CANINE COMPLETE BLOOD COUNT OVERVIEW
1. Don’t hesitate to authorize repeated CBC tests. This will help track your dog’s response to disease and treatment. The cellular composition of a dog’s blood changes rapidly, so sequential tests will reveal more and more about his condition.
2. If your veterinarian has already gone beyond early screening for disease, and still needs definitive answers, insist that CBC tests are read at a commercial veterinary laboratory or vet college.
The complete blood count (CBC) is perhaps the most basic of all the diagnostic tools available. To do CBCs in-house, it takes only a few drops of blood from the patient, some specialized instruments that most veterinary clinics have on hand, and a modicum of practitioner skill.
I look at the CBC as the “great divider,” providing veterinarians with answers that help split our first impressions into either/or diagnostic scenarios. Sequential CBCs can often give us a handle on the progression of the disease and a reasonable assessment of prognosis. The CBC is also one of the easiest of the specialized diagnostic tools to interpret – but, as is true of every diagnostic or treatment tool, it is not without pitfalls if we don’t understand its limitations (see “What the CBC Can’t Do,” end of article).
Complete Blood Count Details
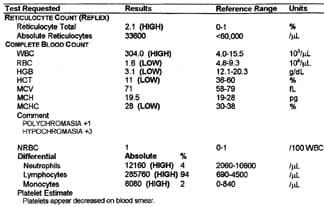
The CBC uses the various cellular components of the blood to help define the animal’s current state of health or disease. Leukocytes (white blood cells or WBCs) and erythrocytes (red blood cells or RBCs) are counted, and their total numbers, compared to normal values, are assessed. Thrombocytes (platelets) may also be counted, or they may be evaluated on the blood film and an estimate made for whether there are adequate numbers or not.
To start, a drop of blood is placed on a microscope slide and spread into a thin film. The film (or blood smear) is stained with a variety of substances that help accentuate cell structures for easy identification. Using the microscope, one hundred white cells are identified, and the percentage of each cell type is recorded. This percentage is multiplied by the total number of WBCs, and this absolute value of the cell type is compared to normal values.
It is a simple task to separate the major cell types of the blood into fractions because their relative mass differs substantially. In a tube that has been centrifuged (or left to settle for a few minutes), the red cells are found at the bottom of the tube, and the combination of white cells and platelets form a thin cap atop the red cells. The fluid portion (plasma or serum) makes up the remaining 50 – 60 percent of the volume of the blood. The plasma contains the enzymes and proteins that are evaluated in blood chemistry analyses, along with clotting and immune system factors and other components.
A quick look at the blood-filled centrifugation tube used for determining the hematocrit (also known as the packed cell volume or PCV) will also reveal dramatic increases in white blood cells, when the white “cap” atop the RBCs is more than a few millimeters deep. A look at the tube can also tell us if the serum is lipemic (contains excess fat, usually due to a non-fasting sample), or if there is serious liver damage (indicated by the yellowish tint that bilirubin imparts) or RBC breakdown in the blood (indicated by reddish serum).
Other red cell indices include MCV (mean corpuscular volume), MCH (mean corpuscular hemoglobin), and MCHC (mean corpuscular hemoglobin concentration). When using manual methods for CBC analyses, these indices are calculated from directly determined measurements (PCV, red cell count, and hemoglobin). Automated counters determine cell numbers, cell size (MCV), and hemoglobin concentration, and mathematically calculate the PCV, MCHC, and MCH. These red cell indices are used as an aid in categorizing or classifying anemias, and they can be helpful for monitoring the progress of the condition.
Bone marrow is the starting ground for all blood cells, so when we can’t find a reason for the lack of any one cell line, we may refer to a bone marrow analysis. For example, when a patient has a nonregenerative anemia with no apparent cause, we will need to take a bone marrow sample, stain and identify the cells, and see if there is an identifiable problem somewhere along the normal progression of cell production.
