage the owner to take the dog to the vet for a health checkup, especially a thyroid check. I know because I’ve been there.”
-Tillie: A Giant Sheltie?
Laura Simcox of Louisville, Kentucky, adopted Tillie, a Sheltie, from the nearby Woodstock Animal Foundation. When Tillie was first picked up in September 2008, she weighed 62 pounds, more than twice her ideal weight (see “before” photo of Tillie on page 12). She was diagnosed as hypothyroid and put on medication.
Tillie was Simcox’s Christmas present in 2008. “At that time,” she says, “Tillie was down to 50 pounds and still had ear infections but her skin issues had mostly cleared up. Over the next year she ate a low-calorie kibble. In addition to thyroxine, my veterinarian also has her on gemmotherapy, and I add a few drops of the remedy called ‘bloodtwig dogberry’ to her food.”
The plant bud remedies used in gemmotherapy, whose manufacturing methods resemble those of homeopathy, are said to stimulate the body’s excretory organs and systems and promote detoxification. Holistic veterinarians who use gemmotherapy recommend bloodtwig dogberry for the thyroid, using it as an adjunct treatment for detoxifying and strengthening the thyroid gland.
Tillie gradually increased her exercise. “She had a great desire to play fetch,” says Simcox, “and she would waddle after my other two dogs as they chased balls. She lay down when she was tired and, as the weeks went by, longer periods elapsed before she had to rest.
“Today at 25 pounds, Tillie is a beautiful shadow of her former self. When we play fetch, I tire of the game long before she does. She has earned her Canine Good Citizen title, is training in agility, and is enrolled in a therapy dog class.”
Like the other dogs described here, Tillie (seen in her “after” photo on page 13) could be a poster dog for hypothyroidism – a dog whose health problems were easily resolved once they were properly diagnosed, and whose life was transformed in the process.
CJ Puotinen lives in Montana. She is the author of The Encyclopedia of Natural Pet Care and other books and a frequent contributor to WDJ.
Mary Straus is the owner of DogAware.com. She lives with her Norwich Terrier, Ella, in the San Francisco Bay Area.






