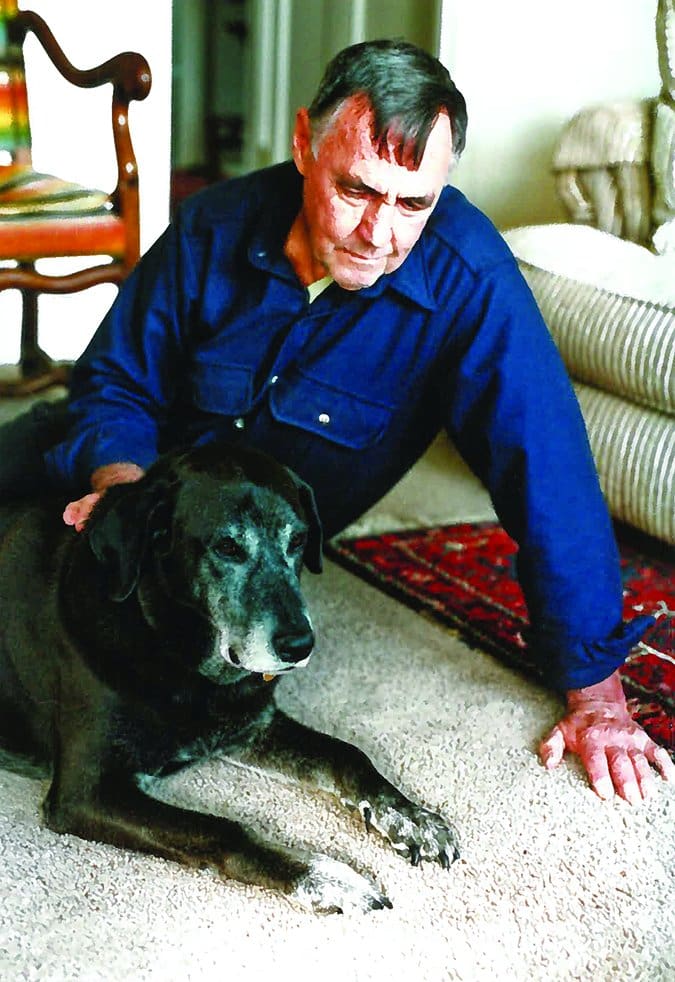
The final kindness we can do for beloved pets who are suffering from disease or painful effects of advanced age is to relieve and shorten their misery. Euthanasia should be painless and peaceful, giving a caregiver a last, loving embrace with her dog (or cat), and a memory of ending the pet’s life in a quiet, dignified, fear-free, trauma-free manner. Many of us are at our most vulnerable at this time, wracked with sadness and distracted with deep concern for our companions – and, unfortunately, this may cause us to fail to ensure that the end we want for our pets resembles our hopeful vision of a peaceful end in any way.
Twice in the past year I went to a veterinary hospital to have an animal companion euthanized. One was my 20-year-old cat, Yogi; the other was a beloved friend’s ancient, blind, deaf, Chihuahua, Hopper, whom I was fostering after my friend’s death. In each instance, I wanted a smooth transition from this life to the afterlife for these much-loved, suffering pets – and in each instance, I was horrified during the process by events that were out of my ability to foresee or control. That is, they were out of my control because I hadn’t foreseen them.
The stories were difficult to recount (they are described in “Pet Euthanasia Gone Wrong“), but as a tribute to these animals, who didn’t get the painless, peaceful end they were entitled to, I’d like to warn others about the things that can potentially go wrong during euthanasia. I want to stand at the edge of the world and scream, “No animal should suffer pain and terror at the end of her life during euthanasia, at the hands of a veterinarian!” Instead, I’ll try to turn my horrific story into an educational opportunity.
Look for Practitioners Dedicated to Fear- and Pain-Free Caregiving
There is no more appropriate time to engage the services of a practitioner trained in fear-free handling techniques than when it comes to euthanizing your pet. Fortunately, there are now at least three well-respected sources of education and certification for veterinarians and their staff (as wells as groomers, daycare providers, dog trainers, and other pet-care professionals) on the topic of handling animals in a way that does not cause them additional stress or pain.
Dr. Sophia Yin, a veterinarian with a special interest in animal behavior and positive reinforcement-based training, is widely credited with pioneering methods of safely handling animals for husbandry and veterinary purposes.