Red Blood Cell Abnormalities
The normal PCV in the adult dog is 37 – 55 percent, and the normal RBC count is 5.5 – 8.5 million cells per microliter of blood. Values that are significantly higher or lower than these send practitioners looking for further clues in certain directions, to wit:
• Fewer than normal RBCs
Low numbers of RBCs or a decreased (or low) PCV indicate anemia. Arbitrarily the severity of the anemia is indicated by the following PCV ranges:
Mild: 30 – 37 percent
Moderate: 20 – 29 percent
Severe: 13 – 20 percent, and
Very severe: less than 13 percent.
Transfusions are usually necessary when the PCV is less than 13 percent, but the severity of clinical signs is often directly correlated to the rapidity of onset of the anemia. That is, if the anemia has developed gradually, the animal may be better able to adapt to the loss of red cells than if there was sudden and massive blood loss.
With anemia, the first step is to determine whether it is regenerative or nonregenerative. Under normal conditions it takes about seven days for the bone marrow to produce a new supply of red cells. But when the marrow is forced to work faster than normal, it tends to send new, not-quite-mature red cells into the blood stream. These immature red cells are called “reticulocytes” or “polychromatic cells,” and they can be seen and counted on blood films by using special stains.
After we give the bone marrow some lag-time to respond (three to four days), a regenerative anemia will have adequate reticulocyte response; nonregenerative anemias will not. Healthy dogs have the capacity to produce a hefty reticulocyte response; in severe anemia, 20-50 percent of their red cells may be reticulocytes.
When an anemia is nonregenerative after three to five days, we may want to look into the cause by evaluating the bone marrow. But often we can get diagnostic clues just by looking at the morphology of the RBCs on a smear and linking their appearance to the most likely causes (see table below).
For example, when there is considerable variability with the RBCs’ size (aniso-cytosis), we can assume the bone marrow is producing young cells, as it should in regenerative anemia. (Younger RBCs are larger than more mature ones.) The presence of high numbers of spherocytes (RBCs that are smaller and rounder than normal) indicates the probability of an immune-system disorder that is attacking the RBCs. “Heinz bodies” indicate an oxidative, toxin-produced change within the RBC.
And of course, a definitive diagnosis is possible when we observe parasites on the blood film, including Haemobartonella canis, Babesia canis, Ehrlichia canis, Histoplasma capsulatum, Dipetalonema reconditum, and Dirofilaria immitis (heartworm).
• More than normal RBCs
An elevated PCV value (polycythemia) is most often the result of dehydration, although sometimes splenic contraction (from fear or excitement) may also cause an increased value. Increased plasma proteins also indicate dehydration, and the protein levels will return to normal upon rehydration.
Polycythemia may also occur when the body is asking for more oxygenation capacity – living at high altitudes, for example, or as a secondary condition related to lung disease. And, there are some rare neoplastic conditions that cause persistently elevated PCVs.
What White Blood Cells Do
Leukocytes (WBCs) are the body’s cellular line of defense, providing a formidable, first-line armamentarium for tracking, isolating, killing, and removing all sorts of invaders, so the WBC portion of the CBC is commonly used to detect and monitor inflammatory processes. WBCs also hold the key for creating and maintaining the body’s immune system function.
The WBCs include the following cell types: neutrophils, band cells (immature neutrophils), lymphocytes, monocytes, eosinophils, and basophils.
We first look at total response (total numbers of WBCs per microliter of blood), and then evaluate the current number values of each of the individual cell lines compared to normal values. Finally, we use these values to help give us the diagnostic category we will be working with to develop our therapeutic protocol.
Normal WBC values (including all white cell types) are 5,500 – 16,900 per microliter.
Neutrophils are usually the most prevalent WBC; in a healthy animal they comprise about 60 to 70 percent of the white cells. Typically, then, when we have increased WBCs, most of the increase will be due to neutrophils.
Neutrophils are thought of as the primary infection fighters of the body. They are attracted to pathogenic invaders – they actually have the capability to move toward the intruders – and they are able to engulf, kill, and remove all sorts of invaders. Normal neutrophil values are 3,000 – 12,000 per microliter. Neutrophils have a short life span (a few hours), so an evaluation of them is indeed a quick snapshot. However, since their turnover rate is so rapid, they offer a good monitoring tool for prognosis.