When Dr. Yin realized that more dogs were being euthanized because of behavioral issues than medical issues, she went back to school (after earning her doctorate in veterinary medicine in 1993). She earned a Masters degree in Animal Science in 2001 and started developing low-stress handling techniques in her veterinary behavior practice. She published a book about these methods, Low Stress Handling, in 2009.
After Dr. Yin’s death in 2014, her business partners continued her legacy by establishing a low-stress handling curriculum and certification for veterinarians, vet techs, and any other animal-care professionals who want to learn to handle companion animals with the least amount of stress and defensiveness possible.
Pets who are less stressed feel more at ease in a hospital, from the minute they walk through the door, throughout their examinations, until they leave. Several levels of Low Stress Handling Certification can be earned by veterinarians and their staff, as well as other animal-care professionals, through Dr. Yin’s legacy, Low Stress Handling University.
Another certification program designed to reduce stress in pets in a hospital environment is called Fear Free, which was founded by Dr. Marty Becker, a veterinarian with a practice in Idaho. Dr. Becker is also adjunct professor at several schools of veterinary medicine and has authored a number of popular books on animal health. Fear Free offers an ever-growing number of courses for veterinary-hospital staff on subjects that range from fear-free animal, transport, waiting rooms, examinations, and in-hospital protocols for sedation, anesthesia, and analgesia.
Individual Fear Free professional certification launched in early 2016. One of the next certifications that Dr. Becker plans to offer is called Compassion-First Pet Hospitals, wherein every aspect of a veterinary practice is designed with the animal patients’ emotional comfort as a priority.
Recently the American Animal Hospital Association (AAHA) began offering an online course in animal hospice and palliative care that includes euthanasia protocols that follow the Low Stress Handling and/or Fear Free philosophies. The certification program can be taken by veterinarians, vet techs, vet office staff, kennel workers, or anyone with an interest in this subject. See the AAHA web page for more information.
These are the only certification programs available to veterinary professionals. Courses in understanding companion animal behavior, body language, and the emotional state of pets were not taught in veterinary schools when Dr. Yin and Dr. Becker were students (I’m not aware of any veterinary schools that include this information in their curriculum even now), and both sought to address that educational void.
If you love your veterinarian, but you don’t think she is aware of these fear-free or low-stress handling educational resources, consider mentioning these certification programs the next time you and your dog see her. If she learned even a few tips on how to help pets be less anxious during vet visits, you’d all (client, patient, doctor, staff) be glad she did.
Confirm Your Vet’s Certification
It’s possible for a veterinarian to independently seek out advanced education and earn competence in animal behavior and low-stress handling techniques, just as Dr. Yin and Dr. Becker did. However, I learned the hard way that pet owners need to be vigilant and ask for confirmation of whatever “low stress” or “fear free” marketing claims are made by a veterinary practice.
As a dog trainer, body-language expert, former veterinary technician – and certified Fear Free Professional myself – I knew that I wanted a compassionate and trained veterinarian and staff to help facilitate a smooth, peaceful, and painless transition for my 20-year-old feline companion, Yogi. Having recently moved to a new area, I searched online for a veterinary hospital whose website referenced fear-free veterinary protocols. I was thrilled to find one about an hour away. The website had several mentions of fear-free visits and one whole page explaining how the practice owners made the hospital fear-free. When I called to make the appointment for Yogi, I asked whether they were versed in Fear Free protocols and was assured that they were.
But after not one but two traumatic euthanasia experiences at the hospital (see “Pet Euthanasia Gone Wrong“), I found myself wondering about how the practitioners could possibly have credentials of any kind in fear-free or low-stress handling. I looked at the website again – and was stunned to realize that the language on the website was all in lower-case; there were no logos indicating the practice had either Fear Free or Low Stress Handling certifications.
I next emailed the customer-service representative at Fear Free asking if this hospital or any staff member was certified by Fear Free. I received an email stating that no one in the hospital was certified and that a Fear Free representative would contact the hospital regarding the language on the practice’s website. Within a few short hours, the language on the hospital website was changed, and now references how the business strives to make its veterinary hospital experience “stress free.”
Lesson learned: Don’t fall for buzzwords. Ask for proof of training, certification, or independent study, and insist on making an appointment with only those individuals who received the training that you want your veterinarian and technician to have.
Pet Euthanasia Protocols
The veterinarian who euthanized my cat and my foster dog used the same drug, in the same way (intra-muscular injection) as a pre-euthanasia sedative. Both animals had a very strong adverse reaction to the injection of the drug; the injection traumatized them and their frenzied responses traumatized me.
The day after the second awful experience, I called the veterinary clinic and asked for the name of the pre-euthanasia drug that was used on my cat and dog.
The drug is called Telazol. It’s a mix of two other drugs, tiletamine and zolazepam. I called Zoetis, the company that makes the drug, detailing the reaction that my animals had. I wanted to find out if the drug had been used improperly, or if the reaction my pets had was typical.
The Zoetis representative told me that while Telazol is not contraindicated to use as a pre-euthanasia sedative, it’s not the drug’s intended primary purpose; its primary purpose is as an anesthetic on difficult-to-manage animals for short procedures such as wound management, not for a pre-sedation before euthanasia. In headline-size type, the Zoetis website says Telazol “Provides restraint or anesthesia for cats and restraint and analgesia for dogs undergoing minor procedures.”
I also learned that the drug can sting badly when administered intramuscularly (IM).
I posted my experience on a closed Facebook group for Fear Free Professionals and asked what drugs or combinations of drugs do they use for a painless, peaceful euthanasia. None of the veterinary professionals in the Fear Free group used this drug in the manner that this vet used it.
All the veterinarians who responded said they mixed Telazol with other drugs and administered it subcutaneously (under the skin, commonly referred to as “sub-q”) rather than IM, because it’s less painful that way. Some didn’t use this drug at all, preferring other drugs, such as the combination of xylazine and ketamine best known by its veterinary nickname, “pre-mix.” Several vets also noted that “pre-mix” can also sting when administered IM. When an animal is emaciated, or has very little muscle tissue (as in the case of many senior cats and dogs, including my two wards), these drugs can cause so much pain when administered IM, that many of these vets inject the drugs sub-q, instead.
The most important bit of information that I gathered is this: There is no single right way to administer a pre-sedation drug or drug cocktail to every animal, every time. Ideally, the veterinarian should take into consideration a number of factors:
- The patient’s species (cat, dog)
- The patient’s physiological condition (obese or thin; well-muscled or lacking adequate muscle tissue; good or poor circulation; etc.)
- The patient’s behavior (calm, or agitated and fearful)
In fact, if a veterinarian uses the exact same drug protocol on every single animal, or will tell you exactly what drug will be used over the phone (before seeing the animal), it’s a red flag; this is absolutely a case in which the veterinarian should see and assess the animal’s condition before deciding which drug or drug combination to use, and how it will be administered (intramuscularly or subcutaneously).
I understand that no practitioner can sedate and euthanize without causing pain or fear in every animal, every time. But now I also know that a skilled, caring practitioner should see and evaluate each animal as an individual, and customize the drugs used and the way they are administered for the unique needs of each animal.
Before Making an Appointment for Euthanasia, Ask These Questions
You will undoubtedly have a meeting with a veterinarian if your dog’s condition is such that you are considering euthanasia as an alternative to suffering for days or weeks from a condition that is slowly or painfully killing him. That’s the time to ask your veterinarian questions about her protocol for euthanasia and listen keenly to her answers; they will tell you if she’s the right vet to help you and your pet at this most sensitive time.
Suggested questions:
• Can I give my pet something at home, before our appointment, that will help with her anxiety about entering the clinic?
• Do you usually sedate dogs before euthanasia? If so, with what?
• What is your protocol for euthanasia?
• What drug or drugs do you use?
• How do you administer these drugs?
• I want to be with my pet the entire time; is that okay?
• What should I be prepared for?
• Will I have time to stay with my pet?
Things to listen for in the veterinarian’s answers:
• “Pat” answers that indicate a rigid protocol, such as, “We always use this drug; it’s the best one.”
• An ideal response would be, “We will access the condition of your pet on the day of euthanasia and then we’ll decide on the appropriate drugs at that time.”
• Patience and compassion, for your pet and you: Did it seem that the veterinarian really listened to your questions, or did you feel rushed?
If you don’t feel completely comfortable with the answers or conversation, it would be wise to look for another veterinarian.