Bands are immature neutrophils, and they are released from the bone marrow whenever there is an increased need somewhere in the body. Normal band values are 0.0 – 299 per microliter.
Within hours, neutrophils respond to a wide variety of stimuli (including infections, tissue necrosis, and immune-mediated diseases) with the inflammatory response. The neutrophil response we observe in the blood represents a dynamic balance between the demand for WBCs at the site of the inflammation and the rate of bone marrow release.
As an example, a severe infection may initially deplete all the available WBCs, resulting in a decreased circulating number (neutropenia). Within hours, however, the bone marrow releases extra neutrophils, and within days is able to produce huge numbers of cells. As the bone marrow responds, it also releases increasing numbers of immature neutrophils (band cells). This process is referred to as leukocytosis with a left shift. So long as the production of cells stays ahead of the demand, there will be an orderly progression from a few immature forms to increasing percentages of more mature cells.
The magnitude of the neutrophilic response is an approximate reflection of the magnitude of the inflammatory response. Further, a localized inflammation, pyometra for example, elicits a greater neutrophil response than generalized inflammation. Some bacteria (pyogenic or fever-inducing bacteria, for example) stimulate a more intense neutrophil response than other types. Dogs have a tremendous capacity for neutrophilic response, and values of 50,000 per microliter or higher are not uncommon with these conditions.
The severity of the inflammatory process is reflected by the degree of the left shift – that is, when the number of band cells and even more immature cells increases greatly, we can assume there is a severe ongoing inflammatory response.
Lymphocytes are associated with immune function. They can become stimulated (reactive) with exposure to antigens (including those found in vaccines), and they carry a long-term memory that gives the immune system its capacity to respond to the antigens the body has been exposed to over a lifetime. Lymphocytes are also the cells most often involved in canine cancers. The normal values for lymphocytes are 1,000 – 4,900 per microliter.
Monocytes are thought of as the scavengers of the bloodstream, mopping up and eliminating the cells and debris of inflammation and infection. The normal values for monocytes are 100 – 1,400 per microliter.
Eosinophils respond to antigen stimulation as seen in many hypersensitive reactions. The normal values for eosinophils are 100 – 1,490 per microliter.
Basophils are a rare cellular component of blood. The “normal” value would be 0.
White Blood Cell Abnormalities
Values of any WBCs that are significantly higher or lower than normal values send practitioners looking for further clues in the following directions:
• More than normal WBCs
An elevation of total white cell numbers (leukocytosis) is usually from an increase in neutrophils, and it can be caused by several things:
Physiologic leukocytosis: Defined by an increase in mature neutrophils and sometimes lymphocyte numbers. It is epinephrine-induced and often due to the fear and struggling that occurs during restraint necessary for blood collection.
Corticosteroid-induced leukocytosis: Typically characterized by increased neutrophils (neutrophilia), decreased lymphocytes (lymphopenia), increased monocytes (monocytosis), and fewer eosinophils (eosinopenia). This reaction can be induced by exogenous (drug-induced) or endogenous (stress-related) factors. Note: These are specific and predictable alterations to the animal’s blood-borne line of defense, changes that occur whenever we choose to use corticosteroid therapy (or whenever the animal undergoes chronic or severe stress). These alterations are only a portion of the dramatic effects corticosteroid therapy has on the body, and to my mind represent one more reason to be very cautious when using this class of drugs.
• Fewer than normal neutrophils
Reduced numbers of neutrophils (neutropenia) can occur whenever there is an overwhelming bacterial infection and the increased tissue demand results in a depletion of the available neutrophils in the marrow. There are also several rather uncommon conditions in which the bone marrow is not capable of producing neutrophils in a normal manner, resulting in reduced numbers in the blood.
• More than normal lymphocytes
Lymphocytosis (increased numbers) may occur temporarily after vaccination or with increased exercise or anxiety. Lymphocytes may also increase with autoimmune disease and lymphosarcoma (cancer).