Be advised that in some areas, there are practitioners who specialize in hospice and end-of-life care; also, many house-call veterinarians report that home euthanasia is a large part of their practice. One directory of these practitioners can be found at Lap of Love.
If one of these specialists is available in your area and you can afford it (they may charge considerably more than a general practitioner would for euthanizing your pet), I’d highly recommend their services. I have found veterinarians who do home euthanasia to be deeply caring and compassionate; most vets who offer this service do so out of a strong desire to offer a highly personalized, unrushed experience.
Until my most recent experiences, all of my pets have been euthanized at home. I would have gladly paid any price for this service, but there aren’t any of these practitioners where I live now.
Trust Your Gut
I teach my dog-training clients to listen to their gut when choosing a vet, groomer, trainer, or boarding facility; if something doesn’t feel right, I tell them, you must be prepared to walk out the door and find a more appropriate person for your beloved pet.
But I have to acknowledge how difficult it is to do this when you are emotionally vulnerable and bracing oneself for something as upsetting as euthanasia. I spent days before each appointment preparing for the fateful day of letting these beloved pets be free of their suffering; even when things happened that I was unhappy about, I didn’t stop the procedure and decline to go through with it at that time.
I wish I had the presence of mind to stop the procedure when I noticed that the vet didn’t touch or greet either one of my animal companions before injecting the sedative. I should have walked out the door right then and there.
Trust me: You don’t want your last memory of your dog to be him screaming in pain and panic. My friends suffered and all I can do today is help educate as many people as I can in their honor.
Trainer Jill Breitner has been training dogs since 1978 and is a body language expert. She is the developer of the Dog Decoder smartphone app, which helps people identify and “de-code” their dogs’ body language for a better understanding. She is also a certified Fear Free Professional and certified in Animal Behavior and Welfare. She lives on the west coast and uses Skype for dog training consultations all over the world.






I am facing this now and want to thank you for this article. I’ve never had an experience like yours and I don’t ever want to go through one. I have been fortunate in the past taking my dogs into a clinic to be put to rest without the trauma you talked about. My present Papillion is a very (very) fearful little girl every place except for her home. Dyna deserves to end her days with peace and dignity. After all, she is the boss over the Aussie and the Poodle! Even the cat respects her high position.
I was not aware of two euthanasia services available in my area. I have not called yet to see if either would be willing to make a fairly long drive out into the country or what would be the cost of their service. At least now I know what questions to ask when I call them. Your so unhappy experience will help me give my girl a more peaceful ending to her life. I thank you so much for that.
I posted my experience on the article about pet euthanasia gone wrong.
I’ve asked a couple vets after my experience what they thought could have happened and both told me when a dog has advanced heart disease it could cause poor circulation and delay the effects of the drugs that sedate and in my Yorkies case it was like the shot caused him to not be able to get enough oxygen because he already had congested heart so by the time he was sedated he was struggling for 15 minutes to breathe. It was horrible. I dont know if there was a way to have prevented this from happening. Maybe more medicine un shot? Maybe I waited too long before I decided to put him to sleep? I’ll never know. The only consolation I have is that I agree that it was still probably more peaceful than without any shot would have been.
I really appreciate your tip about asking for proof of training before letting someone euthanize your dog. My old chihuahua is not doing well, can barely walk or see anymore, which breaks my heart but I think it is time for her to go. My husband suggested that she be euthanized in our home so she can be relaxed, so I am glad I found this article to help me figure out what questions to ask and what to expect.
I put down my dog Hop in November. It was gut wrenching. He was blind and had started going deaf. The vet put an iv in his front leg, which was good, but then came in and said are you ready and reached across and put the sedative in his hind leg, harshly, and said I’ll be back in 5 minutes. My dog started trying to run backwards from the pain. I picked him up and sat on the couch and then he started struggling to breathe. He was miserable and scared and I knew it. Then he came back and after holding and rocking him, I put him on the blanket and right before the vet injected him, the tech accidentally bumped the syringe and he snapped. At that point I knew he was 100% aware. His body may have been sedated, but his mind was not. I was horrified and I wanted to just get it over with for him. He was suffering. The vet injected him and he was gone within a minute. He did not move at all. My heart was breaking. It’s been more than three months and I still am not all right. I am so sad and I feel that I betrayed him. I wish I had just waited one week and researched and thought about it more. But he could not walk, he could not see and now he could not hear. It’s been more than three months and I still am not all right. I am so sad and I feel that I betrayed him. I wish I had just waited one week and researched and thought about it more. It was time, but I made a mistake with the sedative. When I put down my cat at another vets office, he gave him a little bit of anesthetic before putting him to sleep. It seemed to go much better. Why give them a sedative if it does not sedate their mind? I wanted to share my experience and just encourage others to do your research and think twice before agreeing to that painful sedative shot in the leg. Why don’t they just give them anesthesia like they were going to clean their teeth? I don’t get it. Thank you for your posts. Your experience was strikingly similar to mine and it helped to know that I was not dreaming this. Thank you for spreading the word and for sharing.
Pure evil. PURE. why they hell are they doing that to our beloved pets. I just lost my dog and she definately hated the sedative shot. %10000 heart breaking.
Thank you for sharing. Unfortunately, I also had a similar experience with the at home process for my 18 year old cat. It has been over 4 months and I’m still haunted with guilt and trauma watching my best friend so scared in her final moments. I’m still trying to find ways of coping with it which is how I found this article. The only explanation I got was that the vet said she was so thin that she thought it probably stung more than it should of. I just trusted these vets have the most peaceful process in place but it sounds like they don’t. Thank you for your work to educate others so they don’t have to go through what we have. Wishing you lots of love and peace.
Thank you for this article, I just wish I’d seen it before scheduling what I thought would be a more humane in-home euthanasia for my poor dog. This was my second time having to put a dog to sleep and the screaming reaction she had to the sedative injection was a complete shock and is tearing me apart today.
This didn’t occur with my first dog 9 years ago in a vet clinic, and this vet, who just performs in-home euthanasia, did comment on my senior dog’s thinness upon her arrival. Despite this, she gave the injection as an IM shot and did not mention that it could be given SQ but may take longer to work. I was so horrified by her reaction and have been reliving it over and over. I hope my dog can forgive me and I have vowed to be a better advocate for my pet should I find myself in this position again. Bless you
Thank you so much for this information. I was traumatized by such an experience recently and I never ever want to experience that again. At least now I know what to ask.
I put my beloved 15 yr old yorkie Sam down yesterday with Lap of Love. I’m a wreck. He was in kidney failure , barely walk, going blind and barely ate, he was so weak. I loved this boy so much. I’m sorry I followed through with it. Vet showed up and I told her to go to backyard to blankets in the sun. I picked him up and held him with his head over my shoulder like a baby, all of 5 lbs. But as I walked around the corner of my home and saw her Sam must have sensed her presence. He turned his head toward her and howled twice ( for the first time ever) and started barking and snapping at the air. Very strange because he has never snapped in 15 yrs. I immediately stepped back and started to cry and held him in my lap. Did he sense the grim reaper??? she came over and put her hand near his face for him to sniff and he snapped at her. He has no teeth. I thought of canceling but moved forward. She gave injection into his but and e went nuts and started kicking and bucking and then settled down. After 15 min he was asleep or relaxed. She tried to start cath in his vein and could not do it. At this time I was balling and my daughter took over. Then I left for a minute before I fainted myself and asked is it given. She said, Yes. I said is he dead? She said , No, sorry his heart is still beating. I said, what?? I thought it was instant within a minute? She said, I had to inject it in his stomach so it will take longer like 15 min. It was the longest 15 min ever of my life. She said, not yet but its getting slower another 5 min maybe??? Finally his heart stopped. I guess. I wanted to puke. It was NOT stress free for Sam or for me. I’m an RN and I’m so sorry I didn’t just stop when he sensed something bad. He deserved soooo much more.