• Fewer than normal lymphocytes
Lymphopenia (decreased numbers) commonly occurs with excess glucocorticoids, whether they be from endogenous sources (stress, debilitating disease, surgery, shock, trauma, or exposure to heat or cold), or from exogenous sources (such as glucocorticoid therapy). Viral infections such as canine distemper, infectious canine hepatitis, parvovirus, and coronaviral enteritis also cause lymphopenia.
In addition, lymphopenia is expected in acute severe disease, and the return of the lymphocytes into the normal range is a good prognostic sign of decreasing stress. Finally, lymphocytes may be depleted with repeated drainage into a body cavity (chylothorax or protein losing enteropathies as examples).
• More than normal monocytes
Monocytosis (increased numbers) occurs along with inflammation and tissue necrosis, or glucocorticoid therapy.
• More than normal eosinophils
Conditions that typically cause eosinophilia (increased numbers) include parasitism and hypersensitivity reactions. Eosinophilia is also associated with carcinoma, lymphosarcoma, and other specific diseases such as eosinophilic enterocolitis or pneumonitis.
• Fewer than normal eosinophils
Eosinopenia (decreased numbers) occurs with an excess of either endogenous or exogenous corticosteroids, but since eosinophil numbers are so low in normal blood, this phenomena is rarely noticed.
• More than normal basophils
The number of basophils may increase (basophilia) with heartworm or hookworm infestation and with hypersensitivity reactions. With all these there is usually a concurrent eosinophilia. Hypothyroidism occasionally produces basophilia.
All About Thrombocytes
Thrombocytes (also known as platelets) are responsible for adequate clotting of the blood, and platelet problems are the most common cause of bleeding. Estimates of normal values can be done by an experienced technician by simply observing adequate numbers scattered throughout the blood film. Normal platelet values range from 200,000 – 500,000 per microliter.
• Fewer than normal thrombocytes
Severe thrombocytopenia is defined as fewer than 20,000 platelets per microliter, and it is at this value where we begin to see nose bleeding and hemorrhages into the skin and gut. Causes of thrombocytopenia include immune mediated diseases, improper production by the bone marrow, and consumption of platelets during intravascular coagulation (disseminated intravascular coagulation or DIC).
• Larger than normal thrombocytes
Large platelets indicate the possibility of immature cells being released by the bone marrow – perhaps due to increased need in the body.
Detecting Leukemia with the CBC
Leukemia is a progressive, malignant disease of the WBC or RBC bloodforming organs, with neoplastic cells evident in the peripheral blood and bone marrow. Leukemia is generally recognized by diagnosing high numbers of immature (blast) cells in the peripheral blood. Any of the cell lines may be involved, but the most common cell type is the lymphocyte (lymphocytic leukemia). Most cases of leukemia demonstrate elevated numbers of the involved cell type; rarely, the absolute numbers seen are actually decreased from normal.
Since dogs have such a dramatic capacity to elevate leukocyte numbers, it is often difficult to differentiate between leukemia and what is termed a leukemoid reaction – a strong and persistent leukocytosis without the presence of blast cells.
The most common neoplasia of the blood system of dogs is canine malignant lymphoma (lymphosarcoma, lymphocytic leukemia), with a reported incidence of 24:100,000. This is a progressive disease characterized by neoplastic transformation of lymphoid cells. The neoplasia may originate in either solid lymph organs (lymphosarcoma) or in the bone marrow (lymphocytic leukemia). Diagnosis is made, depending on the origin of the disease, by observing many swollen lymph nodes that can be huge, or by finding large numbers of abnormal lymphocytes on a blood film.
What the CBC Can’t Do
The first and foremost limitation that dog owners should recognize is that the CBC is only a snapshot of what is going on in the inner animal; it does not provide us a story with a beginning, middle, and end. To really know how a disease is progressing, we will need perhaps several progressive “snapshots,” each one giving us a better insight into the whole story of the dog’s ongoing health status.
We don’t often come up with a definitive diagnosis using only a CBC. Usually, it tells us how the body is responding or has responded to a generalized condition. For example, increased neutrophils (one of the white blood cells) indicate an inflammatory response. But the CBC does not tell us where in the body the inflammation is located or what has caused the inflammation, and it almost never helps us differentiate between specific diseases.