I am so sorry for this happening to you both. 😭 I’ve never heard of such horrific euthanasia in my life. I’ve put at least 8 animals down and never ever did any of them go through any trauma like that. I just wanted to say how sorry I am and please don’t blame yourself. It wasn’t anything you planned. Its terrible yes but your pet knows it was not you. 💞❤✌🙏
I want to first point out that I am so sorry for your loss and the traumatic way in which your beloved pet left this world. I recently went through the euthanization of my beloved girl Shyla, and I did not experience what you in fact had experienced. I had my girl euthanized at the University of Minnesota, small animal hospital after she could no longer breathe secondary to canine leukemia. I am a critical care nurse who recognized both drugs used to end Shyla’s suffering. The first was propofol, the second was ketamine. We were allowed to spend as much time with her as needed to make sure she knew we loved her and that she would live on in our lives. The Vet then came in at our request and administered a dose of propofol which sedated my girl at which time we were allowed a few more minutes to continue to love and kiss on her. The vet then administered the ketamine that would stop her heart which was quite abrupt. All was done by an intravenous line they had inserted in her hind leg, and when she came riding in on the red wagon to where we were waiting, she did not seem stressed at all and in fact, was happy to see us, which made allowing the vet to euthanize all the more difficult. Shyla was cremated by herself and she now sits with me everyday on my desk in my home office where I can feel her presence and hopefully she can feel mine. She will forever be loved in the hearts of those who knew her.
Just been through this with my cat at my home. She was sleeping peacefully in the sun and I asked the vet to inject her whilst she was calmly snoozing. It wasn’t a peaceful sedation for her, the same reaction of the worst screech I have ever heard her make as the sedative was injected, she ran off, retched violently then finally went unconscious but with tremors. It was terrible.
Then I took her outside and the vet had implied it would be a shot to the abdomen however this was not the case, it was several stabs with the syringe with ghastly blue liquid until he found her poor heart and injected it. I can only pray she felt nothing, whilst being poked around in her chest with the needle.
It was very traumatic for me and for her and I just hope that she was very quickly insensible. I feel like I murdered my cat and would not recommend euthanasia in this way. It seemed like an eternity for me but I hope it was just seconds for her. I will talk to a vet who is a friend and see if I can find out any information. This was just too cruel, for her and for me who has to live with witnessing my dearest little cat’s awful last moments.
I am so sorry you experienced this horror. Than you for sharing your experience. I have a similar experience with my beloved dog of 17 years. She was blind, suffered from severe anxiety, night wakings and was beginning to experience neurological issues. After long and painful debate, my family decided it was time to say goodbye. Our senior cat was euthanized many years ago after she experienced a rapid decline one weekend and stopped eating. Our experience with my cat was completely painless, which is why I was open to euthanasia.
Today’s experience with my dog was unimaginable. When my son and I entered the room, the technician explained the procedure would be painless. From the first pin prick, our poor dog was yelping in pain. This was not one yelp but multiple loud yelps. I cannot calculate how much time elapsed during that initial pin prick but it was excruciating to watch. She was yelping, growling and squirming in the technician’s arms. I expressed my concerns to the technician and shared my perspective that this certainly was not the experience we expected for Bon Bon. The technician could not give me any answer as to why this was happening. My son was visibly upset so I asked him to sit in the car. The technician and I spoke and I chose to remain outside as she delivered the final dosage of medication.
I do not know what sedative drug was issued first. I would not have thought to inquire as I assume the point of euthanasia is to be painless. I wrote a letter to the owner of the vet clinic to understand what happened.
Sending condolences to all who’ve experienced awful last moment’s with their beloved pets.
My dog didn’t have an adverse reaction the the sedation but it took him a while to absorb it. He was so dehydrated despite all of my efforts to syringe water to him the in days prior, that his absorption rate was simply slower. But what happened with the heart stopping medication breaks my heart as I write it. My dog Buckley began gasping, threw his head up toward me, as I sat legs wide open with him in the middle of them, his head coming into my chest, he began to yelp/squeal a loud and excruciating sound. It was awful. It lasted probably 3-5 seconds and then his body relaxed as I guided his head down and he let out one final breath. I will keep that with me forever as I tried to do the right thing… to give him peace and I’m so afraid that I gave him pain and terror. The vets tell me that this was a neurological response, that it was a brain stem reaction, but that he was unaware that he was creating this reaction… and I want to believe them. But I have been with my baby for 12 glorious years and I watched him and mended him after he was attacked by dogs on two separate occasions and not once did he ever make a sounds remotely resembling those noises. They were blood curdling. I have searched and searched and j can’t find anyone else who had a similar circumstance and I’m really afraid that Buckley wasn’t fully under when they released his life. I’m so afraid he went in pain and terrified vs feeling the warmth of my hug and the unending love that I had intended for him to feel.
Oh and this was an at home euthanasia so it was done on my couch, him in my arms, with his brother Charlie next to us.