Another example: A decreased PCV (low numbers of red blood cells or RBCs) tells us only that we are dealing with anemia; it does not tell us whether the anemia is from poor production of RBCs or from blood loss. And, if the anemia is from blood loss, we still need to determine whether this is the result of a bleeding wound, blood loss into the intestine or other body cavity, parasitic infestation, immunologic conditions that directly attack red blood cells, or any other causes. Thus a CBC tells us only how the blood cells are responding to generalized diseases or conditions. It will not tell us anything about which specific organ system is affected; blood chemistries or other alternative diagnostic methods are needed for this step – to my way of thinking, a vital step for developing a holistic protocol for healing.
And, as with any diagnostic tool, the CBC needs to be interpreted in the context of the whole patient – relying on whole-body signs and symptoms – to put together the whole of the diagnosis. Again, as a holistic practitioner, I think veterinarians have the best chance for success when we combine several diagnostic methods, both Western and alternative.
There are a few variables that have a slight effect on the “normal ranges” of CBC parameters – for example, the dog’s age, sex, breed, and pregnancy status – and we need to keep these in mind when we interpret CBCs. But, for the most part, the normal ranges are well established, and these will remain basically the same between labs. Quality control is not as much a problem as it is for blood chemistries, but there are still some considerations to keep in mind (see below ).
Choose the Best Lab for the Job
Canine and human blood cells don’t all look the same on a stained blood smear, and technicians trained with human blood may not identify some cell lines as accurately as a veterinary technician would. Differentiating between monocytes and reactive lymphocytes seems to be a persistent problem, as does identifying immature neutrophils. Technicians trained in human medicine may not have the experience to identify specific canine diseases.
Further, the in-house stains commonly used by most vets are not as good as the stains used in commercial labs for identification of some cells or structures. Reticulocytes are RNA-rich cells that indicate the degree of response the animal is mounting to anemia. Special stains are needed to properly count the number of reticulocytes; poor staining technique (and/or poor technician training) may miss the presence of reticulocytes or miscount them.
Ultimately, quality control depends on the skills of the examiner, and some veterinarians (and/or the technicians in their hospitals) enjoy the art-forms of working with a microscope and using the methods required for counting, staining, and identifying blood cells, and they thus have developed the necessary skills to accurately assess CBCs. Other practitioners don’t have the requisite interest, and they either send their CBCs out, or the CBC becomes a neglected area in their diagnostic arsenal.
For the most part, these quality control issues are not critical – until we have gone beyond early screening and have reached a state in our diagnostic efforts where we need specific, definitive answers. At this stage, it is probably worthwhile to insist that the samples be read at a commercial veterinary laboratory or at the nearest veterinary college.
CBC Summary
The CBC is a quick and easy way to obtain information that helps separate diseases into categories, and provides some information as to the severity of the disease. Sequential CBCs can give us a reasonable idea for the progression and prognosis of the disease. As with all other tools in the practitioner’s tool kit, the CBC is only as good as the “practitioner-operator,” and good practitioners understand the tool’s limitations as well as its value.
Dr. Randy Kidd earned his DVM degree from Ohio State University and his Ph.D. in Pathology/Clinical Pathology from Kansas State University. A past president of the American Holistic Veterinary Medical Association, he’s author of Dr. Kidd’s Guide to Herbal Dog Care and Dr. Kidd’s Guide to Herbal Cat Care.





very informative. thank a lot.
Very informative. Thank you very much. Hope to learn more from you so as to save the life our dear pets.
Thanks a lot
Thanks. VERY HELPFUL W 7 YO F LEONBERGER
I have for months been trying to get my Vet to realize my Beautiful Male Pomeranian 4 years has dog lice which he has lost his hair & lost weight & going to get full blood panel but not sure she will still give me right diagnosis all she wants to do is suggest Revolution, but my 5lb pommy has seizures so I don’t want to give him a pesticide that might kill him. Do you have any suggestions?